Abstract
Purpose
The aim of the present study was to evaluate the clinical and radiographic results of primary total hip arthroplasty (THA) performed with the Alloclassic Variall system (a modified version of the Alloclassic Zweymüller system) and to compare them with those in the literature for the original system.
Methods
Between January 2001 and December 2002, 273 consecutive primary THAs were performed in 259 patients at a single centre with the study system, using ceramic-on-ceramic (81.7 %) or ceramic-on-highly-crosslinked-polyethylene (18.3 %) articulations.
Results
At the time of this study, 28 patients (29 hips; 10.6 %) had died and 40 (43 hips; 15.8 %) were lost to follow-up. Seventeen patients (19 hips; 7.0 %) could be reached only by telephone. There were four revisions in four patients (1.5 %), all involving only the femoral component. Ten-year Kaplan-Meier survival with revision of any component for any reason as the endpoint was 98.4 % (95 % confidence interval: 96.9–100 %; 30 hips remained ‘at risk’). A total of 170 unrevised patients (178 hips; 65.2 %) were assessed clinically and radiographically at a median follow-up of 9.3 years (interquartile range [IQR] 8.8–9.8 years). The median Harris hip score (HHS) was 99.9 points (IQR 97.7–100). The score did not differ significantly between the two articulations. There was no sign of radiographic loosening.
Conclusions
The ten-year implant survival and the HHS score outcomes for THAs performed with the novel system were in line with those documented in the literature for its predecessor.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The Alloclassic Zweymüller hip system (Zimmer GmbH, Winterthur, CH) was introduced in 1979 for patients undergoing total hip arthroplasty (THA) [1]. The system includes: the Alloclassic Zweymüller stem, a straight tapered titanium alloy stem with a rectangular cross-section; and the Alloclassic Zweymüller conical self-tapping cement-free (CSF) cup, a conically shaped titanium shell with sharp self-tapping blades (i.e. a screw shell design) that combines with either a polyethylene (PE) insert or a sandwich insert made of PE/Wrought-Forged-CoCrMo (Metasul, Zimmer GmbH) (Fig. 1). The system has been modified several times, but without changing its design philosophy [1].
In the late 1990s, the Alloclassic Variall system (Zimmer GmbH) was developed from the original system. Unlike the original stem, the proximal part of the novel stem has an additional surface macrostructure, with grooves. This increases the intertrochanteric initial press-fit [2], while enlarging the contact area between new-formed bone and the stem to enhance secondary stability. Unlike the original shell, the novel shell has a spherical base [3], rather than sharp edges, to reduce the risk of bone perforation. In addition, the novel shell can also be combined with ceramic inserts.
Although many studies have documented mid to long-term clinical outcomes with the original system [4–12], only a few have been published on the novel system [2, 3, 13]. To aid healthcare decision-making, we reviewed the results of THAs performed with the novel system at a single centre, and compared these results with those reported in the literature for the original stem.
Materials and methods
In 2011, using the hip arthroplasty register of St.Vincent`s Hospital, Linz, Austria, all patients who underwent THA with the study device, using either ceramic-on-ceramic (CoC) or ceramic-on-highly-crosslinked-polyethylene (CoPE) articulations, between January 2001 and December 2002 were selected to constitute the study cohort.
The cohort comprised 259 consecutive patients (273 THAs), of whom 93 were men (35.9 %) and 166 women (64.1 %), at a median age of 65 years at the time of surgery (IQR 52–72 years). Indications for surgery were: primary osteoarthritis in 209 cases (76.6 %), osteonecrosis of the femoral head in 31 cases (11.4 %), developmental hip dysplasia in 30 cases (11.0 %) and fracture of the femoral neck in three cases (1.1 %) (Table 1).
Operative information
All THAs were performed using the lateral approach, with the patients placed in supine position [14, 15]. The acetabular shell was screwed into the acetabulum; with optimal orientation considered to be an anteversion angle of 10–15° and an inclination angle of 40–45°. The shells were combined with ceramic inserts (BIOLOX forte, CeramTec GmbH, DE) in 223 cases (81.7 %), and with highly-crosslinked-PE (Durasul, Zimmer GmbH) inserts in the remaining 50 cases (18.3 %). 28 mm ceramic femoral heads (BIOLOX forte, CeramTec GmbH, DE) were implanted in all hips.
