Abstract
Summary
The present study evaluates the incidence and mortality of vertebral fractures in Korea, using data from the Health Insurance Review Assessment Service, which includes nationwide information entrusted by Korean government.
Introduction
A vertebral compression fracture is a serious complication associated with osteoporosis of the spine. We evaluated the incidence of vertebral fracture and subsequent mortality in South Korea, using nationwide data from the Health Insurance Review and Assessment Service (HIRA).
Methods
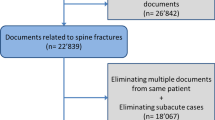
All new visits or admissions to clinics or hospitals for fractures were recorded in nationwide cohort by the Korean HIRA using International Classification of Disease, tenth Revision (ICD-10) code. The incidence of vertebral fracture and excess mortality associated with vertebral fracture were evaluated, in men and women aged 50 years or more between 2005 and 2008. Standardized mortality ratio (SMR) was calculated to determine excess mortality associated with vertebral fracture.
Results
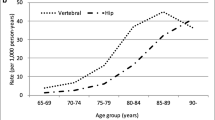
The crude overall incidence of vertebral fractures was 984 per 100,000 person years from 2005 to 2008. The overall mortality rate at 3 months, 6 months, 1 year, and 2 years after vertebral fracture in men (5.56%, 9.41%, 14.6%, and 20.61%, respectively) were higher than that in women (2.41%, 4.36%, 7.16%, and 10.48%, respectively). In both genders, the age-specific mortality rates were more than those of the general population. The SMR was highest during the first 3 months and gradually declined to 2.53 in men and 1.86 in women at the 2-year period.
Conclusions
The incidence of vertebral fracture in South Korea was comparable with other countries such as Switzerland, and the mortality after vertebral fracture is higher than that of normal populations. The incidence of osteoporotic vertebral fracture and following high mortality are likely to become serious socioeconomic problems.

Similar content being viewed by others
References
Cheung G, Chow E, Holden L, Vidmar M, Danjoux C, Yee AJ, Connolly R, Finkelstein J (2006) Percutaneous vertebroplasty in patients with intractable pain from osteoporotic or metastatic fractures: a prospective study using quality-of-life assessment. Can Assoc Radiol J 57:13–21
Salaffi F, Cimmino MA, Malavolta N, Carotti M, Di Matteo L, Scendoni P, Grassi W (2007) The burden of prevalent fractures on health-related quality of life in postmenopausal women with osteoporosis: the IMOF study. J Rheumatol 34:1551–1560
Cooper C, Atkinson EJ, Jacobsen SJ, O’Fallon WM, Melton LJ 3rd (1993) Population-based study of survival after osteoporotic fractures. Am J Epidemiol 137:1001–1005
Ensrud KE, Thompson DE, Cauley JA, Nevitt MC, Kado DM, Hochberg MC, Santora AC 2nd, Black DM (2000) Prevalent vertebral deformities predict mortality and hospitalization in older women with low bone mass. Fracture Intervention Trial Research Group. J Am Geriatr Soc 48:241–249
Center JR, Nguyen TV, Schneider D, Sambrook PN, Eisman JA (1999) Mortality after all major types of osteoporotic fracture in men and women: an observational study. Lancet 353:878–882
Hasserius R, Karlsson MK, Nilsson BE, Redlund-Johnell I, Johnell O (2003) Prevalent vertebral deformities predict increased mortality and increased fracture rate in both men and women: a 10-year population-based study of 598 individuals from the Swedish cohort in the European Vertebral Osteoporosis Study. Osteoporos Int 14:61–68
Cauley JA, Thompson DE, Ensrud KC, Scott JC, Black D (2000) Risk of mortality following clinical fractures. Osteoporos Int 11:556–561
Kanis JA, Oden A, Johnell O, De Laet C, Jonsson B (2004) Excess mortality after hospitalisation for vertebral fracture. Osteoporos Int 15:108–112
Lau E, Ong K, Kurtz S, Schmier J, Edidin A (2008) Mortality following the diagnosis of a vertebral compression fracture in the Medicare population. J Bone Jt Surg Am 90:1479–1486
