Abstract
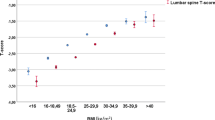
Low body mass index (BMI) is a well-documented risk factor for future fracture. The aim of this study was to quantify this effect and to explore the association of BMI with fracture risk in relation to age, gender and bone mineral density (BMD) from an international perspective using worldwide data. We studied individual participant data from almost 60,000 men and women from 12 prospective population-based cohorts comprising Rotterdam, EVOS/EPOS, CaMos, Rochester, Sheffield, Dubbo, EPIDOS, OFELY, Kuopio, Hiroshima, and two cohorts from Gothenburg, with a total follow-up of over 250,000 person years. The effects of BMI, BMD, age and gender on the risk of any fracture, any osteoporotic fracture, and hip fracture alone was examined using a Poisson regression model in each cohort separately. The results of the different studies were then merged. Without information on BMD, the age-adjusted risk for any type of fracture increased significantly with lower BMI. Overall, the risk ratio (RR) per unit higher BMI was 0.98 (95% confidence interval [CI], 0.97–0.99) for any fracture, 0.97 (95% CI, 0.96–0.98) for osteoporotic fracture and 0.93 (95% CI, 0.91–0.94) for hip fracture (all p <0.001). The RR per unit change in BMI was very similar in men and women ( p >0.30). After adjusting for BMD, these RR became 1 for any fracture or osteoporotic fracture and 0.98 for hip fracture (significant in women). The gradient of fracture risk without adjustment for BMD was not linearly distributed across values for BMI. Instead, the contribution to fracture risk was much more marked at low values of BMI than at values above the median. This nonlinear relation of risk with BMI was most evident for hip fracture risk. When compared with a BMI of 25 kg/m2, a BMI of 20 kg/m2 was associated with a nearly twofold increase in risk ratio (RR=1.95; 95% CI, 1.71–2.22) for hip fracture. In contrast, a BMI of 30 kg/m2, when compared with a BMI of 25 kg/m2, was associated with only a 17% reduction in hip fracture risk (RR=0.83; 95% CI, 0.69–0.99). We conclude that low BMI confers a risk of substantial importance for all fractures that is largely independent of age and sex, but dependent on BMD. The significance of BMI as a risk factor varies according to the level of BMI. Its validation on an international basis permits the use of this risk factor in case-finding strategies.



Similar content being viewed by others
References
Cummings SR, Nevitt MC, Browner WS, Stone K, Fox KM, Ensrud KE, Cauley J, Black D, Vogt TM (1995) Risk factors for hip fracture in white women. Study of Osteoporotic Fractures Research Group. N Engl J Med 332:767–773
Eddy DM, Johnston CC, Cummings SR, Dawson-Hughers B, Lindsay R, Melton LJ et al (1998) Osteoporosis: Review of the evidence for prevention, diagnosis and treatment and cost-effectiveness analysis. Osteoporos Int 8: [Suppl 4]
Honkanen RJ, Honkanen K, Kroger H, Alhava E, Tuppurainen M, Saarikoski S (2000) Risk factors for perimenopausal distal forearm fractures. Osteoporos Int 11:265–270
Galvard H, Elmstahl S, Elmstahl B, Samuelsson SM, Robertsson E (1996) Differences in body composition between female geriatric hip fracture patients and healthy controls: body fat is more important as explanatory factors for the fracture than body weight and lean body mass. Aging (Milano) 8:282–286
Joakimsen RM, Fonnebo V, Magnus JH, Tollan A, Sogaard AJ (1998) The Tromso study: body height, body mass index and fractures. Osteoporos Int 8:436–442
Turner LW, Faile PA, Tomlinson R (1999) Osteoporosis diagnosis and fracture. Orthop Nurs 18:21–27
Van der Voort DJ, Geusens PP, Dinant CJ (2001) Risk factors for osteoporosis related to their outcome: fractures. Osteoporos Int 12:630–638
Young Y, Myers AH, Provenzano G (2001) Factors associated with time to first hip fracture. J Aging Health 13:511–526
Roy DK, O’Neill TW, Finn JD, Lunt M, Silman AJ, Felsenberg D, Ambrecht G, Banzer D, Benevolenskaya LI, Bhalla A, Bruges Armas J, Cannata JB, Cooper C, Dequeker J, Eastell R, Yershova O, Felsch B, Gowin W, Havelka S, Hoszowski K, Jajic I, Janot J, Johnell O, Kanis JA, Krag G, Lopez Vaz A, Lorenc R, Lyritis G, Masaryk P, Matthis C, Miazgowski T, Gennari C, Pols HAP, Poor G, Raspe HH, Reid DM, Reisinger W, Scheidt-Nave C, Stepan J, Todd C, Weber K, Woolf AD, Reeve J (2003) Determinants of incident vertebral fracture in men and women: results from the European Prospective Osteoporosis Study (EPOS). Osteoporos Int 14; 19–26