All patients were asked to return for a follow-up visit to assess implant survival, the incidence and nature of any adverse events, and clinical and radiographic outcomes at approximately ten years after surgery.
Clinical outcome assessment
Harris hip score (HHS) was assessed at follow-up in 2011 for unrevised patients. The results were classified as: excellent (90–100), good (80–89), fair (70–79) or poor (<70).
Radiographic assessment
Hip anteroposterior (AP) view radiographs obtained in the immediate post-operative period and at the final follow-up in 2011 were analysed by one of the authors (KE). The following parameters were assessed: femoral and acetabular radiolucent lines, femoral bone hypertrophy, heterotopic ossification, stem subsidence and change in orientation of the cup.
Radiolucent lines are lower bone density lines around the implant, at the interface between the bone and the prosthesis. Bone hypertrophy is an area of greater bone density than the surroundings. Radiolucent lines and hypertrophy were assessed with reference to the seven zones defined by Gruen et al. [16] for the femoral component and with reference to the three DeLee and Charnley areas [17] for the acetabular component. Heterotopic ossification was classified using the criteria set out by Brooker et al. [18]. Stem subsidence was defined as downward axial stem migration relative to the position documented in the first post-operative radiograph. Only stem subsidence of ≥5 mm was considered [19]. According to Engh et al. [20], femoral stems were regarded as radiographically loose when there was a progressive subsidence or a progressive widening of radiolucent lines; acetabular shells were considered as radiographically loose when there was progressive widening of radiolucent lines or a change in inclination.
Statistical analysis
Categorical data were summarized using counts and percentages. Continuous data were expressed as mean, standard deviation (SD), median and IQR. The Shapiro-Wilk test was used to test for normality.
Comparison between groups (i.e. CoC THA vs. CoPE THA) was performed using Student's t-test in case of normally distributed continuous data, or using Mann–Whitney U-test for non-parametric analysis, while proportions were compared by chi-squared test or by Fisher’s exact test, as appropriate. A p-value of <0.05 was considered to indicate statistical significance.
Survival rates at ten years were calculated using Kaplan-Meier survival analysis with 95 % confidence intervals. The following endpoints were considered: stem revision for any reason, cup (i.e. shell and/or insert) revision for any reason and revision of any component for any reason. Patients who had died or who were lost-to-follow-up were censored at the time of the last available information on their implant status. The statistical analysis was performed using IBM SPSS 21 (IBM Corp.).
Ethical approval
This study was approved by the Ethics Committee of the Institution. Informed consent was obtained from all individual participants included in the study.
Results
At the time of final review, 170 (178 THAs) patients from the original 259 (273 THAs) were assessed both clinically and radiographically at a median follow-up of 9.3 years (IQR 8.8–9.8 years). Of the other patients, 28 (29 THAs) had died, 40 (43 THAs) were lost to follow-up and four (four THAs) had undergone hip revision. Finally, 17 patients (19 THAs) underwent only a telephone interview as they were unable to attend hospital due to distance or poor general condition (Fig. 2). None had undergone revision surgery, and the date of the phone call was considered in the survival rate calculation.
Among the four revisions, two femoral stems were revised due to periprosthetic fracture two weeks and two months after implantation, respectively. One femoral stem was revised five months after implantation due to significant subsidence. The stem had not osseointegrated, and it was considered undersized and was replaced by a larger stem. One stem was revised 6.3 years after implantation due to aseptic loosening (i.e. radiographic signs of loosening and pain). Intra-operatively the implant was found to be definitely loose.
There were also four intra-operative fractures of the greater trochanter, with cranial dislocation of the fractured fragment. They were successfully treated intra-operatively with cerclage wires. No other complications were documented.
