Abstract
Purpose
The aim of this systematic review was to review studies that existed from 1993 to 2012 regarding antimicrobial treatment options of paediatric neurosurgical shunt.
Methods
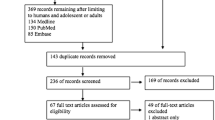
Studies were identified from MEDLINE, Scopus and Cochrane databases using a search strategy that was registered on the PROSPERO database. Studies were included if they had two or more patients, aged less than 18 years, and also specified the organism and antimicrobial treatment that was used.
Results
The search yielded 2,985 articles, and 76 articles were suitable for full review. In the final qualitative analysis, only eight studies were included, involving 86 participants. The most common antimicrobial regimens for Gram-positive infections was intravenous and intrathecal vancomycin (n = 7), followed by intravenous vancomycin monotherapy.
Conclusion
This systematic review has shown that there are no prospective randomised studies of antimicrobial treatment options for paediatric neurosurgical patients in the last 20 years, and larger prospective studies are urgently required for this serious infection. There is some limited case series showing the benefits of certain antimicrobials such as vancomycin and ceftriaxone, but a larger case series or randomised controlled trial is required, particularly to establish the benefit, if any, of additional intraventricular antimicrobials.

Similar content being viewed by others
References
Klimo P Jr, Thompson CJ, Ragel BT, Boop FA (2011) Antibiotic-impregnated shunt systems versus standard shunt systems: a meta- and cost-savings analysis. J Neurosurg Pediatr 8:600–612
Rosenthal VD, Richtmann R, Singh S, Apisarnthanarak A, Kubler A, Viet-Hung N, Ramirez-Wong FM, Portillo-Gallo JH, Toscani J, Gikas A, Duenas L, El-Kholy A, Ghazal S, Fisher D, Mitrev Z, Gamar-Elanbya MO, Kanj SS, Arreza-Galapia Y, Leblebicioglu H, Hlinkova S, Memon BA, Guanche-Garcell H, Gurskis V, Alvarez-Moreno C, Barkat A, Mejia N, Rojas-Bonilla M, Ristic G, Raka L, Yuet-Meng C (2013) Surgical site infections, International Nosocomial Infection Control Consortium (INICC) report, data summary of 30 countries, 2005–2010. Infect Control Hosp Epidemiol 34:597–604
Working Party on the Use of Antibiotics in Neurosurgery of the British Society for Antimicrobial Chemotherapy (1995) Treatment of infections associated with shunting for hydrocephalus. Br J Hosp Med 53:368–373
Huttova M, Freybergh PF, Rudinsky B, Sramka M, Kisac P, Bauer F, Ondrusova A (2007) Postsurgical meningitis caused by Acinetobacter baumannii associated with high mortality. Neuro Endocrinol Lett 28(Suppl 2):15–16
Khan FY, Abukhattab M, Baager K (2012) Nosocomial postneurosurgical Acinetobacter baumannii meningitis: a retrospective study of six cases admitted to Hamad General Hospital, Qatar. J Hosp Infect 80:176–179
Paramythiotou E, Karakitsos D, Aggelopoulou H, Sioutos P, Samonis G, Karabinis A (2007) Post-surgical meningitis due to multiresistant Acinetobacter baumannii. Effective treatment with intravenous and/or intraventricular colistin and therapeutic dilemmas. Med Mal Infect 37:124–125
Tuon FF, Penteado-Filho SR, Amarante D, Andrade MA, Borba LA (2010) Mortality rate in patients with nosocomial Acinetobacter meningitis from a Brazilian hospital. Braz J Infect Dis 14:437–440
Conen A, Walti LN, Merlo A, Fluckiger U, Battegay M, Trampuz A (2008) Characteristics and treatment outcome of cerebrospinal fluid shunt-associated infections in adults: a retrospective analysis over an 11-year period. Clin Infect Dis 47:73–82
