Abstract
Purpose
To investigate imaging features of crossed cerebellar diaschisis (CCD) in cerebral gliomas, and its underlying pathophysiological mechanisms.
Methods
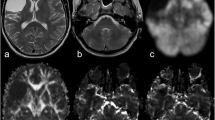
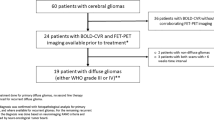
Thirty-three pre-surgical patients with cerebral gliomas and 33 healthy controls underwent arterial spin-labeling, diffusion tensor imaging, and high-resolution T1-weighted imaging using MRI, in order to estimate cerebral blood flow (CBF), white matter integrity, and lesion volume, respectively. Asymmetry indices of CBF in the cerebellum were used for evaluating the level of CCD in the patients. These indices were correlated with clinical variables (lesion size and position, tumor histological grade, and CBF asymmetry) and diffusion tensor imaging parameters (fractional anisotropy and number of fibers in the cortico-ponto-cerebellar pathway and across the cerebral hemispheres), respectively.
Results
The patients showed decreased CBF in the cerebellar hemisphere contralateral to the supratentorial tumor, and increased CBF asymmetry in the cerebellum (both P < 0.05). CCD levels in high-grade gliomas were higher than those of low-grade gliomas (P < 0.05). CCD levels were negatively correlated with the size of the supratentorial lesions, and positively correlated with FA asymmetry in the cerebral fibers (both P < 0.05).
Conclusions
CCD in cerebral gliomas was specifically associated with tumor histological grade, lesion size, and white matter impairments in the hemisphere ipsilateral to the tumor. The findings implicated that observing CCD might have potential for assisting grading diagnosis of cerebral gliomas.





Similar content being viewed by others
Abbreviations
- CCD:
-
crossed cerebellar diaschisis
- CPC:
-
cortico-ponto-cerebellar
- 3D ASL:
-
three-dimensional arterial spin labeling
- DTI:
-
diffusion tensor imaging
- CBF:
-
cerebral blood flow
- FA:
-
fractional anisotropy
- AI:
-
asymmetry index
References
Lin D, Kleinman J, Wityk R et al (2009) Crossed cerebellar diaschisis in acute stroke detected by dynamic susceptibility contrast MR perfusion imaging. AJNR Am J Neuroradiol 30:710–715
Szilágyi G, Vas A, Kerényi L, Nagy Z, Csiba L, Gulyás B (2012) Correlation between crossed cerebellar diaschisis and clinical neurological scales. Acta Neurol Scand 125:373–381
Jeon YW, Kim SH, Lee JY, Whang K, Kim MS, Kim YJ, Lee MS, Brain Research Group (2012) Dynamic CT perfusion imaging for the detection of crossed cerebellar diaschisis in acute ischemic stroke. Korean J Radiol 13:12–19
Mahale R, Mehta A, Rangasetty S (2015) Crossed cerebellar diaschisis due to Rasmussen encephalitis. Pediatr Neurol 53:272–273
Cianfoni A, Luigetti M, Bradshaw ML, Welsh CT, Edwards J, Glazier S (2010) MRI findings of crossed cerebellar diaschisis in a case of Rasmussen’s encephalitis. J Neurol 257:1748–1750
Ohe Y, Hayashi T, Deguchi I et al (2013) A case of nonconvulsive status epilepticus with a reversible contralateral cerebellar lesion: temporal changes in magnetic resonance imaging and single-photon emission computed tomography finding. J Stroke Cerebrovasc Dis 22:e639-e642
Teoh EJ, Green AL, Bradley KM (2014) Crossed cerebellar diaschisis due to cerebral diffuse large B cell lymphoma on 18F-FDG PET/CT. Int J Hematol 100:415–416
Calabria F, Schillaci O (2012) Recurrent glioma and crossed cerebellar diaschisis in a patient examined with 18F-DOPA and 18F-FDG PET/CT. Clin Nucl Med 37:878–879
Feeney DM, Baron JC (1986) Diaschisis. Stroke 17:817–830
Baron JC, Bousser MG, Comar D, Castaigne P (1981) “Crossed cerebellar diaschisis” in human supratentorial brain infarction. Trans Am Neurol Assoc 105:459–461
Kamouchi M, Fujishima M, Saku Y, Ibayashi S, Iida M (2004) Crossed cerebellar hypoperfusion in hyperacute ischemic stroke. J Neurol Sci 225:65–69
