Abstract
Background
Antiplatelet agents given to prevent thromboembolic disease are frequently withdrawn prior to surgical procedures to reduce bleeding complications. This action may expose patients to increased thromboembolic morbidity and mortality.
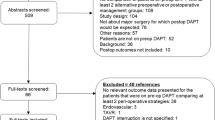
Methods
A series of 2012 patients who had undergone gastroenterologic surgery between January 2005 and June 2010 at our institution were reviewed. Among this cohort, antiplatelet therapy (APT) was used in 519 patients (25.8 %). The perioperative management included interruption of APT 1 week before surgery and early postoperative reinstitution in patients at low thromboembolic risk, although APT was maintained until surgery in those at high thromboembolic risk. Bleeding and thromboembolic complications, as well as other outcome variables, were assessed in patients with and without APT.
Results
Among 519 patients with APT, 99 (19.1 %) underwent multidrug APT. Among them, 124 (23.9 %) required preoperative continuation of APT. None suffered from excessive bleeding intraoperatively. There were 19 thromboembolic events (0.9 %) in the whole cohort. Postoperative bleeding complications occurred in 37 patients (1.8 %). Multivariate analysis showed that increased postoperative bleeding complications were independently associated with multidrug APT [hazard ratio (HR) 4.3, p = 0.014], high-risk surgical procedures (HR 3.5, p = 0.003), and perioperative heparin bridging (HR 2.8, p = 0.029). High-risk surgery (HR 8.3, p < 0.001) and poor performance status (HR 4.9, p = 0.005)—but neither APT nor anticoagulation use—were significant prognostic factors for thromboembolic complications.
Conclusions
Satisfactory outcomes were obtained during gastroenterologic surgery under rigorous perioperative management, including single-agent APT continuation in patients at high thromboembolic risk. Patients treated with multidrug APT still represent a challenging group, however, and need to be carefully managed to prevent perioperative complications.


Similar content being viewed by others
References
Cattaneo M (2004) Aspirin and clopidogrel: efficacy, safety, and the issue of drug resistance. Arterioscler Thromb Vasc Biol 24:1980–1987
Chassot PG, Delabays A, Spahn DR (2007) Perioperative use of anti-platelet drugs. Best Pract Res Clin Anaesthesiol 21:241–256
Grines CL, Bonow RO, Casey DE Jr et al (2007) Prevention of premature discontinuation of dual antiplatelet therapy in patients with coronary artery stents: a science advisory from the American Heart Association, American College of Cardiology, Society for Cardiovascular Angiography and Interventions, American College of Surgeons, and American Dental Association, with representation from the American College of Physicians. Circulation 115:813–818
King SB 3rd, Smith SC Jr, Hirshfeld JW Jr et al (2008) 2007 Focused update of the ACC/AHA/SCAI 2005 guideline update for percutaneous coronary intervention: a report of the American College of Cardiology/American Heart Association Task Force on Practice guidelines. J Am Coll Cardiol 51:172–209
Hermiz S, Larsen P, Galletly DC et al (2009) Peri-operative management of anti-platelet agents. ANZ J Surg 79:521–525
Fujikawa T, Tanaka A, Abe T et al (2013) Does antiplatelet therapy affect outcomes of patients receiving abdominal laparoscopic surgery? Lessons from more than 1,000 laparoscopic operations in a single tertiary referral hospital. J Am Coll Surg 217:1044–1053
Sorensen JB, Klee M, Palshof T et al (1993) Performance status assessment in cancer patients: an inter-observer variability study. Br J Cancer 67:773–775
Eagle KA, Berger PB, Calkins H et al (2002) ACC/AHA guideline update for perioperative cardiovascular evaluation for noncardiac surgery: executive summary a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1996 Guidelines on Perioperative Cardiovascular Evaluation for Noncardiac Surgery). Circulation 105:1257–1267
Eagle KA, Rihal CS, Mickel MC et al (1997) Cardiac risk of noncardiac surgery: influence of coronary disease and type of surgery in 3368 operations: CASS Investigators and University of Michigan Heart Care Program—Coronary Artery Surgery Study. Circulation 96:1882–1887
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Fujikawa T, Maekawa H, Shiraishi K, et al (2012) Successful resection of complicated bleeding arteriovenous malformation of the jejunum in patients starting dual-antiplatelet therapy just after implanting a drug-eluting coronary stent. BMJ Case Rep doi: 10.1136/bcr-2012-006779
Fujikawa T, Noda T, Tada S, et al (2013) Intractable intraoperative bleeding requiring platelet transfusion during emergent cholecystectomy in a patient with dual antiplatelet therapy after drug-eluting coronary stent implantation (with video). BMJ Case Rep. doi: 10.1136/bcr-2013-008948
Mita K, Ito H, Murabayashi R et al (2012) Postoperative bleeding complications after gastric cancer surgery in patients receiving anticoagulation and/or antiplatelet agents. Ann Surg Oncol 19:3745–3752
Thachil J, Gatt A, Martlew V (2008) Management of surgical patients receiving anticoagulation and antiplatelet agents. Br J Surg 95:1437–1448
Broad L, Lee T, Conroy M et al (2007) Successful management of patients with a drug-eluting coronary stent presenting for elective, non-cardiac surgery. Br J Anaesth 98:19–22
Kaluza GL, Joseph J, Lee JR et al (2000) Catastrophic outcomes of noncardiac surgery soon after coronary stenting. J Am Coll Cardiol 35:1288–1294
