Abstract
Background
Although papillary thyroid carcinoma (PTC) often presents as multifocal or bilateral tumors, but whether multifocality or bilaterality is associated with disease recurrence/persistence is controversial. We evaluated the association between multifocality and bilaterality of PTC and disease recurrence/persistence. We also analyzed the location and number of tumors in multifocal PTC.
Methods
We reviewed the medical records of 2,095 patients who underwent total thyroidectomy for PTC. Tumors were classified as solitary or multifocal PTC according to the number of tumors present. Multifocal PTCs were subdivided into multifocal-unilateral and multifocal-bilateral PTC based on the tumor location. Solitary tumor or multifocal tumors located in one lobe were classified as unilateral PTC, and tumors in both lobes were classified as bilateral PTC. We analyzed the clinicopathologic features and clinical outcomes in each classification. Logistic regression models were used to assess the relation between multifocality or bilaterality and disease recurrence/persistence.
Results
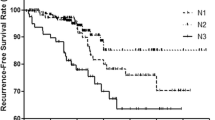
Extrathyroidal invasion, cervical lymph node metastasis, and advanced TNM stage were significantly more frequent in multifocal PTC than in solitary PTC. Extrathyroidal invasion, cervical lymph node metastasis, advanced TNM stage, and distant metastasis were significantly more frequent in bilateral PTC than in unilateral PTC. The clinicopathologic parameters did not differ significantly between patients with multifocal-unilateral and multifocal-bilateral PTC. Multifocality was found to be an independent predictor of disease recurrence/persistence [odds ratio (OR) 1.45, 95 % confidence interval (CI) 1.01–2.10, p = 0.04]. However, there was no association between bilaterality and disease recurrence/persistence (OR 0.98, 95 % CI 0.64–1.48, p = 0.92). In multifocal PTC, the number of tumors (OR 1.75, 95 % CI 1.04–2.97, p = 0.04), but not the location of tumors (OR 0.56, 95 % CI 0.31–1.02, p = 0.06), was significantly associated with disease recurrence/persistence.
Conclusions
Although multifocal and bilateral PTC had aggressive pathologic features, only multifocality was associated with an increased risk of disease recurrence/persistence. This suggests that the number of tumor foci, but not their location, is a significant predictor of clinical outcomes.

Similar content being viewed by others
References
Katoh R, Sasaki J, Kurihara H et al (1992) Multiple thyroid involvement (intraglandular metastasis) in papillary thyroid carcinoma: a clinicopathologic study of 105 consecutive patients. Cancer 70:1585–1590
Iida F, Yonekura M, Miyakawa M (1969) Study of intraglandular dissemination of thyroid cancer. Cancer 24:764–771
Shattuck TM, Westra WH, Ladenson PW et al (2005) Independent clonal origins of distinct tumor foci in multifocal papillary thyroid carcinoma. N Engl J Med 352:2406–2412
Sugg SL, Ezzat S, Rosen IB et al (1998) Distinct multiple RET/PTC gene rearrangements in multifocal papillary thyroid neoplasia. J Clin Endocrinol Metab 83:4116–4122
Park SY, Park YJ, Lee YJ et al (2006) Analysis of differential BRAF V600E mutational status in multifocal papillary thyroid carcinoma: evidence of independent clonal origin in distinct tumor foci. Cancer 107:1831–1838
McCarthy RP, Wang M, Jones TD et al (2006) Molecular evidence for the same clonal origin of multifocal papillary thyroid carcinomas. Clin Cancer Res 12:2414–2418
Wang W, Wang H, Teng X et al (2010) Clonal analysis of bilateral, recurrent, and metastatic papillary thyroid carcinomas. Hum Pathol 41:1299–1309
DeGroot LJ, Kaplan EL, McCormick M et al (1990) Natural history, treatment, and course of papillary thyroid carcinoma. J Clin Endocrinol Metab 71:414–424