Serteser M, Ozben T, Gümüslü S, Balkan S, Balkan E (2001) Biochemical evidence of crossed cerebellar diaschisis in terms of nitric oxide indicators and lipid peroxidation products in rats during focal cerebral ischemia. Acta Neurol Scand 103:43–48
Komaba Y, Mishina M, Utsumi K, Katayama Y, Kobayashi S, Mori O (2004) Crossed cerebellar diaschisis in patients with cortical infarction logistic regression analysis to control for confounding effects. Stroke 35:472–476
Madai VI, Altaner A, Stengl KL, Zaro-Weber O, Heiss WD, von Samson-Himmelstjerna FC, Sobesky J (2011) Crossed cerebellar diaschisis after stroke: can perfusion-weighted MRI show functional inactivation? J Cereb Blood Flow Metab 31:1493–1500
Liu Y, Karonen JO, Nuutinen J, Vanninen E, Kuikka JT, Vanninen RL (2007) Crossed cerebellar diaschisis in acute ischemic stroke: a study with serial SPECT and MRI. J Cereb Blood Flow Metab 27:1724–1732
Chen S, Guan M, Lian HJ, Ma LJ, Shang JK, He S, Ma MM, Zhang ML, Li ZY, Wang MY, Shi DP, Zhang JW (2014) Crossed cerebellar diaschisis detected by arterial spin-labeled perfusion magnetic resonance imaging in subacute ischemic stroke. J Stroke Cerebrovasc Dis 23:2378–2383
Pantano P, Baron JC, Samson Y et al (1986) Crossed cerebellar diaschisis. Further studies. Brain 109:677–694
Meyer JS, Obara K, Muramatsu K (1993) Diaschisis. Neurol Res 15:362–366
Otte A, Roelcke U, von Ammon K, Hausmann O, Maguire RP, Missimer J, Müller-Brand J, Radü EW, Leenders KL (1998) Crossed cerebellar diaschisis and brain tumor biochemistry studied with positron emission tomography,[18 F] fluorodeoxyglucose and [11 C] methionine. J Neurol Sci 156:73–77
Kang KM, Sohn CH, Kim BS, Kim YI, Choi SH, Yun TJ, Kim JH, Park SW, Cheon GJ, Han MH (2015) Correlation of asymmetry indices measured by arterial spin-labeling MR imaging and SPECT in patients with crossed cerebellar diaschisis. AJNR Am J Neuroradiol 36:1662–1668
Förster A, Kerl HU, Goerlitz J, Wenz H, Groden C (2014) Crossed cerebellar diaschisis in acute isolated thalamic infarction detected by dynamic susceptibility contrast perfusion MRI. PLoS One 9:e88044
Noguchi T, Nishihara M, Egashira Y, Azama S, Hirai T, Kitano I, Yakushiji Y, Kawashima M, Irie H (2015) Arterial spin-labeling MR imaging of cerebral hemorrhages. Neuroradiology 57:1135–1144
Kang KM, Sohn CH, Choi SH, Jung KH, Yoo RE, Yun TJ, Kim JH, Park SW (2017) Detection of crossed cerebellar diaschisis in hyperacute ischemic stroke using arterial spin-labeled MR imaging. PLoS One 12(3):e0173971
Nocuń A, Wojczal J, Szczepańska-Szerej H, Wilczyński M, Chrapko B (2013) Quantitative evaluation of crossed cerebellar diaschisis, using voxel-based analysis of Tc-99m ECD brain SPECT. Nucl Med Rev Cent East Eur 16:31–34
Kim J, Lee SK, Lee JD, Kim YW, Kim DI (2005) Decreased fractional anisotropy of middle cerebellar peduncle in crossed cerebellar diaschisis: diffusion-tensor imaging-positron-emission tomography correlation study. AJNR Am J Neuroradiol 26:2224–2228
Gold L, Lauritzen M (2002) Neuronal deactivation explains decreased cerebellar blood flow in response to focal cerebral ischemia or suppressed neocortical function. Proc Natl Acad Sci U S A 99:7699–7704
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Funding
This study was funded by the Natural Science Foundation of China (Grant no. 81530054), the Chinese Post-Doctor Foundation (2016M603064), the Post-Doctor Foundation Jiangsu province (1501169B), Key Talents Project of Jiangsu Province (Grant nos. ZDRCA2016093), Independent Research Project in State Key Laboratory of Analytical Chemistry for Life Science (Grant nos. 5431ZZXM1716) and the Wellcome Trust (Grant no. 101253/Z/13/Z).
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Liu, X., Li, J., Xu, Q. et al. Pathological factors contributing to crossed cerebellar diaschisis in cerebral gliomas: a study combining perfusion, diffusion, and structural MR imaging. Neuroradiology 60, 643–650 (2018). https://doi.org/10.1007/s00234-018-2015-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-018-2015-3