Abstract
Background
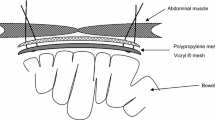
Prosthetic incisional hernia repair (PIHR) is superior to primary closure in preventing hernia recurrence. Serious complications have been associated with the use of prosthetic material. Complications of subsequent surgical interventions after prior PIHR in relation to its anatomical position were the objectives of this study.
Patients and Methods
Patients who underwent subsequent laparotomy/laparoscopy after PIHR between January 1992 and February 2005 at our institution were evaluated. Intraperitoneal and preperitoneal mesh was related to complication rates after subsequent surgical interventions.
Results
Sixty-six of 335 patients underwent re-laparotomy after PIHR. The perioperative course was complicated in 76% (30/39) of procedures with intraperitoneal placed grafts compared to 29% (8/27) of interventions with preperitoneally positioned meshes (P < 0.001). Small bowel resections were necessary in 21% of the intraperitoneal group (8/39) versus 0% in the preperitoneal group. Surgical site infection rates were higher in the intraperitoneal group (10/39, 26%, versus 1/27, 4%). Enterocutaneous fistula formation was rare and occurred in two patients after subsequent laparotomy (5%).
Conclusions
Re-laparotomy after PIHR with polypropylene meshes are associated with more preoperative and postoperative complications when the mesh is placed intraperitoneally. Therefore 0intraperitoneal positioning of polypropylene mesh at incisional hernia repair should be avoided if possible.

Similar content being viewed by others
References
Israelsson LA, Jonsson T. Incisional hernia after midline laparotomy: a prospective study. Eur J Surg 1996;162:125–129
Lewis RT, Wiegand FM. Natural history of vertical abdominal parietal closure: Prolene versus Dexon. Can J Surg 1989;32:196–200
Mudge M, Hughes LE. Incisional hernia: a 10 year prospective study of incidence and attitudes. Br J Surg 1985;72:70–71
Burger JW, Luijendijk RW, Hop WC, et al. Long-term follow-up of a randomized controlled trial of suture versus mesh repair of incisional hernia. Ann Surg 2004;240:578–583; discussion 583–585
Luijendijk RW, Hop WC, van den Tol MP, et al. A comparison of suture repair with mesh repair for incisional hernia. N Engl J Med 2000;343:392–398
Read RC, Yoder G. Recent trends in the management of incisional herniation. Arch Surg 1989;124:485–488
de Vries Reilingh TS, van Geldere D, Langenhorst B, et al. Repair of large midline incisional hernias with polypropylene mesh: comparison of three operative techniques. Hernia 2004;8:56–59
Langer C, Schaper A, Liersch T, et al. Prognosis factors in incisional hernia surgery: 25 years of experience. Hernia 2005;9:16–21
Usher FC. Hernia repair with knitted polypropylene mesh. Surg Gynecol Obstet 1963;117:239–240
Farmer L, Ayoub M, Warejcka D, et al. Adhesion formation after intraperitoneal and extraperitoneal implantation of polypropylene mesh. Am Surg 1998;64:144–146
Bodenbach M, Bschleipfer T, Stoschek M, et al. [Intravesical migration of a polypropylene mesh implant 3 years after laparoscopic transperitoneal hernioplasty]. Urologe A 2002;41:366–368
Losanoff JE, Richman BW, Jones JW. Entero-colocutaneous fistula: a late consequence of polypropylene mesh abdominal wall repair: case report and review of the literature. Hernia 2002;6:144–147
Riaz AA, Ismail M, Barsam A, et al. Mesh erosion into the bladder: a late complication of incisional hernia repair. A case report and review of the literature. Hernia 2004;8:158–159
Fernandez Lobato R, Martinez Santos C, Ortega Deballon P, et al. Colocutaneous fistula due to polypropylene mesh. Hernia 2001;5:107–109
Ott V, Groebli Y, Schneider R. Late intestinal fistula formation after incisional hernia using intraperitoneal mesh. Hernia 2005;9:103–104
Vrijland WW, Jeekel J, Steyerberg EW, et al. Intraperitoneal polypropylene mesh repair of incisional hernia is not associated with enterocutaneous fistula. Br J Surg 2000;87:348–352
Basoglu M, Yildirgan MI, Yilmaz I, et al. Late complications of incisional hernias following prosthetic mesh repair. Acta Chir Belg 2004;104:425–428
Leber GE, Garb JL, Alexander AI, et al. Long-term complications associated with prosthetic repair of incisional hernias. Arch Surg 1998;133:378–382
Menzies D, Ellis H. Intestinal obstruction from adhesions—how big is the problem? Ann R Coll Surg Engl 1990;72:60–63
Luijendijk RW, Wauters CC, Voormolen MH, et al. [Intra-abdominal adhesions and foreign-body granulomas following earlier laparotomy]. Ned Tijdschr Geneeskd 1994;138):717–721
Luijendijk RW, de Lange DC, Wauters CC, et al. Foreign material in postoperative adhesions. Ann Surg 1996;223:242–248
Morris-Stiff GJ, Hughes LE. The outcomes of nonabsorbable mesh placed within the abdominal cavity: literature review and clinical experience. J Am Coll Surg 1998;186:352–367
Molloy RG, Moran KT, Waldron RP, et al. Massive incisional hernia: abdominal wall replacement with Marlex mesh. Br J Surg 1991;78:242–244
White TJ, Santos MC, Thompson JS. Factors affecting wound complications in repair of ventral hernias. Am Surg 1998;64:276–280
Sikkink CJ, de Reilingh TS, Malyar AW, et al. Adhesion formation and reherniation differ between meshes used for abdominal wall reconstruction. Hernia 2006;10:218–222
Author information
Authors and Affiliations
Corresponding author
Additional information
J. A. Halm and L. L. de Wall contributed equally to the writing of this article.
Rights and permissions
About this article
Cite this article
Halm, J.A., de Wall, L.L., Steyerberg, E.W. et al. Intraperitoneal Polypropylene Mesh Hernia Repair Complicates Subsequent Abdominal Surgery. World J. Surg. 31, 423–429 (2007). https://doi.org/10.1007/s00268-006-0317-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-006-0317-9