Abstract
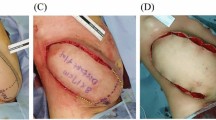
Facial defect reconstruction is a challenge for plastic surgeons due to unique esthetic and functional properties of the region. Facial tissue expansion provides an ideal reconstruction resource. However, the donor site is limited in the facial region. Thus, a cost-effective expansion management is crucial for an efficient reconstruction. In this article, the evolution of our donor site preference for tissue expansion from pure healthy tissue to a defect-healthy tissue combination is presented. Fifteen patients underwent skin reconstruction with local tissue expansion for facial and cervical defects. The full facial or cervical region including the defect and healthy tissue combination was determined as the donor expansion site. The donor site was not limited only to pure healthy tissue. The largest size rectangular expander suitable for the combined expandable donor site size was placed under the defect and healthy tissue border, paying attention to carry the expander far beneath the defect site. The defect site and most adjacent healthy tissue were expanded simultaneously. Major complications such as infection, hematoma, rupture, or flap necrosis were not observed. The expansion of defect-healthy tissue border presented successful reconstruction results with acceptable scars. In the traditional tissue expansion concept, using a large size expander to provide more abundant flap gain does not comply with the limited size of healthy donor site in the face. Expanding the whole facial region, without restriction of the defect, supplies excess donor tissue area for larger size expander use. Eventually, defect-healthy tissue border expansion with large expanders results in minimum final scar and less tissue loss in flap relocation and enables optimal flap gain. This method can easily be adapted to any tissue expansion site of the body.
Level of Evidence IV
This journal requires that authors assign a level of evidence to each article. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors www.springer.com/00266.





Similar content being viewed by others
References
Argenta LC, Watanabe MJ, Grabb WC (1983) The use of tissue expansion in head and neck reconstruction. Ann Plast Surg 11:31–37
Kawashima T, Yamada A, Ueda K, Asato H, Harii K (1994) Tissue expansion in facial reconstruction. Plast Reconstr Surg 94:944–950
Neale HW, Kurtzman LC, Goh KB, Billmire DA, Yakuboff KP, Warden G (1993) Tissue expanders in the lower face and anterior neck in pediatric burn patients: limitations and pitfalls. Plast Reconstr Surg 91:624–631
Neumann CG (1957) The expansion of an area of skin by progressive distention of a subcutaneous balloon; use of the method for securing skin for subtotal reconstruction of the ear. Plast Reconstr Surg (1946) 19:124–130
Radovan C (1982) Breast reconstruction after mastectomy using the temporary expander. Plast Reconstr Surg 69:195–208
Radovan C (1984) Tissue expansion in soft-tissue reconstruction. Plast Reconstr Surg 74:482–492
Turko A, Fuzaylov G, Savchyn V, Driscoll D (2013) Immediate and early tissue expander placement for acute closure of scalp wounds. Ann Plast Surg 71:160–165
Buhrer DP, Huang TT, Yee HW, Blackwell SJ (1988) Treatment of burn alopecia with tissue expanders in children. Plast Reconstr Surg 81:512–515
Chun JT, Rohrich RJ (1998) Versatility of tissue expansion in head and neck burn reconstruction. Ann Plast Surg 41:11–16
MacLennan SE, Corcoran JF, Neale HW (2000) Tissue expansion in head and neck burn reconstruction. Clin Plast Surg 27:121–132
Manders EK, Schenden MJ, Furrey JA, Hetzler PT, Davis TS, Graham WP 3rd (1984) Soft-tissue expansion: concepts and complications. Plast Reconstr Surg 74:493–507
Antonyshyn O, Gruss JS, Zuker R, Mackinnon SE (1988) Tissue expansion in head and neck reconstruction. Plast Reconstr Surg 82:58–68
Nordström RE, Pietilä JP, Rintala AE (1988) Clinical experience with tissue expansion. Facial Plast Surg 5:317–327
Baker SR, Swanson NA (1990) Tissue expansion of the head and neck. Indications, technique, and complications. Arch Otolaryngol Head Neck Surg 116:1147–1153
Baker SR, Swanson NA (1990) Clinical applications of tissue expansion in head and neck surgery. Laryngoscope 100:313–319
Marks MW, Argenta LC (2013) Principles and applications of tissue expansion. In: Neligan PC (ed) Plastic Surgery, vol 1. Elsevier, New York, pp 622–653
Bascom DA, Wax MK (2002) Tissue expansion in the head and neck: current state of the art. Curr Opin Otolaryngol Head Neck Surg. 10:273–277
Nordström RE (1984) “Stretch-back” in scalp reductions for male pattern baldness. Plast Reconstr Surg 73:422–426
Bhandari PS (2009) Mathematical calculations in a spherical tissue expander. Ann Plast Surg 62:200–204
van Rappard JH, Molenaar J, van Doorn K, Sonneveld GJ, Borghouts JM (1988) Surface-area increase in tissue expansion. Plast Reconstr Surg 82:833–839
Zide BM, Karp NS (1992) Maximizing gain from rectangular tissue expanders. Plast Reconstr Surg 90:500–504
Bauer BS, Margulis A (2004) The expanded transposition flap: shifting paradigms based on experience gained from two decades of pediatric tissue expansion. Plast Reconstr Surg 114:98–106
Lentz AK, Bauer BS (2014) Tissue expansion. In: Thorne CH (ed) Grabb and Smith’s Plastic Surgery, 7th edn. Lippincott Williams & Wilkins, Philadelphia, pp 87–93
Bauer BS, Few JW, Chavez CD, Galiano RD (2001) The role of tissue expansion in the management of large congenital pigmented nevi of the forehead in the pediatric patient. Plast Reconstr Surg 107:668–675
Khalatbari B, Bakhshaeekia A (2013) Ten-year experience in face and neck unit reconstruction using tissue expanders. Burns 39:522–527
Alagöz MŞ, Öksüz S, Keskin M, Yaşar EK, Eren F, Hasdemir M, Ülkür E (2015) Avoiding extended scar in skin expansion: Alagoz technique. J Craniofac Surg 26:e291–e292
Duits EH, Molenaar J, van Rappard JH (1989) The modeling of skin expanders. Plast Reconstr Surg 83:362–367
Pamplona DC, Weber HI, Leta FR (2014) Optimization of the use of skin expanders. Skin Res Technol 20:463–472
Handschel J, Schultz S, Depprich RA, Smeets R, Sproll C, Ommerborn MA, Naujoks C, Kübler NR, Zimmermann A (2013) Tissue expanders for soft tissue reconstruction in the head and neck area: requirements and limitations. Clin Oral Investig 17:573–578
Acknowledgments
The authors would like to thank Dr. Celalettin Sever, Dr. Emrah Kağan Yaşar, and Dr. Hüseyin Gerçek for their assistance in data collection and in the surgeries.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest to disclose.
Rights and permissions
About this article
Cite this article
Öksüz, S., Alagöz, M.Ş. & Ülkür, E. Changing the Donor Site Selection Concept of Facial Skin Expansion from Pure Healthy Tissue to Defect and Healthy Tissue Combination. Aesth Plast Surg 39, 745–751 (2015). https://doi.org/10.1007/s00266-015-0547-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-015-0547-z