Abstract
Purpose
Ligaments are frequently damaged in sports activities and trauma, and severe ligament injury can lead to joint instability and osteoarthritis. In this study, we aimed to regenerate the medial collateral ligament (MCL) using an absorbable stent-shaped poly-l-lactic acid (PLLA) scaffold in a rabbit model to examine the biocompatibility and mechanical properties.
Methods
Twenty-three Japanese white rabbits were used in this study. MCL defects were surgically created in the knee joints and then reconstructed using stent-shaped PLLA scaffolds. As controls, flexor digitorum longus (FDL) tendons were implanted into the contralateral knees. Seven rabbits were sacrificed at three time points, conducted four, eight and 16 weeks after the operation. The regenerated tissues were histologically evaluated using fibre alignment scoring, morphology of fibroblast scoring and immunohistochemical analysis of types I and III collagen. The regenerated tissues were also biomechanically evaluated by measuring the ultimate failure load and stiffness.
Results
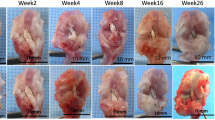
At four weeks post-operation, spindle-shaped cells were observed on the inside of the scaffolds. At eight weeks, maturation of the regenerated tissues and collagen fibre alignment parallel to the ligaments was observed. At 16 weeks, the fibre alignment had become denser. The fibre alignment and morphology of fibroblast scores significantly increased in a time-dependent manner. Expression of type I collagen was more strongly observed in the scaffold group at eight and 16 weeks post-operation than at four weeks. Type III collagen was also observed at four, eight and 16 weeks post-operation. A thin layer of fibrocartilage was observed at the ligament-bone junction at eight and 16 weeks. The ultimate failure load of the scaffold group was 46.7 ± 20.7 N, 66.5 ± 11.0 N and 74.3 ± 11.5 N at four, eight and 16 weeks post-operation, respectively. There was no statistical difference between the normal MCL and the scaffold group at 16 weeks post-operation.
Conclusions
The stent-shaped PLLA scaffold allowed for MCL regeneration with type I collagen expression and fibrocartilage formation and resulted in sufficient mechanical function.




Similar content being viewed by others
References
O’Donoghue DH (1973) Reconstruction for medial instability of the knee. J Bone Joint Surg Am 55:941–954
Lind M, Jakobsen BW, Lund B, Hansen MS, Abdallah O, Christiansen SE (2009) Anatomical reconstruction of the medial collateral ligament and posteromedial corner of the knee in patients with chronic medial collateral ligament instability. Am J Sports Med 37:1116–1122. doi:10.1177/0363546509332498
Yoshiya S, Kuroda R, Mizuno K, Yamamoto T, Kurosaka M (2005) Medial collateral ligament reconstruction using autogenous hamstring tendons: technique and results in initial cases. Am J Sports Med 33:1380–1385. doi:10.1177/0363546504273487
Marx RG, Hetsroni I (2012) Surgical technique: medial collateral ligament reconstruction using Achilles allograft for combined knee ligament injury. Clin Orthop Relat Res 470:798–805. doi:10.1007/s11999-011-1941-8
Dandy DJ, Gray AJ (1994) Anterior cruciate ligament reconstruction with the Leeds-Keio prosthesis plus extra-articular tenodesis. Results after six years. J Bone Joint Surg Br 76:193–197
Ghalayini SR, Helm AT, Bonshahi AY, Lavender A, Johnson DS, Smith RB (2010) Arthroscopic anterior cruciate ligament surgery: results of autogenous patellar tendon graft versus the Leeds-Keio synthetic graft five year follow-up of a prospective randomised controlled trial. Knee 17:334–339. doi:10.1016/j.knee.2009.09.008
Murray AW, Macnicol MF (2004) 10–16 year results of Leeds-Keio anterior cruciate ligament reconstruction. Knee 11:9–14. doi:10.1016/s0968-0160(03)00076-0
Rading J, Peterson L (1995) Clinical experience with the Leeds-Keio artificial ligament in anterior cruciate ligament reconstruction. A prospective two-year follow-up study. Am J Sports Med 23:316–319
Bostman OM (1998) Osteoarthritis of the ankle after foreign-body reaction to absorbable pins and screws: a three- to nine-year follow-up study. J Bone Joint Surg Br 80:333–338