Lee JK, Seok JY, Lee JH, Choi EH, Phi JH, Kim SK, Wang KC, Lee HJ (2012) Incidence and risk factors of ventriculoperitoneal shunt infections in children: a study of 333 consecutive shunts in 6 years. J Korean Med Sci 27:1563–1568
Turgut M, Alabaz D, Erbey F, Kocabas E, Erman T, Alhan E, Aksaray N (2005) Cerebrospinal fluid shunt infections in children. Pediatr Neurosurg 41:131–136
James HE, Bradley JS (2008) Aggressive management of shunt infection: combined intravenous and intraventricular antibiotic therapy for twelve or less days. Pediatr Neurosurg 44:104–111
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 62:1006–1012
Krcmery V Jr, Filka J, Uher J, Kurak H, Sagat T, Tuharsky J, Novak I, Urbanova T, Kralinsky K, Mateicka F, Krcmeryova T, Jurga L, Sulcova M, Stencl J, Krupova I (1999) Ciprofloxacin in treatment of nosocomial meningitis in neonates and in infants: report of 12 cases and review. Diagn Microbiol Infect Dis 35:75–80
Yilmaz A, Dalgic N, Musluman M, Sancar M, Colak I, Aydin Y (2010) Linezolid treatment of shunt-related cerebrospinal fluid infections in children. J Neurosurg Pediatr 5:443–448
Arnell K, Enblad P, Wester T, Sjolin J (2007) Treatment of cerebrospinal fluid shunt infections in children using systemic and intraventricular antibiotic therapy in combination with externalization of the ventricular catheter: efficacy in 34 consecutively treated infections. J Neurosurg 107:213–219
Stamos JK, Kaufman BA, Yogev R (1993) Ventriculoperitoneal shunt infections with gram-negative bacteria. Neurosurgery 33:858–862
Kralinsky K, Svetlansky I, Kovacicova G, Filka J, Huttova M, Krcmery V Jr (2000) Nosocomial meningitis due to Pseudomonas aeruginosa in children. J Chemother 12:538–539
Kim YK, Shin HJ, Kim YJ (2012) A fifteen-year epidemiological study of ventriculoperitoneal shunt infections in pediatric patients: A single center experience. Korean J Pediatr Infect Dis 19:141–148
Jourdan C, Convert J, Peloux A, Boussaid O, Grando J, Tigaud S (1996) Successful CSF penetration of continuous teicoplanin infusion after failure of continuous vancomycin infusion in three cases of shunt associated meningitis. [Diffusion intrathecale efficace de la teicoplanine apres echec de la vancomycine, administrees en perfusion continue, dans trois cas de meningite sur shunt]. Pathol Biol 44:389–392
Michelone G, Barasolo G, Dei Cas A, Vizzi T, Caselli D, Maccabruni A (1999) Ventriculitis in patients with DVP: clinical and therapeutical considerations in a pediatric cohort. [Ventriculite infettiva in portatori di shunt ventricolo-peritoneale: considerazioni cliniche e terapeutiche su una casistica pediatrica]. Riv Ital di Pediatr 25:873–878
Acknowledgments
RD would like to thank the staff of Alder Hey Hospital library for their assistance in sourcing some of the publications.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary digital content Table 1
Title: PRISMA Checklist. Description: This table gives a checklist of the items that should be covered as part of the systematic review. It details the page on which the item is covered in the manuscript (DOC 63 kb)
Supplementary digital content Table 2
Title: List of cases included in the systematic review. Description: This table gives the full details of all the cases included in this systematic review and gives the key parameters that were extracted from the papers (DOCX 40 kb)
Rights and permissions
About this article
Cite this article
Drew, R.J., Cole, T.S., Lee, M.K. et al. Antimicrobial treatment options for neurosurgical ventricular shunt infections in children from 1993 to 2012: a systematic review. Childs Nerv Syst 30, 841–850 (2014). https://doi.org/10.1007/s00381-013-2333-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-013-2333-z