Abstract
Background
Abusive head trauma (AHT) is an important cause of morbidity in infants. Identifying which well-appearing infants are at risk for AHT and need neuroimaging is challenging, and concern about radiation exposure limits the use of head CT. Availability of an MRI protocol that is highly sensitive for intracranial hemorrhage would allow for AHT screening of well-appearing infants without exposing them to radiation.
Objective
To develop a screening MRI protocol to identify intracranial hemorrhage in well-appearing infants at risk for AHT.
Materials and methods
Infants enrolled in a parent study of well-appearing infants at increased risk for AHT were eligible for the current study if they underwent both head CT and conventional brain MRI. A derivation cohort of nine infants with AHT was used to identify sequences that provided the highest sensitivity for intracranial hemorrhage. A validation cohort of 78 infants including both controls with normal neuroimaging and cases with AHT was used to evaluate the accuracy of the selected sequences.
Results
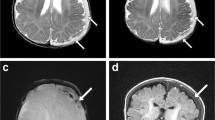
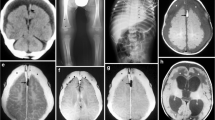
Three pulse sequences — axial T2, axial gradient recalled echo (GRE) and coronal T1-W inversion recovery — were 100% sensitive for intracranial hemorrhage in the derivation cohort. The same sequences were 100% sensitive (25/25) and 83% specific (44/53) for intracranial hemorrhage in the validation cohort.
Conclusion
A screening MRI protocol including axial T2, axial GRE and coronal T1-W inversion recovery sequences is highly sensitive for intracranial hemorrhage and may be useful as a screening tool to differentiate well-appearing infants at risk for AHT who should undergo head CT from those who can safely be discharged without head CT. Additional research is needed to evaluate the feasibility of this approach in clinical practice.



Similar content being viewed by others
References
Sieswerda-Hoogendoorn T, Bilo RA, van Duurling LL et al (2013) Abusive head trauma in young children in the Netherlands: evidence for multiple incidents of abuse. Acta Paediatr 102:e497–e501
Petska HW, Sheets LK, Knox BL (2013) Facial bruising as a precursor to abusive head trauma. Clin Pediatr 52:86–88
Oral R, Yagmur F, Nashelsky M et al (2008) Fatal abusive head trauma cases: consequence of medical staff missing milder forms of physical abuse. Pediatr Emerg Care 24:816–821
Ricci L, Giantris A, Merriam P et al (2003) Abusive head trauma in Maine infants: medical, child protective, and law enforcement analysis. Child Abuse Negl 27:271–283
Jenny C, Hymel KP, Ritzen A et al (1999) Analysis of missed cases of abusive head trauma. JAMA 281:621–626
Sieswerda-Hoogendoorn T, Boos S, Spivack B et al (2012) Abusive head trauma part II: radiological aspects. Eur J Pediatr 171:617–623
Ginde AA, Foianini A, Renner DM et al (2008) Availability and quality of computed tomography and magnetic resonance imaging equipment in U.S. emergency departments. Acad Emerg Med 15:780–783
Keenan HT, Runyan DK, Marshall SW et al (2004) A population-based comparison of clinical and outcome characteristics of young children with serious inflicted and noninflicted traumatic brain injury. Pediatrics 114:633–639
Sieswerda-Hoogendoorn T, Boos S, Spivack B et al (2012) Educational paper: abusive head trauma part I. Clinical aspects. Eur J Pediatr 171:415–423
Menoch MJ, Hirsh DA, Khan NS et al (2012) Trends in computed tomography utilization in the pediatric emergency department. Pediatrics 129:e690–e697
Brenner DJ, Hall EJ (2007) Computed tomography — an increasing source of radiation exposure. N Engl J Med 357:2277–2284
Bressan S, Romanato S, Mion T et al (2012) Implementation of adapted PECARN decision rule for children with minor head injury in the pediatric emergency department. Acad Emerg Med 19:801–807
Hennelly KE, Mannix R, Nigrovic LE et al (2013) Pediatric traumatic brain injury and radiation risks: a clinical decision analysis. J Pediatr 162:392–397
Foerster BR, Petrou M, Lin D et al (2009) Neuroimaging evaluation of non-accidental head trauma with correlation to clinical outcomes: a review of 57 cases. J Pediatr 154:573–577
Yu CK, Yuen VM, Wong GT et al (2013) The effects of anaesthesia on the developing brain: a summary of the clinical evidence. F1000Res 2:166
Kemp AM, Rajaram S, Mann M et al (2009) What neuroimaging should be performed in children in whom inflicted brain injury (iBI) is suspected? A systematic review. Clin Radiol 64:473–483
Patel DM, Tubbs RS, Pate G et al (2014) Fast-sequence MRI studies for surveillance imaging in pediatric hydrocephalus. J Neurosurg Pediatr 13:440–447
Iskandar BJ, Sansone JM, Medow J et al (2004) The use of quick-brain magnetic resonance imaging in the evaluation of shunt-treated hydrocephalus. J Neurosurg 101:147–151
Rozovsky K, Ventureyra EC, Miller E (2013) Fast-brain MRI in children is quick, without sedation, and radiation-free, but beware of limitations. J Clin Neurosci 20:400–405
Keenan HT, Runyan DK, Marshall SW et al (2003) A population-based study of inflicted traumatic brain injury in young children. JAMA 290:621–626
Hymel KP, Abshire TC, Luckey DW et al (1997) Coagulopathy in pediatric abusive head trauma. Pediatrics 99:371–375
Miglioretti DL, Johnson E, Williams A et al (2013) The use of computed tomography in pediatrics and the associated radiation exposure and estimated cancer risk. JAMA Pediatr 167:700–707
Acknowledgments
Data contained in this manuscript were presented at the following conferences: Annual Meeting of the Helfer Society, Annapolis, MD, April 6, 2014; Pediatric Academic Societies & Asian Society for Pediatric Research Joint Meeting, Vancouver, Canada, May 4, 2014; Society for Pediatric Radiology (SPR) Annual Meeting, Washington D.C., May 14, 2014. Funding was provided by the National Institutes of Health (NICHD R01HD055986).
We would like to thank Emily Heineman, Pamela Rubin and Marci Provins for their technical assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Rights and permissions
About this article
Cite this article
Flom, L., Fromkin, J., Panigrahy, A. et al. Development of a screening MRI for infants at risk for abusive head trauma. Pediatr Radiol 46, 519–526 (2016). https://doi.org/10.1007/s00247-015-3500-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-015-3500-z