Inui A, Kokubu T, Makino T, Nagura I, Toyokawa N, Sakata R, Kotera M, Nishino T, Fujioka H, Kurosaka M (2010) Potency of double-layered poly L-lactic acid scaffold in tissue engineering of tendon tissue. Int Orthop 34:1327–1332. doi:10.1007/s00264-009-0917-8
Sasaki K, Kuroda R, Ishida K, Kubo S, Matsumoto T, Mifune Y, Kinoshita K, Tei K, Akisue T, Tabata Y, Kurosaka M (2008) Enhancement of tendon-bone osteointegration of anterior cruciate ligament graft using granulocyte colony-stimulating factor. Am J Sports Med 36:1519–1527. doi:10.1177/0363546508316282
Kawakami H, Shino K, Hamada M, Nakata K, Nakagawa S, Nakamura N, Toritsuka Y, Yoshikawa H, Ochi T (2004) Graft healing in a bone tunnel: bone-attached graft with screw fixation versus bone-free graft with extra-articular suture fixation. Knee Surg Sports Traumatol Arthrosc 12:384–390. doi:10.1007/s00167-003-0484-2
Fukui N, Katsuragawa Y, Sakai H, Oda H, Nakamura K (1998) Effect of local application of basic fibroblast growth factor on ligament healing in rabbits. Rev Rhum Engl Ed 65:406–414
Irie T, Majima T, Sawaguchi N, Funakoshi T, Nishimura S, Minami A (2011) Biomechanical and histologic evaluation of tissue engineered ligaments using chitosan and hyaluronan hybrid polymer fibers: a rabbit medial collateral ligament reconstruction model. J Biomed Mater Res A 97:111–117. doi:10.1002/jbm.a.32938
Fan H, Liu H, Wong EJ, Toh SL, Goh JC (2008) In vivo study of anterior cruciate ligament regeneration using mesenchymal stem cells and silk scaffold. Biomaterials 29:3324–3337. doi:10.1016/j.biomaterials.2008.04.012
Yokoya S, Mochizuki Y, Natsu K, Omae H, Nagata Y, Ochi M (2012) Rotator cuff regeneration using a bioabsorbable material with bone marrow-derived mesenchymal stem cells in a rabbit model. Am J Sports Med 40:1259–1268. doi:10.1177/0363546512442343
Ikeda R, Fujioka H, Nagura I, Kokubu T, Toyokawa N, Inui A, Makino T, Kaneko H, Doita M, Kurosaka M (2009) The effect of porosity and mechanical property of a synthetic polymer scaffold on repair of osteochondral defects. Int Orthop 33:821–828. doi:10.1007/s00264-008-0532-0
Chen K, Sahoo S, He P, Ng KS, Toh SL, Goh JC (2012) A hybrid silk/RADA-based fibrous scaffold with triple hierarchy for ligament regeneration. Tissue Eng Part A 18:1399–1409. doi:10.1089/ten.TEA.2011.0376
Aoki M, Miyamoto S, Okamura K, Yamashita T, Ikada Y, Matsuda S (2004) Tensile properties and biological response of poly(L-lactic acid) felt graft: an experimental trial for rotator-cuff reconstruction. J Biomed Mater Res B Appl Biomater 71:252–259. doi:10.1002/jbm.b.30084
Barber JG, Handorf AM, Allee TJ, Li WJ (2011) Braided nanofibrous scaffold for tendon and ligament tissue engineering. Tissue Eng Part A. doi:10.1089/ten.tea.2010.0538
Sahoo S, Toh SL, Goh JC (2010) A bFGF-releasing silk/PLGA-based biohybrid scaffold for ligament/tendon tissue engineering using mesenchymal progenitor cells. Biomaterials 31:2990–2998. doi:10.1016/j.biomaterials.2010.01.004
Kimura A, Aoki M, Fukushima S, Ishii S, Yamakoshi K (2003) Reconstruction of a defect of the rotator cuff with polytetrafluoroethylene felt graft. Recovery of tensile strength and histocompatibility in an animal model. J Bone Joint Surg Br 85:282–287
Kawai T, Yamada T, Yasukawa A, Koyama Y, Muneta T, Takakuda K (2010) Anterior cruciate ligament reconstruction using chitin-coated fabrics in a rabbit model. Artif Organs 34:55–64. doi:10.1111/j.1525-1594.2009.00786.x
Lu HH, Cooper JA Jr, Manuel S, Freeman JW, Attawia MA, Ko FK, Laurencin CT (2005) Anterior cruciate ligament regeneration using braided biodegradable scaffolds: in vitro optimization studies. Biomaterials 26:4805–4816. doi:10.1016/j.biomaterials.2004.11.050
Okuno H, Tanaka J, Fujioka H, Maruo S, Makino T, Watanabe Y (2002) Evaluation of an interference screw for tendon reattachment to small bones. J Orthop Trauma 16:418–421
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nishimoto, H., Kokubu, T., Inui, A. et al. Ligament regeneration using an absorbable stent-shaped poly-l-lactic acid scaffold in a rabbit model. International Orthopaedics (SICOT) 36, 2379–2386 (2012). https://doi.org/10.1007/s00264-012-1660-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-012-1660-0