Mazzaferri EL, Kloos RT (2001) Clinical review 128: current approaches to primary therapy for papillary and follicular thyroid cancer. J Clin Endocrinol Metab 86:1447–1463
Leboulleux S, Rubino C, Baudin E et al (2005) Prognostic factors for persistent or recurrent disease of papillary thyroid carcinoma with neck lymph node metastases and/or tumor extension beyond the thyroid capsule at initial diagnosis. J Clin Endocrinol Metab 90:5723–5729
Baek SK, Jung KY, Kang SM et al (2010) Clinical risk factors associated with cervical lymph node recurrence in papillary thyroid carcinoma. Thyroid 20:147–152
Scheumann GF, Gimm O, Wegener G, et al. (1994) Prognostic significance and surgical management of locoregional lymph node metastases in papillary thyroid cancer. World J Surg 18:559–567; discussion 567–558. doi:10.1007/BF00353765
Carcangiu ML, Zampi G, Pupi A et al (1985) Papillary carcinoma of the thyroid: a clinicopathologic study of 241 cases treated at the University of Florence, Italy. Cancer 55:805–828
Schindler AM, van Melle G, Evequoz B et al (1991) Prognostic factors in papillary carcinoma of the thyroid. Cancer 68:324–330
Mazzaferri EL, Jhiang SM (1994) Long-term impact of initial surgical and medical therapy on papillary and follicular thyroid cancer. Am J Med 97:418–428
Chow SM, Law SC, Chan JK et al (2003) Papillary microcarcinoma of the thyroid: prognostic significance of lymph node metastasis and multifocality. Cancer 98:31–40
Sciuto R, Romano L, Rea S et al (2009) Natural history and clinical outcome of differentiated thyroid carcinoma: a retrospective analysis of 1,503 patients treated at a single institution. Ann Oncol 20:1728–1735
Lin JD, Chao TC, Hsueh C et al (2009) High recurrent rate of multicentric papillary thyroid carcinoma. Ann Surg Oncol 16:2609–2616
Pasieka JL, Thompson NW, McLeod MK, et al. (1992) The incidence of bilateral well-differentiated thyroid cancer found at completion thyroidectomy. World J Surg 16:711–716; discussion 716–717. doi:10.1007/BF02067365
Pacini F, Elisei R, Capezzone M et al (2001) Contralateral papillary thyroid cancer is frequent at completion thyroidectomy with no difference in low- and high-risk patients. Thyroid 11:877–881
Grigsby PW, Reddy RM, Moley JF et al (2006) Contralateral papillary thyroid cancer at completion thyroidectomy has no impact on recurrence or survival after radioiodine treatment. Surgery 140:1043–1047 discussion 1047–1049
Wang W, Zhao W, Wang H et al (2012) Poorer prognosis and higher prevalence of BRAF V600E mutation in synchronous bilateral papillary thyroid carcinoma. Ann Surg Oncol 19:31–36
AJCC (American Joint Committee on Cancer) (2010) Thyroid. In: Edge SB, Byrd DR, Compton CC, et al. (eds). AJCC Cancer Staging Manual, 7th edn. Springer, New York, pp 87–96
Russell WO, Ibanez ML, Clark RL et al (1963) Thyroid carcinoma: classification, intraglandular dissemination, and clinicopathological study based upon whole organ sections of 80 glands. Cancer 16:1425–1460
Lin YK, Sheng JM, Zhao WH et al (2009) Multifocal papillary thyroid carcinoma: clinical analysis of 168 cases. Zhonghua Wai Ke Za Zhi 47:450–453
Hwang E, Pakdaman MN, Tamilia M et al (2010) Bilateral papillary thyroid cancer and associated histopathologic findings. J Otolaryngol Head Neck Surg 39:284–287
Acknowledgments
This work was supported by a 2012 SMC Clinical Research grant (CR0112101), the Korean Foundation for Cancer Research (PHO1115755), and a Samsung Biomedical Research Institute grant (SBRI C-B0-233-3).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kim, H.J., Sohn, S.Y., Jang, H.W. et al. Multifocality, But Not Bilaterality, Is a Predictor of Disease Recurrence/Persistence of Papillary Thyroid Carcinoma. World J Surg 37, 376–384 (2013). https://doi.org/10.1007/s00268-012-1835-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-012-1835-2