Nasser M, Kapeliovich M, Markiewicz W (2005) Late thrombosis of sirolimus-eluting stents following noncardiac surgery. Catheter Cardiovasc Interv 65:516–519
Wilson SH, Fasseas P, Orford JL et al (2003) Clinical outcome of patients undergoing non-cardiac surgery in the two months following coronary stenting. J Am Coll Cardiol 42:234–240
Kimchi NA, Broide E, Scapa E et al (2007) Antiplatelet therapy and the risk of bleeding induced by gastrointestinal endoscopic procedures: a systematic review of the literature and recommendations. Digestion 75:36–45
Nuttall GA, Santrach PJ, Oliver WC Jr et al (1996) The predictors of red cell transfusions in total hip arthroplasties. Transfusion 36:144–149
Palmer JD, Sparrow OC, Iannotti F (1994) Postoperative hematoma: a 5-year survey and identification of avoidable risk factors. Neurosurgery 35:1061–1064, discussion 1064–1065
Vasudeva P, Goel A, Sengottayan VK et al (2009) Antiplatelet drugs and the perioperative period: what every urologist needs to know. Indian J Urol 25:296–301
Chechik O, Inbar R, Danino B et al (2011) Anti-platelet therapy: no association with increased blood loss in patients undergoing open or laparoscopic appendectomy. Isr Med Assoc J 13:342–344
Cahill RA, McGreal GT, Crowe BH, et al (2005) Duration of increased bleeding tendency after cessation of aspirin therapy. J Am Coll Surg 200:564–573, quiz A559–A561
Komatsu T, Tamai Y, Takami H et al (2005) Study for determination of the optimal cessation period of therapy with anti-platelet agents prior to invasive endoscopic procedures. J Gastroenterol 40:698–707
Weber AA, Braun M, Hohlfeld T et al (2001) Recovery of platelet function after discontinuation of clopidogrel treatment in healthy volunteers. Br J Clin Pharmacol 52:333–336
Burger W, Chemnitius JM, Kneissl GD et al (2005) Low-dose aspirin for secondary cardiovascular prevention: cardiovascular risks after its perioperative withdrawal versus bleeding risks with its continuation—review and meta-analysis. J Intern Med 257:399–414
Dacey LJ, Munoz JJ, Johnson ER et al (2000) Effect of preoperative aspirin use on mortality in coronary artery bypass grafting patients. Ann Thorac Surg 70:1986–1990
Yusuf S, Zhao F, Mehta SR et al (2001) Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST-segment elevation. N Engl J Med 345:494–502
Artang R, Dieter RS (2007) Analysis of 36 reported cases of late thrombosis in drug-eluting stents placed in coronary arteries. Am J Cardiol 99:1039–1043
De la Torre-Hernandez JM, Alfonso F, Hernandez F et al (2008) Drug-eluting stent thrombosis: results from the multicenter Spanish registry ESTROFA (Estudio ESpanol sobre TROmbosis de stents FArmacoactivos). J Am Coll Cardiol 51:986–990
Eisenstein EL, Anstrom KJ, Kong DF et al (2007) Clopidogrel use and long-term clinical outcomes after drug-eluting stent implantation. JAMA 297:159–168
Iakovou I, Schmidt T, Bonizzoni E et al (2005) Incidence, predictors, and outcome of thrombosis after successful implantation of drug-eluting stents. JAMA 293:2126–2130
Kimura T, Morimoto T, Nakagawa Y et al (2009) Antiplatelet therapy and stent thrombosis after sirolimus-eluting stent implantation. Circulation 119:987–995
Park DW, Park SW, Park KH et al (2006) Frequency of and risk factors for stent thrombosis after drug-eluting stent implantation during long-term follow-up. Am J Cardiol 98:352–356
Spertus JA, Kettelkamp R, Vance C et al (2006) Prevalence, predictors, and outcomes of premature discontinuation of thienopyridine therapy after drug-eluting stent placement: results from the PREMIER registry. Circulation 113:2803–2809
Bowry AD, Brookhart MA, Choudhry NK (2008) Meta-analysis of the efficacy and safety of clopidogrel plus aspirin as compared to antiplatelet monotherapy for the prevention of vascular events. Am J Cardiol 101:960–966
Jerjes-Sanchez C (2005) Venous and arterial thrombosis: a continuous spectrum of the same disease? Eur Heart J 26:3–4
Korte W, Cattaneo M, Chassot PG et al (2011) Peri-operative management of antiplatelet therapy in patients with coronary artery disease: joint position paper by members of the working group on Perioperative Haemostasis of the Society on Thrombosis and Haemostasis Research (GTH), the working group on Perioperative Coagulation of the Austrian Society for Anesthesiology, Resuscitation and Intensive Care (OGARI) and the Working Group Thrombosis of the European Society for Cardiology (ESC). Thromb Haemost 105:743–749
Douketis JD, Berger PB, Dunn AS et al (2008) The perioperative management of antithrombotic therapy: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest 133(Suppl):299S–339S
Fleisher LA, Beckman JA, Brown KA et al (2009) 2009 ACCF/AHA focused update on perioperative beta blockade incorporated into the ACC/AHA 2007 guidelines on perioperative cardiovascular evaluation and care for noncardiac surgery. J Am Coll Cardiol 54:e13–e118
Poldermans D, Bax JJ, Boersma E et al (2009) Guidelines for pre-operative cardiac risk assessment and perioperative cardiac management in non-cardiac surgery. Eur Heart J 30:2769–2812
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fujikawa, T., Tanaka, A., Abe, T. et al. Effect of Antiplatelet Therapy on Patients Undergoing Gastroenterological Surgery: Thromboembolic Risks Versus Bleeding Risks During Its Perioperative Withdrawal. World J Surg 39, 139–149 (2015). https://doi.org/10.1007/s00268-014-2760-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-014-2760-3