Bouza C, Lopez T, Palma M, Amate JM (2007) Hospitalised osteoporotic vertebral fractures in Spain: analysis of the national hospital discharge registry. Osteoporos Int 18:649–657
Gong HS, Oh WS, Chung MS, Oh JH, Lee YH, Baek GH (2009) Patients with wrist fractures are less likely to be evaluated and managed for osteoporosis. J Bone Jt Surg Am 91:2376–2380
Jee SH, Ohrr H, Sull JW, Yun JE, Ji M, Samet JM (2005) Fasting serum glucose level and cancer risk in Korean men and women. JAMA 293:194–202
Sung SK, Lee SG, Lee KS, Kim DS, Kim KH, Kim KY (2009) First-year treatment adherence among outpatients initiating antihypertensive medication in Korea: results of a retrospective claims review. Clin Ther 31:1309–1320
Kang HY, Yang KH, Kim YN, Moon SH, Choi WJ, Kang DR, Park SE (2010) Incidence and mortality of hip fracture among the elderly population in South Korea: a population-based study using the national health insurance claims data. BMC Publ Health 10:230
Korean Statistical Information Service. http://www.kosis.kr. Accessed Nov 24 2008
Richmond J, Aharonoff GB, Zuckerman JD, Koval KJ (2003) Mortality risk after hip fracture. J Orthop Trauma 17:53–56
Tsuboi M, Hasegawa Y, Suzuki S, Wingstrand H, Thorngren KG (2007) Mortality and mobility after hip fracture in Japan: a ten-year follow-up. J Bone Jt Surg Br 89:461–466
Ulm K (1990) A simple method to calculate the confidence interval of a standardized mortality ratio (SMR). Am J Epidemiol 131:373–375
Kanis JA, Burlet N, Cooper C, Delmas PD, Reginster JY, Borgstrom F, Rizzoli R (2008) European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int 19:399–428
Kanis JA, Johnell O, De Laet C, Jonsson B, Oden A, Ogelsby AK (2002) International variations in hip fracture probabilities: implications for risk assessment. J Bone Miner Res 17:1237–1244
Lippuner K, Johansson H, Kanis JA, Rizzoli R (2009) Remaining lifetime and absolute 10-year probabilities of osteoporotic fracture in Swiss men and women. Osteoporos Int 20:1131–1140
Kado DM, Browner WS, Palermo L, Nevitt MC, Genant HK, Cummings SR (1999) Vertebral fractures and mortality in older women: a prospective study. Study of Osteoporotic Fractures Research Group. Arch Intern Med 159:1215–1220
Ioannidis G, Papaioannou A, Hopman WM, Akhtar-Danesh N, Anastassiades T, Pickard L, Kennedy CC, Prior JC, Olszynski WP, Davison KS, Goltzman D, Thabane L, Gafni A, Papadimitropoulos EA, Brown JP, Josse RG, Hanley DA, Adachi JD (2009) Relation between fractures and mortality: results from the Canadian Multicentre Osteoporosis Study. CMAJ 181:265–271
Johnell O, Kanis JA, Oden A, Sernbo I, Redlund-Johnell I, Petterson C, De Laet C, Jonsson B (2004) Mortality after osteoporotic fractures. Osteoporos Int 15:38–42
Sanders KM, Seeman E, Ugoni AM, Pasco JA, Martin TJ, Skoric B, Nicholson GC, Kotowicz MA (1999) Age- and gender-specific rate of fractures in Australia: a population-based study. Osteoporos Int 10:240–247
Sakuma M, Endo N, Oinuma T, Endo E, Yazawa T, Watanabe K, Watanabe S (2008) Incidence and outcome of osteoporotic fractures in 2004 in Sado City, Niigata Prefecture, Japan. J Bone Miner Metab 26:373–378
Acknowledgements
This study was supported by the Korean Health Insurance Review and Assessment Service (HIRA) and conducted using data from the Korean National Health Insurance Claims Database.
Conflicts of interest
This study was supported by the Korean Health Insurance Review and Assessment Service (HIRA) and conducted using data from the Korean National Health Insurance Claims Database.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lee, YK., Jang, S., Jang, S. et al. Mortality after vertebral fracture in Korea. Osteoporos Int 23, 1859–1865 (2012). https://doi.org/10.1007/s00198-011-1833-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-011-1833-5