Abstract
Background
Four times daily dosing (qid) with a proton pump inhibitor can cause rapid increase in intragastric pH. We investigated the efficacy of the front-loading with rabeprazole 10 mg qid on a subsequent regimen with rabeprazole 10 mg twice daily (bid) for 7 days in extensive metabolizers (EMs) of CYP2C19.
Methods
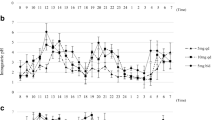
Five EMs received three different 1-week regimens in a crossover manner as follows: (1) rabeprazole 10 mg bid for 7 days; (2) a front-loading regimen of rabeprazole (rabeprazole 10 mg qid on day 0 and bid on days 1 to 7); and (3) rabeprazole 10 mg qid for 7 days. Five intermediate metabolizers (IMs) and four poor metabolizers (PMs) received rabeprazole 10 mg bid regimen only. Twenty-four-hour intragastric pH-monitorings were performed on days 1, 4, and 7. Area under the intragastric pH-time curves (AUCs) from days 1 to 7 was calculated using 24-h median intragastric pHs on days 1, 4, and 7.
Results
Twenty-four-hour intragastric pHs in the front-loading group on days 1, 4, and 7 were 5.1, 4.9, and 5.1, respectively. The median AUC with front-loading in EMs (34.4, pH·day) was significantly higher than that in EMs with rabeprazole 10 mg bid (30.74, p = 0.043). No statistically significant differences in median AUCs were noted among front-loading in EMs, rabeprazole 10 mg qid in EMs (37.2), rabeprazole 10 mg bid in IMs (37.3), and PMs (39.4).
Conclusions
The one-day front-loading regimen of rabeprazole 10 mg qid provided sufficient acid inhibition for 7 days, even in CYP2C19 EMs.






Similar content being viewed by others
Abbreviations
- EM:
-
Extensive metabolizer
- H. pylori :
-
Helicobacter pylori
- IM:
-
Intermediate metabolizer
- PPI:
-
Proton pump inhibitor
- PM:
-
Poor metabolizer
References
Walsh JH, Peterson WL (1995) The treatment of Helicobacter pylori infection in the management of peptic ulcer disease. N Engl J Med 333(15):984–991
Furuta T et al (2002) Effect of cytochrome P4502C19 genotypic differences on cure rates for gastroesophageal reflux disease by lansoprazole. Clin Pharmacol Ther 72(4):453–460
Furuta T et al (2005) Influence of CYP2C19 polymorphism and Helicobacter pylori genotype determined from gastric tissue samples on response to triple therapy for H. pylori infection. Clin Gastroenterol Hepatol 3(6):564–573
Sugimoto M et al (2007) Evidence that the degree and duration of acid suppression are related to Helicobacter pylori eradication by triple therapy. Helicobacter 12(4):317–323
Current European concepts in the management of Helicobacter pylori infection. The maastricht consensus report (1997) European Helicobacter pylori study group. Gut 41(1):8–13
Asaka M et al (2010) Guidelines for the management of Helicobacter pylori infection in Japan: 2009 revised edition. Helicobacter 15(1):1–20
Satoh K (2002) Indications for Helicobacter pylori eradication therapy and first-line therapy regimen in Japan: recommendation by the Japanese Society for Helicobacter Research. J Gastroenterol 37(Suppl 13):34–38
Grayson ML et al (1989) Effect of varying pH on the susceptibility of Campylobacter pylori to antimicrobial agents. Eur J Clin Microbiol Infect Dis 8(10):888–889
Hunt RH (1993) pH and Hp–gastric acid secretion and Helicobacter pylori: implications for ulcer healing and eradication of the organism. Am J Gastroenterol 88(4):481–483
Heifets LB, Lindholm-Levy PJ, Comstock RD (1992) Clarithromycin minimal inhibitory and bactericidal concentrations against Mycobacterium avium. Am Rev Respir Dis 145(4 Pt 1):856–858
Scott D et al (1998) The life and death of Helicobacter pylori. Gut 43(Suppl 1):S56–S60
Scott DR et al (1998) The role of internal urease in acid resistance of Helicobacter pylori. Gastroenterology 114(1):58–70
Marcus EA et al (2012) The effects of varying acidity on Helicobacter pylori growth and the bactericidal efficacy of ampicillin. Aliment Pharmacol Ther 36(10):972–979
Sohn DR et al (1992) Disposition kinetics and metabolism of omeprazole in extensive and poor metabolizers of S-mephenytoin 4′-hydroxylation recruited from an Oriental population. J Pharmacol Exp Ther 262(3):1195–1202
Chiba K et al (1993) Oxidative metabolism of omeprazole in human liver microsomes: cosegregation with S-mephenytoin 4’-hydroxylation. J Pharmacol Exp Ther 266(1):52–59
Pearce RE et al (1996) Identification of the human P450 enzymes involved in lansoprazole metabolism. J Pharmacol Exp Ther 277(2):805–816
Sohn DR et al (1997) Metabolic disposition of lansoprazole in relation to the S-mephenytoin 4′-hydroxylation phenotype status. Clin Pharmacol Ther 61(5):574–582
Chang M et al (1995) Interphenotype differences in disposition and effect on gastrin levels of omeprazole—suitability of omeprazole as a probe for CYP2C19. Br J Clin Pharmacol 39(5):511–518
Kubota T, Chiba K, Ishizaki T (1996) Genotyping of S-mephenytoin 4′-hydroxylation in an extended Japanese population. Clin Pharmacol Ther 60(6):661–666
