Abstract
Background
Surgical wound infections are a significant problem and may interfere with healing. There is no uniform data in the literature regarding the rate of infection among the resection of skin tumors and the benefit of antibiotic prophylaxis. This study evaluated the effectiveness of antibiotic prophylaxis with cefazolin in resections of nonmelanocytic skin tumors and whether the histological type and ulceration is related to the rate of wound infection.
Methods
Two hundred and twenty-seven patients undergoing non-melanocytic skin tumor resection were randomly divided into two groups: group I without antibiotic prophylaxis of surgical site infection, and group II with intravenous cefazolin prophylaxis. Authors looked for surgical wound infection during a month of follow-up. Comparison intra and extra groups were made considering the tumor histology, and if it was ulcerated or not to surgical site infection.
Results
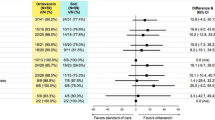
The infection rate in the sample was 25 lesions (12.01 %). Antibiotic prophylaxis proved to be effective in ulcerative lesions, and the infection rate was reduced from 12 cases (30 %) to 3 cases (9.85 %) (p Fisher = 0.04; RRR = 0.61; NNT = 4.80) but was not associated with reduced infection rates in any histological type.
Conclusions
Antibiotic prophylaxis was effective in preventing wound infection in ulcerated non-melanocytic skin tumor.
Level of Evidence: Level I, therapeutic study.
Similar content being viewed by others
References
Silver A, Eichorn A, Kral J, et al. (1996) Timeliness and use of antibiotic prophylaxis in selected inpatient surgical procedures. The antibiotic prophylaxis study group. Am J Surg 171(6):548–552
Nichols RL, Florman S (2001) Clinical presentations of soft-tissue infections and surgical site infections. Clin Infect Dis 33(Suppl 2):S84–S93
Wright TI, Baddour LM, Berbari EF, et al. (2008) Antibiotic prophylaxis in dermatologic surgery: advisory statement 2008. J Am Acad Dermatol 59(3):464–473
Kaiser AB, Clayson KR, Mulherin JL Jr, et al. (1978) Antibiotic prophylaxis in vascular surgery. Ann Surg 188(3):283–289
Futoryan T, Grande D (1995) Postoperative wound infection rates in dermatologic surgery. Dermatol Surg 21(6):509–514
Burke JF (1961) The effective period of preventive antibiotic action in experimental incisions and dermal lesions. Surgery 50:161–168
Ross CB, Wheeler WG, Jones MJ, Kerins CA, Peek TE (1997) Ceftriaxone versus cefazolin in peripheral arterial operations: a randomized, prospective trial. South Med J 90(1):16–22
Edwards WH Jr, Kaiser AB, Tapper S, et al. (1993) Cefamandole versus cefazolin in vascular surgical wound infection prophylaxis: cost-effectiveness and risk factors. J Vasc Surg 18(3):470–475
Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR (1999) Guideline for prevention of surgical site infection, 1999. Centers for Disease Control and Prevention (CDC) hospital infection control practices advisory committee. Am J Infect Control 27(2):97–132
Cranny G, Elliott R, Weatherly H, et al. (2008) A systematic review and economic model of switching from non-glycopeptide to glycopeptide antibiotic prophylaxis for surgery. Health Technol Assess 12(1):1–147
Webster J, Osborne S (2015) Preoperative bathing or showering with skin antiseptics to prevent surgical site infection. Cochrane Database Syst Rev 2:CD004985
Tanner J, Norrie P, Melen K (2011) Preoperative hair removal to reduce surgical site infection. Cochrane Database Syst Rev (11):CD004122
Heal CF, Buettner PG, Cruickshank R, et al. (2009) Does single application of topical chloramphenicol to high risk sutured wounds reduce incidence of wound infection after minor surgery? Prospective randomised placebo controlled double blind trial. BMJ 338:a2812
Hart D, Postlethwait RW, Brown IW Jr, Smith WW, Johnson PA (1968) Postoperative wound infections: a further report on ultraviolet irradiation with comments on the recent (1964) national research council cooperative study report. Ann Surg 167(5):728–743
Culver DH, Horan TC, Gaynes RP, et al. (1991) Surgical wound infection rates by wound class, operative procedure, and patient risk index. National Nosocomial Infections Surveillance System. Am J Med 91(3B):152S–157S
Cruse PJ, Foord R (1980) The epidemiology of wound infection. A 10-year prospective study of 62, 939 wounds. Surg Clin North Am 60(1):27–40
Enzler MJ, Berbari E, Osmon DR (2011) Antimicrobial prophylaxis in adults. Mayo Clin Proc 86(7):686–701
Zhang Y, Dong J, Qiao Y, He J, Wang T, Ma S (2014) Efficacy and safety profile of antibiotic prophylaxis usage in clean and clean-contaminated plastic and reconstructive surgery: a meta-analysis of randomized controlled trials. Ann Plast Surg 72(1):121–130
Heal CF, Buettner PG, Drobetz H (2012) Risk factors for surgical site infection after dermatological surgery. Int J Dermatol 51(7):796–803
Heal C, Buettner P, Browning S (2006) Risk factors for wound infection after minor surgery in general practice. Med J Aust 185(5):255–258
Bowater RJ, Stirling SA, Lilford RJI (2009) Antibiotic prophylaxis in surgery a generally effective intervention? Testing a generic hypothesis over a set of meta-analyses. Ann Surg 249(4):551–556
Rogers HD, Desciak EB, Marcus RP, Wang S, MacKay-Wiggan J, Eliezri YD (2010) Prospective study of wound infections in Mohs micrographic surgery using clean surgical technique in the absence of prophylactic antibiotics. J Am Acad Dermatol 63(5):842–851
Hurst EA, Grekin RC, SS Y, Neuhaus IM (2007) Infectious complications and antibiotic use in dermatologic surgery. Semin Cutan Med Surg 26(1):47–53
Karegoudar JS, Prabhakar PJ, Vijayanath V, Anitha MR, Surpur RR, Patil VM (2012) Shaving versus depilation cream for pre-operative skin preparation. Indian J Surg 74(4):294–297
Levender MM, Davis SA, Kwatra SG, Williford PM, Feldman SR (2012) Use of topical antibiotics as prophylaxis in clean dermatologic procedures. J Am Acad Dermatol 66(3):445–451
McHugh SM, Corrigan MA, Dimitrov BD, et al. (2011) Preventing infection in general surgery: improvements through education of surgeons by surgeons. J Hosp Infect 78(4):312–316
Lathlean S (1999) Skin cancer in general practice in South Australia. A five year study. Aust Fam Physician 28(Suppl 1):S28–S31
Sorensen LT Wound healing and infection in surgery: the pathophysiological impact of smoking, smoking cessation, and nicotine replacement therapy: a systematic review. Ann Surg 255(6):1069–1079
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Rodrigo Dreher, Juliana Tenório, Ygor Ferrão, Pedro Ely declare that they have no conflict of interest.
Patient consent
Patients provided written consent before their inclusion in this study.
Ethical standards
This study is in accordance with the Declaration of Helsinki regarding research on human beings and approved by a local board (CAAE 30780914100005335).
Funding
None
Rights and permissions
About this article
Cite this article
Dreher, R., Tenório, J.L.C., Ferrão, Y.A. et al. Antibiotic prophylaxis with cefazolin in reducing the infection rate of non-melanocytic skin tumors: a randomized clinical trial. Eur J Plast Surg 40, 133–136 (2017). https://doi.org/10.1007/s00238-016-1240-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00238-016-1240-4