Abstract
Background
When surgeons decide to perform lobectomy as the treatment of papillary thyroid carcinomas (PTCs), they must consider the possibility of contralateral cancer. We wanted to determine the incidence of bilateral PTCs (bPTCs) and analyze their characteristics. We also wanted to determine how many patients with bPTC were missed preoperatively.
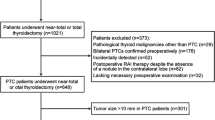
Methods
From January 2007 to May 2011, a total of 466 patients with PTC who were treated by total thyroidectomy at a single institution were enrolled. Patients were divided into two groups based on bilaterality. The patients with bPTCs were further investigated regarding the preoperative presence of the contralateral tumor.
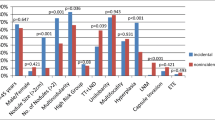
Results
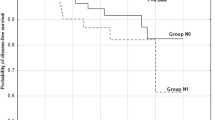
Bilaterality was seen in 29.8 % of PTC patients. In all, 36.8 % of PTCs ≥1 cm, and 25.7 % were papillary thyroid microcarcinomas (PTMCs). The presence of PTC in the contralateral lobe was missed in 15.8 % of bPTCs and in 21.3 % of bPTMCs. The rates of preoperatively nondetected contralateral cancer were 4.7 and 5.5 % for PTCs and PTMCs, respectively. Tumor size and multifocality were factors associated with bilaterality (p = 0.014 and p < 0.001, respectively).
Conclusions
Bilaterality is found more frequently when the tumor is large. Multifocality also can help predict the possibility of bilaterality. Therefore, total thyroidectomy may be necessary for patients with a multifocal or large tumor. It should be noted that the presence of a contralateral cancer is missed in 4.7 and 5.5 % of patients with preoperatively diagnosed unilateral PTC and PTMC, respectively.
Similar content being viewed by others
References
Davies L, Welch HG (2006) Increasing incidence of thyroid cancer in the United States, 1973–2002. JAMA 295:2164–2167
Mazeh H, Samet Y, Hochstein D et al (2011) Multifocality in well-differentiated thyroid carcinomas calls for total thyroidectomy. Am J Surg 201:770–775
Hodgson NC, Button J, Solorzano CC (2004) Thyroid cancer: is the incidence still increasing? Ann Surg Oncol 11:1093–1097
Cooper DS, Doherty GM, Haugen BR et al (2009) Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid 19:1167–1214
Baudin E, Travagli JP, Ropers J et al (1998) Microcarcinoma of the thyroid gland: the Gustave-Roussy Institute experience. Cancer 83:553–559
Haymart MR, Cayo M, Chen H (2009) Papillary thyroid microcarcinomas: big decisions for a small tumor. Ann Surg Oncol 16:3132–3139
Wang W, Zhao W, Wang H et al (2011) Poorer prognosis and higher prevalence of BRAF (V600E) mutation in synchronous bilateral papillary thyroid carcinoma. Ann Surg Oncol 19:31–36
Pitt SC, Sippel RS, Chen H (2009) Contralateral papillary thyroid cancer: does size matter? Am J Surg 197:342–347
Grigsby PW, Reddy RM, Moley JF et al (2006) Contralateral papillary thyroid cancer at completion thyroidectomy has no impact on recurrence or survival after radioiodine treatment. Surgery 140:1043–1047 discussion 1047–1049
Schonberger J, Marienhagen J, Agha A et al (2007) Papillary microcarcinoma and papillary cancer of the thyroid <or=1 cm: modified definition of the WHO and the therapeutic dilemma. Nuklearmedizin 46:115–120 quiz N141–142
Pasieka JL, Thompson NW, McLeod MK et al (1992) The incidence of bilateral well-differentiated thyroid cancer found at completion thyroidectomy. World J Surg 16:711–716. doi:10.1007/BF02067365 discussion 716–717
Koo BS, Lim HS, Lim YC et al (2010) Occult contralateral carcinoma in patients with unilateral papillary thyroid microcarcinoma. Ann Surg Oncol 17:1101–1105
Pacini F, Elisei R, Capezzone M et al (2001) Contralateral papillary thyroid cancer is frequent at completion thyroidectomy with no difference in low- and high-risk patients. Thyroid 11:877–881
Miccoli P, Minuto MN, Ugolini C et al (2007) Intrathyroidal differentiated thyroid carcinoma: tumor size-based surgical concepts. World J Surg 31:888–894. doi:10.1007/s00268-006-0795-9
Shattuck TM, Westra WH, Ladenson PW et al (2005) Independent clonal origins of distinct tumor foci in multifocal papillary thyroid carcinoma. N Engl J Med 352:2406–2412
Iida F, Yonekura M, Miyakawa M (1969) Study of intraglandular dissemination of thyroid cancer. Cancer 24:764–771
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lee, K.J., Cho, Y.J., Kim, J.G. et al. How Many Contralateral Papillary Thyroid Carcinomas Can Be Missed?. World J Surg 37, 780–785 (2013). https://doi.org/10.1007/s00268-013-1913-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-013-1913-0