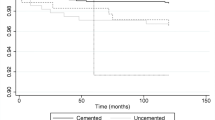
Ten-year Kaplan-Meier survival was 100 % (with 30 hips remaining ‘at risk’), with cup revision for any reason as the endpoint, and 98.4 % (95 % CI 96.9–100 %; with 30 hips remaining ‘at risk’), with stem revision for any reason or any component revision for any reason as the endpoints (Fig. 3).
Clinical outcome assessment
The median HHS for the 170 unrevised patients (178 hips) who attended the last visit was 99.9 (IQR 97.7–100) (Table 2). The score was categorized as excellent or good in 174 cases (97.8 %) and fair in one case (0.6 %), while the results were poor in three cases (1.7 %). The poor HHS results in these three cases were mainly due to comorbidities (i.e. patient affected by spinal or contralateral hip disorders).
The HHS results did not significantly differ between the CoC and CoPE articulations (p = 0.254).
Radiological outcomes
Radiolucent lines around the stem in at least one Gruen zone were detected in 12 hips (6.7 % of the hips that could be assessed radiographically; see Fig. 4). The highest incidence was in zone 7 (ten hips; 5.6 %). No radiolucent lines were observed in zones 4, 5 and 6. Radiolucent lines around the acetabular shell were detected only in one hip in zone III (0.6 %). There were no radiolucent lines larger than 2 mm. Femoral bone hypertrophy around the stem was detected in five hips (2.8 % of the hips that could be assessed radiographically) in zone 3 (one hip), zone 4 (one hip), zone 5 (three hips) and zone 7 (one hip). None of the unrevised hips had stem subsidence or any other signs of stem or cup loosening at final follow-up. Heterotopic ossification was detected in 42 hips (23.6 %) and classified as grade I in 29 hips (16.3 %), grade II in 12 hips (6.7 %) and grade III in one hip (0.6 %). No hip had heterotopic ossification grade IV. The percentage of patients with heterotopic ossification was smaller in the group who received non-steroidal anti-inflammatory drugs (NSAIDs) than in those who received opioids or no medication (20.3 % versus 44.0 %; p = 0.010; chi-square test).
Discussion
The survival/revision rate is one of the most important parameters to consider when evaluating THA outcomes [9]. In our series we documented ten-year Kaplan-Meier survival of 98.4 % (95 % CI 96.6–100 %) with stem revision and any component revision as the endpoints, and 100 % with cup revision as the endpoint. We compared our results with those of published studies on the original system in primary THA as summarized in Table 3 [4, 6–12]. In these studies, the ten-year Kaplan-Meier survival rates range from 98.9 % to 100 % for the stem [7–9, 11], from 93 % to 99 % for the cup [7, 9, 11] and from 92 % to 98 % for the entire system (i.e. any component revision as endpoint) [4, 6, 7, 9–12].
Additionally, we analysed the review article by Janda et al. [1], which summarizes systematically searched published studies on THAs performed with the original system. The authors focused their statistical analysis not on KM survival, but on a parameter called ‘revisions per 100 observed component years’. This parameter allows to pool together data from different cohorts and to calculate an overall “revision rate”. All the patients in the initial cohort are taken into consideration until the time of the latest follow-up or death. For THAs performed with the original system, Janda et al. documented 0.27 revisions per 100 observed component years (95 % CI 0.20–0.37). This value was based on a pooled cohort of 1,760 THAs with a mean implantation time per THA of 8.69 years. In our cohort, taking into consideration all initial patients (273 THAs) until the time of last contact or death, there were 0.19 revisions per 100 observed component years (with a mean implantation time per THA of 7.9 years and with revision for any reason as the endpoint), which is outside the lower extremity of the 95 % CI documented by Janda et al. The survival performance of this novel system is therefore in line with or exceeds that documented for the original system.
Regarding patients outcomes, the median HHS in our series was 99.9 (mean 97.4) at a median follow-up of 9.3 years (mean, 9.3 years), with no significant differences between CoC and CoPE articulations. In the reviewed literature, two studies documented the HHS at a follow-up time similar to ours. Pieringer et al. [8] reported a median HHS of 89 (mean, 85.4) at a mean follow-up of 10.8 years, while Grübl et al. [7] reported a mean HHS of 85.4 at a median follow-up of 10.1 years.
