Abstract
Objectives
To establish a diagnostic tree analysis (DTA) model based on ultrasonography (US) findings and clinical characteristics for differential diagnosis of common causes of cervical lymphadenopathy in children.
Methods
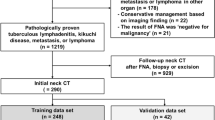
A total of 242 patients (131 boys, 111 girls; mean age, 11.2 ± 0.3 years; range, 1 month–18 years) with pathologically confirmed Kikuchi disease (n = 127), reactive hyperplasia (n = 64), lymphoma (n = 24), or suppurative lymphadenitis (n = 27) who underwent neck US were included. US images were retrospectively reviewed to assess lymph node (LN) characteristics, and clinical information was collected from patient records. DTA models were created using a classification and regression tree algorithm on the basis of US imaging and clinical findings. The patients were randomly divided into training (70%, 170/242) and validation (30%, 72/242) datasets to assess the diagnostic performance of the DTA models.
Results
In the DTA model based on all predictors, perinodal fat hyperechogenicity, LN echogenicity, and short diameter of the largest LN were significant predictors for differential diagnosis of cervical lymphadenopathy (overall accuracy, 85.3% and 83.3% in the training and validation datasets). In the model based on categorical parameters alone, perinodal fat hyperechogenicity, LN echogenicity, and loss of fatty hilum were significant predictors (overall accuracy, 84.7% and 86.1% in the training and validation datasets).
Conclusions
Perinodal fat hyperechogenicity, heterogeneous echotexture, short diameter of the largest LN, and loss of fatty hilum were significant US findings in the DTA for differential diagnosis of cervical lymphadenopathy in children.
Key Points
• Diagnostic tree analysis model based on ultrasonography and clinical findings would be helpful in differential diagnosis of pediatric cervical lymphadenopathy.
• Significant predictors were perinodal fat hyperechogenicity, heterogeneous echotexture, short diameter of the largest LN, and loss of fatty hilum.




Similar content being viewed by others
Abbreviations
- CART:
-
Classification and regression tree
- CNB:
-
Core needle biopsy
- CRP:
-
C-reactive protein
- CT:
-
Computed tomography
- DTA:
-
Decision tree analysis
- ESR:
-
Erythrocyte sedimentation rate
- FNA:
-
Fine needle aspiration
- ICC:
-
Interclass correlation coefficient
- LD:
-
Long diameter
- LN:
-
Lymph node
- PACS:
-
Picture archival and communication system
- SD:
-
Short diameter
- US:
-
Ultrasonography
- WBC:
-
White blood cell count
References
Park YW (1995) Evaluation of neck masses in children. Am Fam Physician 51:1904–1912
Bozlak S, Varkal MA, Yildiz I et al (2016) Cervical lymphadenopathies in children: a prospective clinical cohort study. Int J Pediatr Otorhinolaryngol 82:81–87
Deosthali A, Donches K, DelVecchio M, Aronoff S (2019) Etiologies of pediatric cervical lymphadenopathy: a systematic review of 2687 subjects. Glob Pediatr Health 6:2333794X19865440
De Corti F, Cecchetto G, Vendraminelli R, Mognato G (2014) Fine-needle aspiration cytology in children with superficial lymphadenopathy. Pediatr Med Chir 36:80–82
Gwili N, Abdel-Hadi M, Nour-Eldin A et al (2014) Lymphadenopathy in a series of Egyptian pediatric patients and the role of pathology in the diagnostic workup. Pediatr Dev Pathol. https://doi.org/10.2350/14-05-1480-oa.1
Sarsu SB, Sahin K (2016) A retrospective evaluation of lymphadenopathy in children in a single center's experience. J Pak Med Assoc 66:654–657