Willig R, Luukinen H, Jalovaara P (2003) Factors related to occurrence of hip fractures during a fall on the hip. Public Health 117:25–30
World Health Organization (1998) Obesity. Preventing and managing the global epidemic. World Health Organization, Geneva
Mokdad AH, Bowman BA, Ford ES, Vinicor F, Marks JS, Koplan JP (2001) The continuing epidemics of obesity and diabetes in the United States. JAMA 286:1195–200
Peeters A, Barendregt JJ, Willekens F, Mackenbach JP, Al Mamun AA, Bonneux L; NEDCOM, the Netherlands Epidemiology and Demographic Compression of Morbidity Research Group (2003) Obesity in adulthood and its consequences for life expectancy: a life-table analysis. Ann Intern Med 138:24–32
Kanis JA, Delmas P, Burckhardt P, Cooper C, Torgerson D, on behalf of the European Foundation for Osteoporosis and Bone Disease (1997) Guidelines for diagnosis and management of osteoporosis. Osteoporos Int 7:390–406
Royal College of Physicians (1999) Clinical Guidelines for strategies to prevent and treat osteoporosis. Royal College of Physicians, London
Kwaliteitsinstituut voor de Gezondheidszorg CBP (2002) Osteoporose: tweede herziene richtlijn. Utrecht, the Netherlands. ISBN 90–76906–23–8
Johnell O, Gullberg B, Kanis JA, Allander E, Elffors L, Dequeker J, Dilsen G, Gennari C, Vaz AL, Lyritis G, Mazzuoli G, Miravet L, Passeri M, Cano RP, Rapado A, Ribot C (1995) Risk factors for hip fracture in European women—the Medos Study. J Bone Miner Res 10:1802–1815
Kanis J, Johnell O, Gullberg B, Allander E, Elffors L, Ranstam J, Dequeker J, Dilsen G, Gennari C, Vaz A, Lyritis G, Mazzuoli G, Miravet L, Passeri M, Perez CR, Rapado A, Ribot C (1999) Risk factors for hip fracture in men from southern Europe: the MEDOS study. Mediterranean Osteoporosis Study. Osteoporos Int 9:45–54
Hofman A, Grobbee DE, de Jong PT, van den Ouweland FA (1991) Determinants of disease and disability in the elderly: The Rotterdam Elderly Study. Eur J Epidemiol 7:403–422
De Laet CEDH, Van Hout BA, Burger H, Hofman A, Weel AEAM, Pols HAP (1998) Hip fracture prediction in elderly men and women: validation of the Rotterdam Study. J Bone Miner Res 13:1587–1593
O’Neill TW, Felsenberg D, Varlow J, Cooper C, Kanis JA, Silman AJ (1996) The prevalence of vertebral deformity in European men and women: the European Vertebral Osteoporosis Study. J Bone Miner Res 11:1010–1017
Felsenberg D, Silman AJ, Lunt M, Ambrecht G, Ismail AA, Finn JD, Cockerill WC, Banzer D, Benevolenskaya LI, Bhalla A, Bruges Armas J, Cannata JB, Cooper C, Dequeker J, Eastell R, Ershova O, Felsch B, Gowin W, Havelka S, Hoszowski K, Jajic I, Janot J, Johnell O, Kanis JA, Kragl G, Lopez Vaz A, Lorenc R, Lyritis G, Masaryk P, Matthis C, Miazgowski T, Parisi G, Pols HAP, Poor G, Raspe HH, Reid DM, Reisinger W, Scheidt-Nave C, Stepan J, Todd C, Weber K, Woolf AD, Reeve J, O’Neill TW (2002) Incidence of vertebral fracture in Europe: results from the European Prospective Osteoporosis Study, Epos. J Bone Miner Res 17:716–724
Ismail AA, Pye SR, Cockerill WC, Lunt M, Silman AJ, Reeve J, Banzer D, Benevolenskaya LI, Bhalla A, Bruges Armas J, Cannata JB, Cooper C, Delmas PD, Dequeker J, Dilsen G, Falch JA, Felsch B, Felsenberg D, Finn JD, Gennari C, Hoszowski K, Jajic I, Janott J, Johnell O, Kanis JA, Kragl G, Lopez Vaz A, Lorenc R, Lyritis G, Marchand F, Masaryk P, Matthis C, Miazgowski T, Naves-Diaz M, Pols HAP, Poor G, Rapado A, Raspe HH, Reid DM, Reisinger W, Scheidt-Nave C, Stepan J, Todd C, Weber K, Woolf AD, O’Neill TW (2002) Incidence of limb fracture across Europe: results from the European prospective osteoporosis study, EPOS. Osteoporos Int 13:565–571
Kreiger N, Tenenhouse A, Joseph L et al (1999) The Canadian Multicentre Osteoporosis Study CaMos: background, rationale, methods. Can J Aging 18:376–387
Melton LJ III, Crowson CS, O’Fallon WM, Wahner HW, Riggs BL (2003) Relative contributions of bone density, bone turnover and clinical risk factors to long-term fracture prediction. J Bone Miner Res 18:312–318
Melton LJ III, Atkinson EJ, O’Connor MK, O’Fallon WM, Riggs BL (1998) Bone density and fracture risk in men. J Bone Miner Res 13:1915–1923