Despite the excellent Harris hip score results in our study cohort, there were four intra-operative trochanteric fractures (1.5 %), which are, however, not uncommon during the implantation of standard-length stems through the direct lateral surgical approach [21].
Radiolucent lines around the stem in at least one Gruen zone were reported in 6.7 % of the hips that could be radiographically assessed at final follow-up. This value is far lower than that observed in previous studies with the original stem [10, 22]. Stem geometry is known to influence post-operative bone remodelling [23], and the lower incidence of radiolucent lines in the proximal Gruen zones with the novel device may indicate that the proximal macrostructure of the stem improves proximal osseointegration. Nevertheless, the impact of proximal radiolucent lines on longevity of Alloclassic Zweymüller-type stems has been questioned—proximal femoral radiolucent lines have, in fact, been described as clinically irrelevant after observation periods of up to 17 years [10, 22].
Heterotopic ossification was documented in 23.6 % of cases, with a significantly higher incidence in patients who did not receive NSAIDs (p = 0.010). This supports the literature indicating that NSAID administration helps to prevent heterotopic ossification [24, 25].
The present study has some limitations, primarily the lack of pre-operative HHS and the retrospective character of the study design. However, as far as we are aware, this is the first study to document eight- to ten-year results for THAs performed with this relatively new system.
In conclusion, eight- to ten-year outcomes for THAs performed with the study system were in line with those documented for its predecessor.
References
Janda W, Huebl M, Stoeckl B, Thaler M, Labek G (2010) Performance of the Zweymueller total hip arthroplasty system: a literature review including arthroplasty register data. Eur Orthop Traumatol 1:9–15. doi:10.1007/s12570-010-0004-z
Suda AJ, Knahr K (2009) Early results with the cementless Variall hip system. Expert Rev Med Devices 6(1):21–25. doi:10.1586/17434440.6.1.21
Knahr K, Karamat L, Loho G, Pospischill M (2005) Tribological considerations for a new hip system. Acta Chir Orthop Traumatol Cech 72(2):116–121
Busch VJ, Pouw MH, Laumen AM, van Susante JL, Vervest AM (2012) Long-term outcome of 73 Zweymuller total hip prostheses with a screw cup in patients under 50 years of age. Hip Int 22(3):292–295. doi:10.5301/HIP.2012.9239
Delaunay C, Cazeau C, Kapandji AI (1998) Cementless primary total hip replacement. Four to eight year results with the Zweymuller-Alloclassic prosthesis. Int Orthop 22(1):1–5. doi:10.1007/s002640050198
Garcia-Cimbrelo E, Cruz-Pardos A, Madero R, Ortega-Andreu M (2003) Total hip arthroplasty with use of the cementless Zweymuller Alloclassic system. A ten to thirteen-year follow-up study. J Bone Joint Surg Am 85-A(2):296–303
Grubl A, Chiari C, Gruber M, Kaider A, Gottsauner-Wolf F (2002) Cementless total hip arthroplasty with a tapered, rectangular titanium stem and a threaded cup: a minimum ten-year follow-up. J Bone Joint Surg Am 84-A(3):425–431
Pieringer H, Auersperg V, Griessler W, Bohler N (2003) Long-term results with the cementless Alloclassic brand hip arthroplasty system. J Arthroplasty 18(3):321–328. doi:10.1054/arth.2003.50045
Pieringer H, Auersperg V, Bohler N (2006) Long-term results of the cementless Alloclassic hip arthroplasty system using a 28-mm ceramic head: with a retrospective comparison to a 32-mm head. J Arthroplasty 21(7):967–974. doi:10.1016/j.arth.2005.08.027
Pospischill M, Knahr K (2005) Cementless total hip arthroplasty using a threaded cup and a rectangular tapered stem. Follow-up for ten to 17 years. J Bone Joint Surg (Br) 87(9):1210–1215. doi:10.1302/0301-620X.87B9.16107
