Abstract
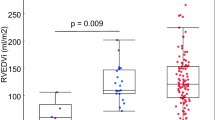
Initial surgical strategies in neonates with single left ventricular (LV) anatomy vary based on adequacy of pulmonary and systemic blood flow. Differing myocardial responses to these strategies, as reflected in indices of systolic function, ventricular size, and mass have not been well defined. We sought to evaluate single LV myocardial response to varied physiology and initial palliation and determine whether the response is consistent and predictable. Infants with single LV physiology were divided based on neonatal palliation: no palliation/PA band (NO); BT shunt only (BT); or Norwood procedure (NP). Echo measures were obtained at presentation, early post-bidirectional Glenn (BDG), late post-BDG follow-up, and post-Fontan procedure. Measures included ejection fraction, LV mass indexed to height2.7 and end diastolic volume indexed to body surface area, and mass/volume ratio. The cohort included 38 children (13 NO, 13 BT, 12 NP). Ejection fraction was similar but depressed in all groups at all stages. LV mass was higher in the NP group than the BT group at early post-BDG (p = 0.03) and higher than both BT and NO groups (p < 0.01) at late post-BDG, but the difference was resolved by post-Fontan follow-up. The NP group had the most remarkable remodeling in LV size from BDG to Fontan, suggesting that volume unloading is most valuable in this subgroup. Ventricular remodeling can be identified by echocardiography in children with single LV physiology, despite variable initial surgical palliative strategies. Importantly, these initial surgical strategies do not result in significant differences after Fontan palliation during early childhood.




Similar content being viewed by others
References
Webber SA, LeBlanc JG, Keeton BR, Salmon AP, Sandor GG, Lamb RK, Monro JL (1995) Pulmonary artery banding is not contraindicated in double inlet left ventricle with transposition and aortic arch obstruction. Eur J Cardiothorac Surg 9:515–520
Alsoufi B, Gillespie S, Kogon B, Schlosser B, Sachdeva R, Kim D, Clabby M, Kanter K (2015) Results of palliation with an initial modified Blalock–Taussig shunt in neonates with single ventricle anomalies associated with restrictive pulmonary blood flow. Ann Thorac Surg 99:1639–1646 (discussion 1646-7)
Williams JA, Bansal AK, Kim BJ, Nwakanma LU, Patel ND, Seth AK, Alejo DE, Gott VL, Vricella LA, Baumgartner WA, Cameron DE (2007) Two thousand Blalock–Taussig shunts: a six-decade experience. Ann Thorac Surg 84:2070–2075 (discussion 2070-5)
Ruzmetov M, Geiss DM, Fortuna RS (2013) Outcomes of double inlet left ventricle and similar morphologies: a single center comparison of initial pulmonary artery banding versus a norwood-type reconstruction. J Card Surg 28:569–575
Gaasch WH, Zile MR (2011) Left ventricular structural remodeling in health and disease: with special emphasis on volume, mass, and geometry. J Am Coll Cardiol 58:1733–1740
Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, Picard MH, Roman MJ, Seward J, Shanewise J, Solomon S, Spencer KT, St John Sutton M, Stewart W, American Society of Echocardiography’s Nomenclature and Standards Committee; Task Force on Chamber Quantification; American College of Cardiology Echocardiography Committee; American Heart Association; European Association of Echocardiography, European Society of Cardiology (2006) Recommendations for chamber quantification. Eur J Echocardiogr 7(2):79–108
Khoury PR, Mitsnefes M, Daniels SR, Kimball TR (2009) Age-specific reference intervals for indexed left ventricular mass in children. J Am Soc Echocardiogr 22:709–714
Lorenz CH (2000) The range of normal values of cardiovascular structures in infants, children, and adolescents measured by magnetic resonance imaging. Pediatr Cardiol 21:37–46
Frommelt PC, Guey LT, Minich LL, Bhat M, Bradley TJ, Colan SD, Ensing G, Gorentz J, Heydarian H, John JB, Lai WW, Levine JC, Mahle WT, Miller SG, Ohye RG, Pearson GD, Shirali GS, Wong PC, Cohen MS, Pediatric Heart Network Investigators (2012) Does initial shunt type for the Norwood procedure affect echocardiographic measures of cardiac size and function during infancy? The single ventricle reconstruction trial. Circulation 125:2630–2638
Frommelt PC, Gerstenberger E, Cnota JF, Cohen MS, Gorentz J, Hill KD, John JB, Levine JC, Lu J, Mahle WT, McCandless RT, Mertens L, Pearson GD, Spencer C, Thacker D, Williams IA, Wong PC, Newburger JW, Pediatric Heart Network Investigators (2014) Impact of initial shunt type on cardiac size and function in children with single right ventricle anomalies before the Fontan procedure: the single ventricle reconstruction extension trial. J Am Coll Cardiol 64:2026–2035
Sano T, Ogawa M, Yabuuchi H, Matsuda H, Nakano S, Shimazaki Y, Taniguchi K, Arisawa J, Hirose H, Kawashima Y (1988) Quantitative cineangiographic analysis of ventricular volume and mass in patients with single ventricle: relation to ventricular morphologies. Circulation 77:62–69
Isabella G, Daliento L, Chioin R, Milanesi O, Razzolini R, Dalla Volta S (1988) Left ventricular size and function in double inlet left ventricle. Int J Cardiol 21:43–49
Grosse-Wortmann L, Al-Otay A, Yoo SJ (2009) Aortopulmonary collaterals after bidirectional cavopulmonary connection or Fontan completion: quantification with MRI. Circ Cardiovasc Imaging 2:219–225
Fogel MA, Weinberg PM, Hoydu AK, Hubbard AM, Rychik J, Jacobs ML, Fellows KE, Haselgrove J (1997) Effect of surgical reconstruction on flow profiles in the aorta using magnetic resonance blood tagging. Ann Thorac Surg 63:1691–1700
Fogel MA, Li C, Nicolson SC, Spray TL, Gaynor JW, Fuller S, Keller MS, Harris MA, Yoganathan AP, Whitehead KK (2014) Comparison by magnetic resonance phase contrast imaging of pulse-wave velocity in patients with single ventricle who have reconstructed aortas versus those without. Am J Cardiol 114:1902–1907
Oparil S, Bishop SP, Clubb FJ Jr (1984) Myocardial cell hypertrophy or hyperplasia. Hypertension 6:III38–III43
Anversa P, Olivetti G, Loud AV (1980) Morphometric study of early postnatal development in the left and right ventricular myocardium of the rat. I. Hypertrophy, hyperplasia, and binucleation of myocytes. Circ Res 46:495–502
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest or financial disclosures to reveal as part of this study.
Rights and permissions
About this article
Cite this article
Horriat, N.L., Deatsman, S.L., Stelter, J. et al. Variable Myocardial Response to Load Stresses in Infants with Single Left Ventricular Anatomy: Influence of Initial Physiology and Surgical Palliative Strategy. Pediatr Cardiol 37, 1569–1574 (2016). https://doi.org/10.1007/s00246-016-1471-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-016-1471-y