Johansson H, Oden A, Johnell O, Jonsson B, De Laet C, Oglesby A, McCloskey EV, Kayan K, Jalava T, Kanis JA (2004) Optimization of BMD measurements to identify high risk groups for treatment—a test analysis. J Bone Miner Res 19(6):906-913
Jones G, Nguyen TV, Sambrook PN, Kelly PJ, Gilbert C, Eisman JA (1994) Symptomatic fracture incidence in elderly men and women. The Dubbo Osteoporosis Epidemiology Study, DOES. Osteoporos Int 4:277–282
Dargant-Molina P, Favier F, Grandjean H et al (1996) Fall-related factors and risk of hip fracture: the EPIDOS prospective study. Lancet 348:145–149
Chapurlat R, Garnero P, Breart G, Meunier P, Delmas PD (2000) Serum estradiol and sex hormone-binding globulin and the risk of hip fracture in elderly women: The EPIDOS study. J Bone Miner Res 15:1835–1841
Garnero P, Sornay-Rendu E, Claustrat B, Delmas PD (2000) Biochemical markers of bone turnover, endogenous hormones and the risk of fracture in postmenopausal women: the OFELY study. J Bone Miner Res 15:1526–1536
Honkanen R, Tuppurainen M, Kroger H, Alhava E, Saarikoski S (1998) Relationships between risk factors and fractures differ by type of fracture; a population-based study of 12,192 perimenopausal women. Osteoporos Int 8:25–31
Svanborg A (1977) Seventy-year-old people in Gothenburg. A population study in an industrialised Swedish city ii. Journal Presentation of Social and Medical Conditions. Acta Medica Scand 611 [Suppl]:5
Johansson C, Black D, Johnell O, Oden A, Mellstrom D (1998) Bone mineral density is a predictor of survival. Calcif Tissue Int 63:190–196
Fujiwara S, Kasagi F, Yamada M, Kodama K (1997) Risk factors for hip fracture in Japanese cohort. J Bone Miner Res 12:998–1004
Fujiwara S, Kagasi F, Masunari N, Naito K, Suzuki G, Fukunage M (2003) Fracture prediction from bone mineral density in Japanese men and women. J Bone Miner Res 18:1547–1553
Kanis JA, Oden A, Johnell O, Jonsson B, De Laet C, Dawson A (2002) The burden of osteoporotic fractures: a method for setting intervention thresholds. Osteoporos Int 12:417–424
Higgins JPT, Thompson SG, Deeks JJ, Altman DG. (2003) Measuring inconsistency in meta-analyses. BMJ 327:557–60
Kiel DP, Felson DT, Anderson JJ, Wilson PWF (1987) Hip fracture and the use of estrogens in postmenopausal women. The Framingham Study. N Eng J Med 317:1169–1174
Malmivaara A, Heliovaara M, Knekt P, Reunanen A, Aromaa A (1993) Risk factors for injurious falls leading to hospitalization or death in a cohort of 19,500 adults. Am J Epidemiol 138:384–394
Bischoff HA, Stahelim HB, Dick W, Akos R, Kuecht M, Salis C, Nebiker M, Thieler R, Pfeifer M, Bergerow B, Lew RA, Conzelmann M (2003) Effects of vitamin D and calcium supplementation on falls: a randomized controlled trial. J Bone Miner Res 18:343–351
Wootton R, Brereton PJ, Clark MB, Hesp R, Hodkinson HM, Klenerman L, Reeve J, Slavin G, Tellez M (1979) Fractured neck of femur in the elderly: an attempt to identify patients at risk. Clin Sci 57:93–101
Nilsson BE (1970) Spinal osteoporosis and femoral neck fracture. Clin Orthop Relat Res 68:93–95
Marshall D, Johnell O, Wedel H (1996) Meta-analysis of how well measures of bone mineral density predict occurrence of osteoporotic fractures. BMJ 312:1254–1259
Sirola J, Kroger H, Honkanen R, Sandini L, Tuppurainen M, Jurvelin JS, Saarikoski S (2003) Risk factors associated with peri- and postmenopausal bone loss: does HRT prevent weight loss-related bone loss? Osteoporos Int 14:27–33
Davison KS, Siminoski K, Chik C, Jen H, Warshawski R, Lee K (2003) Impact of height loss due to vertebral fractures on body mass index. J Bone Miner Res [Suppl]:S243
Acknowledgements
We are grateful to Drs. T.V. Nguyen and J.R. Center for their help with the DOES Study. We would like to thank the Alliance for Better Bone Health, Hologic, IGEA, Lilly, Lunar, Novartis, Pfizer, Roche and Wyeth for their unrestricted support of this work. We are also grateful to the EU (FP3/5), the International Osteoporosis Foundation, the International Society for Clinical Densitometry and the National Osteoporosis Foundation for supporting this study
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
De Laet, C., Kanis, J.A., Odén, A. et al. Body mass index as a predictor of fracture risk: A meta-analysis. Osteoporos Int 16, 1330–1338 (2005). https://doi.org/10.1007/s00198-005-1863-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-005-1863-y