Abstract
Purpose
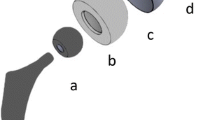
Constrained devices, standard implants with large heads, and dual mobility systems have become popular options to manage instability after total hip arthroplasty (THA). Clinical results with these options have shown variable success rates and significant higher rates of aseptic loosening and mechanical failures with constrained implants. Literature suggests potential advantages of dual mobility, however little is known about its biomechanics. We present a comparative biomechanical study of a standard implant, a constrained implant, and a dual mobility system.
Methods
A finite element analysis was developed to assess and compare these acetabular options with regard to the range of motion (ROM) to impingement, the angle of dislocation, the resistive torque, the volume of polyethylene (PE) with a stress above 80% of the elastic limit, and the interfacial cup/bone stress.
Results
Dual mobility implants provided the greatest ROM to impingement and allowed delaying subluxation and dislocation when compared to standard and constrained implants. Dual mobility also demonstrated the lowest resistive torque at subluxation while the constrained implant provided the greatest one. The lowest critical PE volume was observed with the dual mobility implant, and the highest stress at the interfaces was observed with the constrained implant.
Conclusion
This study highlights the biomechanical advantages of dual mobility systems over constrained and standard implants, and is supported by the clinical results reported. Therefore, the use of dual mobility systems in situations at risk for instability should be advocated and constrained implants should be restricted to salvage situations.



Similar content being viewed by others
References
Morrey BF (2004) Results of reoperation for hip dislocation: the big picture. Clin Orthop 94–101. doi: 10.1097/01.blo.0000150318.27723.8c
Berry DJ (2001) Unstable total hip arthroplasty: detailed overview. Instr Course Lect 50:265–274
Bartz RL, Noble PC, Kadakia NR, Tullos HS (2000) The effect of femoral component head size on posterior dislocation of the artificial hip joint. J Bone Joint Surg Am 82:1300–1307
Cooper HJ, Della V (2014) Large diameter femoral heads: is bigger always better? Bone Joint J 96B:23–26. doi:10.1302/0301-620X.96B11.34342
Burroughs BR, Hallstrom B, Golladay GJ et al (2005) Range of motion and stability in total hip arthroplasty with 28-, 32-, 38-, and 44-mm femoral head sizes: An in vitro study. J Arthroplasty 20:11–19. doi:10.1016/j.arth.2004.07.008
Goetz DD, Capello WN, Callaghan JJ, et al (1998) Salvage of total hip instability with a constrained acetabular component. Clin Orthop 171–181
Shapiro GS, Weiland DE, Markel DC et al (2003) The use of a constrained acetabular component for recurrent dislocation. J Arthroplasty 18:250–258. doi:10.1054/arth.2003.50090
Guyen O, Lewallen DG, Cabanela ME (2008) Modes of failure of Osteonics constrained tripolar implants: a retrospective analysis of forty-three failed implants. J Bone Joint Surg Am 90:1553–60. doi:10.2106/JBJS.G.00317
Guyen O, Pibarot V, Vaz G et al (2007) Unconstrained tripolar implants for primary total hip arthroplasty in patients at risk for dislocation. J Arthroplasty 22:849–58. doi:10.1016/j.arth.2006.11.014
Guyen O, Pibarot V, Vaz G et al (2009) Use of a dual mobility socket to manage total hip arthroplasty instability. Clin Orthop Relat Res 467:465–72. doi:10.1007/s11999-008-0476-0
Vasukutty NL, Middleton RG, Young P et al (2014) A double mobility acetabular implant for primary hip arthroplasty in patients at high risk of dislocation. Ann R Coll Surg Engl 96:597–601. doi:10.1308/003588414X14055925058391
Vigdorchik JM, D’Apuzzo MR, Markel DC et al (2015) Lack of early dislocation following total hip arthroplasty with a new dual mobility acetabular design. Hip Int 25:34–38. doi:10.5301/hipint.5000186