Suckel A, Geiger F, Kinzl L, Wulker N, Garbrecht M (2009) Long-term results for the uncemented Zweymuller/Alloclassic hip endoprosthesis. A 15-year minimum follow-up of 320 hip operations. J Arthroplasty 24(6):846–853. doi:10.1016/j.arth.2008.03.021
Zwartele R, Peters A, Brouwers J, Olsthoorn P, Brand R, Doets C (2008) Long-term results of cementless primary total hip arthroplasty with a threaded cup and a tapered, rectangular titanium stem in rheumatoid arthritis and osteoarthritis. Int Orthop 32(5):581–587. doi:10.1007/s00264-007-0383-0
Knahr K, Pokorny A, Frank A (2011) The noisy hip: only in ceramic-on-ceramic bearings? J Bone Joint Surg (Br) 93-B(SUPP IV):429–430
Bauer R, Kerschbaumer F, Poisel S, Oberthaler W (1979) The transgluteal approach to the hip joint. Arch Orthop Trauma Surg 95(1–2):47–49
Reichert JC, Volkmann MR, Koppmair M, Rackwitz L, Ludemann M, Rudert M, Noth U (2015) Comparative retrospective study of the direct anterior and transgluteal approaches for primary total hip arthroplasty. Int Orthop. doi:10.1007/s00264-015-2732-8
Gruen TA, McNeice GM, Amstutz HC (1979) "Modes of failure" of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res 141:17–27
DeLee JG, Charnley J (1976) Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res 121:20–32
Brooker AF, Bowerman JW, Robinson RA, Riley LH (1973) Ectopic ossification following total hip replacement. Incidence and a method of classification. J Bone Joint Surg Am 55(8):1629–1632
Evola FR, Evola G, Graceffa A, Sessa A, Pavone V, Costarella L, Sessa G, Avondo S (2014) Performance of the CLS Spotorno uncemented stem in the third decade after implantation. Bone Joint J 96-B(4):455–461. doi:10.1302/0301-620X.96B4.32607
Engh CA, Glassman AH, Griffin WL, Mayer JG (1988) Results of cementless revision for failed cemented total hip arthroplasty. Clin Orthop Relat Res 235:91–110
Molli RG, Lombardi AV Jr, Berend KR, Adams JB, Sneller MA (2012) A short tapered stem reduces intraoperative complications in primary total hip arthroplasty. Clin Orthop Relat Res 470(2):450–461. doi:10.1007/s11999-011-2068-7
Dohle J, Becker W, Braun M (2001) Radiological analysis of osseointegration after implantation of the Zweymuller-Alloclassic total hip system. Z Orthop Ihre Grenzgeb 139(6):517–524. doi:10.1055/s-2001-19234
Engh CA Jr, Sychterz C, Engh C Sr (1999) Factors affecting femoral bone remodeling after cementless total hip arthroplasty. J Arthroplasty 14(5):637–644. doi:10.1016/S0883-5403(99)90091-8
Bedi A, Zbeda RM, Bueno VF, Downie B, Dolan M, Kelly BT (2012) The incidence of heterotopic ossification after hip arthroscopy. Am J Sports Med 40(4):854–863. doi:10.1177/0363546511434285
Fransen M, Neal B (2004) Non-steroidal anti-inflammatory drugs for preventing heterotopic bone formation after hip arthroplasty. Cochrane Database Syst Rev 3, CD001160. doi:10.1002/14651858.CD001160.pub2
Acknowledgments
The authors would like to thank Aida Stamm, M.Sc., (Clinical Research Department, Zimmer GmbH) for study coordination.
Conflict of interest
The clinical study was sponsored by Zimmer GmbH (Winterthur, CH). Josef Hochreiter, Katja Emmanuel and Klaus Kirschbichler have no competing interests. Giovanni Brusaferri is employed by Zimmer GmbH.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Hochreiter, J., Brusaferri, G., Kirschbichler, K. et al. Long-term follow-up of primary total hip arthroplasty with the Alloclassic Variall system. International Orthopaedics (SICOT) 40, 1409–1415 (2016). https://doi.org/10.1007/s00264-015-2953-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-015-2953-x