Lee EJ, Lee HS, Park JE, Hwang JS (2018) Association Kikuchi disease with Hashimoto thyroiditis: a case report and literature review. Ann Pediatr Endocrinol Metab 23:99–102
Lee K-Y, Yeon Y-H, Lee B-C (2004) Kikuchi-Fujimoto disease with prolonged fever in children. Pediatrics 114:e752
Chiappini E, Camaioni A, Benazzo M et al (2015) Development of an algorithm for the management of cervical lymphadenopathy in children: consensus of the Italian Society of Preventive and Social Pediatrics, jointly with the Italian Society of Pediatric Infectious Diseases and the Italian Society of Pediatric Otorhinolaryngology. Expert Rev Anti Infect Ther 13:1–11
Aulino JM, Kirsch CFE, Burns J et al (2019) ACR appropriateness criteria((R)) neck mass-adenopathy. J Am Coll Radiol 16:S150–s160
Ghafoori M, Azizian A, Pourrajabi Z, Vaseghi H (2015) Sonographic evaluation of cervical lymphadenopathy; comparison of metastatic and reactive lymph nodes in patients with head and neck squamous cell carcinoma using gray scale and Doppler techniques. Iran J Radiol 12:e11044
Nozaki T, Morita Y, Hasegawa D et al (2016) Cervical ultrasound and computed tomography of Kawasaki disease: comparison with lymphadenitis. Pediatr Int 58:1146–1152
Ryoo I, Suh S, Lee YH, Seo HS, Seol HY (2015) Comparison of ultrasonographic findings of biopsy-proven tuberculous lymphadenitis and Kikuchi disease. Korean J Radiol 16:767–775
Strassen U, Geisweid C, Hofauer B, Knopf A (2018) Sonographic differentiation between lymphatic and metastatic diseases in cervical lymphadenopathy. Laryngoscope 128:859–863
Dogan S, Yildirim A, Erbakirci R et al (2016) The role of ultrasonography for differentiating and management of malignant cervical lymph nodes. Eur J Gen Med 13:7–15
Ahuja AT, Ying M (2005) Sonographic evaluation of cervical lymph nodes. AJR Am J Roentgenol 184:1691–1699
Khanna R, Sharma AD, Khanna S, Kumar M, Shukla RC (2011) Usefulness of ultrasonography for the evaluation of cervical lymphadenopathy. World J Surg Oncol 9:29–29
You SH, Kim B, Yang KS, Kim BK (2019) Cervical necrotic lymphadenopathy: a diagnostic tree analysis model based on CT and clinical findings. Eur Radiol 29:5635–5645
Baek HJ, Lee JH, Lim HK, Lee HY, Baek JH (2014) Diagnostic accuracy of the clinical and CT findings for differentiating Kikuchi's disease and tuberculous lymphadenitis presenting with cervical lymphadenopathy. Jpn J Radiol 32:637–643
Kwon SY, Kim TK, Kim YS, Lee KY, Lee NJ, Seol HY (2004) CT findings in Kikuchi disease: analysis of 96 cases. AJNR Am J Neuroradiol 25:1099–1102
Lee S, Yoo JH, Lee SW (2012) Kikuchi disease: differentiation from tuberculous lymphadenitis based on patterns of nodal necrosis on CT. AJNR Am J Neuroradiol 33:135–140
Kim JY, Lee H, Yun BL (2017) Ultrasonographic findings of Kikuchi cervical lymphadenopathy in children. Ultrasonography 36:66–70
Lee MH, Lee SW, Kang BC (1999) Ultrasonographic evaluation of suppurative cervical lymphadenitis in children : focusing on abscess formation. J Korean Soc Med Ultrasound 18:313–318
Lo WC, Chang WC, Lin YC, Hsu YP, Liao LJ (2012) Ultrasonographic differentiation between Kikuchi's disease and lymphoma in patients with cervical lymphadenopathy. Eur J Radiol 81:1817–1820
Onciu M, Medeiros LJ (2003) Kikuchi-Fujimoto lymphadenitis. Adv Anat Pathol 10:204–211
Yoo JL, Suh SI, Lee YH et al (2011) Gray scale and power Doppler study of biopsy-proven Kikuchi disease. J Ultrasound Med 30:957–963
Marcy SM (1985) Cervical adenitis. Pediatr Infect Dis 4:S23–S26
Schwetschenau E, Kelley DJ (2002) The adult neck mass. Am Fam Physician 66:831–838