Vasukutty NL, Middleton RG, Matthews EC et al (2012) The double-mobility acetabular component in revision total hip replacement. J Bone Joint Surg Br 94(B):603–608. doi:10.1302/0301-620X.94B5.27876
Bensen AS, Jakobsen T, Krarup N (2014) Dual mobility cup reduces dislocation and re-operation when used to treat displaced femoral neck fractures. Int Orthop 38:1241–1245. doi:10.1007/s00264-013-2276-8
van Heumen M, Heesterbeek PJC, Swierstra BA et al (2015) Dual mobility acetabular component in revision total hip arthroplasty for persistent dislocation: no dislocations in 50 hips after 1–5 years. J Orthop Traumatol 16:15–20. doi:10.1007/s10195-014-0318-7
Rüdiger HA, Parvex V, Terrier A (2016) Impact of the femoral head position on moment arms in total hip arthroplasty: a parametric finite element study. J Arthroplasty 31:715–720. doi:10.1016/j.arth.2015.09.044
Terrier A, Levrero Florencio F, Rudiger HA (2014) Benefit of cup medialization in total hip arthroplasty is associated with femoral anatomy. Clin Orthop Relat Res 472:3159–65. doi:10.1007/s11999-014-3787-3
Terrier A, Parvex V, Rüdiger HA (2016) Impact of individual anatomy on the benefit of cup medialisation in total hip arthroplasty. Hip Int 26:537–542. doi:10.5301/hipint.5000392
Wu G, Siegler S, Allard P et al (2002) ISB recommendation on definitions of joint coordinate system of various joints for the reporting of human joint motion—part 1: ankle, hip, and spine. J Biomech 35:543–548
Pruitt LA (2005) Deformation, yielding, fracture and fatigue behavior of conventional and highly cross-linked ultra high molecular weight polyethylene. Biomaterials 26:905–15. doi:10.1016/j.biomaterials.2004.03.022
Teoh SH, Chan WH, Thampuran R (2002) An elasto-plastic finite element model for polyethylene wear in total hip arthroplasty. J Biomech 35:323–30
Keller TS (1994) Predicting the compressive mechanical behavior of bone. J Biomech 27:1159–68
Saikko VO (1996) A three-axis hip joint simulator for wear and friction studies on total hip prostheses. Proc Inst Mech Eng H 210:175–85
Combes A, Migaud H, Girard J et al (2013) Low rate of dislocation of dual-mobility cups in primary total hip arthroplasty. Clin Orthop 471:3891–3900. doi:10.1007/s11999-013-2929-3
Shrader MW, Parvizi J, Lewallen DG (2003) The use of a constrained acetabular component to treat instability after total hip arthroplasty. J Bone Joint Surg Am 85:2179–2183
Lombardi J, Skeels MD, Berend KR et al (2011) Do large heads enhance stability and restore native anatomy in primary total hip arthroplasty? Clin Orthop 469:1547–1553. doi:10.1007/s11999-010-1605-0
Muratoglu OK, Bragdon CR, O’Connor D et al (2001) Larger diameter femoral heads used in conjunction with a highly cross-linked ultra-high molecular weight polyethylene: a new concept. J Arthroplasty 16:24–30. doi:10.1054/arth.2001.28376
Blumenfeld TJ, McKellop HA, Schmalzried TP, Billi F (2011) Fracture of a cross-linked polyethylene liner. A multifactorial issue. J Arthroplasty 26:666. doi:10.1016/j.arth.2010.07.009, e5–666.e8
Guyen O, Chen QS, Bejui-Hugues J et al (2007) Unconstrained tripolar hip implants: effect on hip stability. Clin Orthop Relat Res 455:202–8. doi:10.1097/01.blo.0000238796.59596.1f
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest statement
This study was funded by internal sources. The funding source did not play a role in the investigation.
Ethical review committee statement
Included.
Location where the work was performed
The study was performed at the Ecole Polytechnique Fédérale de Lausanne (EPFL) and the Centre Hospitalier Universitaire Vaudois (CHUV) in Lausanne/Switzerland.
Rights and permissions
About this article
Cite this article
Terrier, A., Latypova, A., Guillemin, M. et al. Dual mobility cups provide biomechanical advantages in situations at risk for dislocation: a finite element analysis. International Orthopaedics (SICOT) 41, 551–556 (2017). https://doi.org/10.1007/s00264-016-3368-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-016-3368-z