Ishizaki T, Horai Y (1999) Review article: cytochrome P450 and the metabolism of proton pump inhibitors–emphasis on rabeprazole. Aliment Pharmacol Ther 13(Suppl 3):27–36
Kurzawski M et al (2006) Effect of CYP2C19*17 gene variant on Helicobacter pylori eradication in peptic ulcer patients. Eur J Clin Pharmacol 62(10):877–880
Sugimoto K et al (2008) Limited frequency of the CYP2C19*17 allele and its minor role in a Japanese population. Br J Clin Pharmacol 65(3):437–439
Sugimoto M et al (2004) Different dosage regimens of rabeprazole for nocturnal gastric acid inhibition in relation to cytochrome P450 2C19 genotype status. Clin Pharmacol Ther 76(4):290–301
Sugimoto M et al (2005) Comparison of an increased dosage regimen of rabeprazole versus a concomitant dosage regimen of famotidine with rabeprazole for nocturnal gastric acid inhibition in relation to cytochrome P450 2C19 genotypes. Clin Pharmacol Ther 77(4):302–311
Shirai N et al (2001) Effects of CYP2C19 genotypic differences in the metabolism of omeprazole and rabeprazole on intragastric pH. Aliment Pharmacol Ther 15(12):1929–1937
Furuta T et al (1999) CYP2C19 genotype status and effect of omeprazole on intragastric pH in humans. Clin Pharmacol Ther 65(5):552–561
Furuta T et al (2001) Effect of genotypic differences in CYP2C19 on cure rates for Helicobacter pylori infection by triple therapy with a proton pump inhibitor, amoxicillin, and clarithromycin. Clin Pharmacol Ther 69(3):158–168
Sugimoto M et al (2014) Comparison of acid inhibition with standard dosages of proton pump inhibitors in relation to CYP2C19 genotype in Japanese. Eur J Clin Pharmacol 70(9):1073–1078
Yasuda S et al (1995) Comparison of the kinetic disposition and metabolism of E3810, a new proton pump inhibitor, and omeprazole in relation to S-mephenytoin 4′-hydroxylation status. Clin Pharmacol Ther 58(2):143–154
Horai Y et al (2001) Pharmacodynamic effects and kinetic disposition of rabeprazole in relation to CYP2C19 genotypes. Aliment Pharmacol Ther 15(6):793–803
Sugimoto M et al (2012) Rabeprazole 10 mg q.d.s. decreases 24-h intragastric acidity significantly more than rabeprazole 20 mg b.d. or 40 mg o.m., overcoming CYP2C19 genotype. Aliment Pharmacol Ther 36(7):627–634
Miehlke S et al (2003) A prospective, randomized study of quadruple therapy and high-dose dual therapy for treatment of Helicobacter pylori resistant to both metronidazole and clarithromycin. Helicobacter 8(4):310–319
Furuta T et al (2001) Effects of genotypic differences in CYP2C19 status on cure rates for Helicobacter pylori infection by dual therapy with rabeprazole plus amoxicillin. Pharmacogenetics 11(4):341–348
Furuta T et al (2003) High-dose rabeprazole/amoxicillin therapy as the second-line regimen after failure to eradicate H. pylori by triple therapy with the usual doses of a proton pump inhibitor, clarithromycin and amoxicillin. Hepato-Gastroenterology 50(54):2274–2278
Shirai N et al (2007) Dual therapy with high doses of rabeprazole and amoxicillin versus triple therapy with rabeprazole, amoxicillin, and metronidazole as a rescue regimen for Helicobacter pylori infection after the standard triple therapy. Eur J Clin Pharmacol 63(8):743–749
Suzuki S et al (2012) Development of a novel, fully-automated genotyping system: principle and applications. Sensors (Basel) 12(12):16614–16627
Furuta T et al (2007) Pharmacogenomics-based tailored versus standard therapeutic regimen for eradication of H. pylori. Clin Pharmacol Ther 81(4):521–528
Sahara S et al (2015) Potent gastric acid inhibition over 24 hours by 4-times daily dosing of esomeprazole 20 mg. Digestion 91(4):277–285
Zvyaga T et al (2012) Evaluation of six proton pump inhibitors as inhibitors of various human cytochromes P450: focus on cytochrome P450 2C19. Drug Metab Dispos 40(9):1698–1711
Saitoh T et al (2002) Effects of rabeprazole, lansoprazole and omeprazole on intragastric pH in CYP2C19 extensive metabolizers. Aliment Pharmacol Ther 16(10):1811–1817
Fock KM et al (2005) Rabeprazole vs esomeprazole in non-erosive gastro-esophageal reflux disease: a randomized, double-blind study in urban Asia. World J Gastroenterol 11(20):3091–3098
Ramsjo M et al (2010) CYP2C19 activity comparison between Swedes and Koreans: effect of genotype, sex, oral contraceptive use, and smoking. Eur J Clin Pharmacol 66(9):871–877
Conflicts of interest
The First Department of Medicine and the Center for Clinical Research at Hamamatsu University School of Medicine have received grants from Takeda Pharmaceutical Co., Ltd., AstraZeneca KK, Eisai Co., Ltd., and Daiichi-Sankyo Co. Ltd. The authors have no other conflicts of interest that are directly relevant to the content of this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kagami, T., Sugimoto, M., Ichikawa, H. et al. One-day front-loading with four doses of rabeprazole followed by a standard twice-daily regimen provides sufficient acid inhibition in extensive metabolizers of CYP2C19. Eur J Clin Pharmacol 71, 1467–1475 (2015). https://doi.org/10.1007/s00228-015-1941-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-015-1941-9