Hernandez M, Chowdhury R, Woods J, Cabrera J, Hardigan PC (2011) Management of suppurative cervical lymphadenitis in a healthy 24-year-old man. J Am Osteopath Assoc 111:49–51
Kikuchi M (1972) Lymphadenitis showing focal reticulum cell hyperplasia with nuclear debris and phagocytes: a clinicopathological study. Acta Haematol Jpn 35:379–380
Kuo TT (1995) Kikuchi's disease (histiocytic necrotizing lymphadenitis). A clinicopathologic study of 79 cases with an analysis of histologic subtypes, immunohistology, and DNA ploidy. Am J Surg Pathol 19:798–809
Perry AM, Choi SM (2018) Kikuchi-Fujimoto disease: a review. Arch Pathol Lab Med 142:1341–1346
Ahuja A, Ying M, Yang WT, Evans R, King W, Metreweli C (1996) The use of sonography in differentiating cervical lymphomatous lymph nodes from cervical metastatic lymph nodes. Clin Radiol 51:186–190
Ishii J, Fujii E, Suzuki H, Shinozuka K, Kawase N, Amagasa T (1992) Ultrasonic diagnosis of oral and neck malignant lymphoma. Bull Tokyo Med Dent Univ 39:63–69
Bruneton JN, Normand F, Balu-Maestro C et al (1987) Lymphomatous superficial lymph nodes: US detection. Radiology 165:233–235
Ying M, Ahuja A, Brook F, Brown B, Metreweli C (1996) Sonographic appearance and distribution of normal cervical lymph nodes in a Chinese population. J Ultrasound Med 15:431–436
Leboulleux S, Girard E, Rose M et al (2007) Ultrasound criteria of malignancy for cervical lymph nodes in patients followed up for differentiated thyroid cancer. J Clin Endocrinol Metab 92:3590–3594
Ganeshalingam S, Koh DM (2009) Nodal staging. Cancer Imaging 9:104–111
Ferrer R (1998) Lymphadenopathy: differential diagnosis and evaluation. Am Fam Physician 58:1313–1320
Libman H (1987) Generalized lymphadenopathy. J Gen Intern Med 2:48–58
Morland B (1995) Lymphadenopathy. Arch Dis Child 73:476–479
Slap GB, Brooks JS, Schwartz JS (1984) When to perform biopsies of enlarged peripheral lymph nodes in young patients. JAMA 252:1321–1326
Citak EC, Koku N, Demirci M, Tanyeri B, Deniz H (2011) A retrospective chart review of evaluation of the cervical lymphadenopathies in children. Auris Nasus Larynx 38:618–621
Giovanni JE, Dowd MD, Kennedy C, Michael JG (2011) Interexaminer agreement in physical examination for children with suspected soft tissue abscesses. Pediatr Emerg Care 27:475–478
Yen K, Karpas A, Pinkerton HJ, Gorelick MH (2005) Interexaminer reliability in physical examination of pediatric patients with abdominal pain. Arch Pediatr Adolesc Med 159:373–376
Marin JR, Bilker W, Lautenbach E, Alpern ER (2010) Reliability of clinical examinations for pediatric skin and soft-tissue infections. Pediatrics 126:925–930
Funding
This study has received funding by Seoul National University College of Medicine Education Research Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Young Jin Ryu.
Conflict of interest
The authors declare that they have no competing interests.
Statistics and biometry
The Division of Statistics in the Medical Research Collaborating Center at Seoul National University Bundang Hospital kindly provided statistical advice for this manuscript.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• Retrospective
• Case-control study
• Performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 8363 kb)
Rights and permissions
About this article
Cite this article
Park, J.E., Ryu, Y.J., Kim, J.Y. et al. Cervical lymphadenopathy in children: a diagnostic tree analysis model based on ultrasonographic and clinical findings. Eur Radiol 30, 4475–4485 (2020). https://doi.org/10.1007/s00330-020-06794-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-020-06794-w