Abstract
Introduction and hypothesis
Sacropexy is considered the gold standard for the treatment of pelvic organ prolapse (POP) although dissection of the promontory may be challenging, particularly in obese women. Laparoscopic lateral suspension with mesh (LLS) could be an alternative.
Methods
LLS provides lateral attachment by fibrosis of a vesicovaginal mesh. Clinical evaluation was performed at 1 year using the simplified POP quantification system (POP-Q). Primary outcomes were objective and subjective cure at 1 year. After a mean of 7.2 years the rates of reoperation and complications were assessed as secondary outcomes. Patient satisfaction was evaluated by telephone interview using a ten-point-scale and the PGI-I scale. Factors predicting satisfaction were determined by logistic regression analysis.
Results
A total of 417 patients were treated between 2003 and 2011. At 1 year 78.4% of patients were asymptomatic and anatomic success rates were 91.6% for the anterior compartment, 93.6% for the apical compartment and 85.3% for the posterior compartment. The complication rate of Clavien-Dindo grade III or higher was 2.2%. The mesh exposure rate was 4.3% and the reoperation rate was 7.3%. Of the 417 patients, 214 participated in the telephone interview. Over 85% rated their situation as improved and satisfaction was associated with the absence of concomitant hysterectomy.
Conclusions
LLS is a safe technique with promising results in terms of a composite outcome, low complication rates and high long-term patient satisfaction. However, a randomized controlled trial is needed to establish the technique as an alternative to sacropexy in the treatment of POP in obese and high morbidity patients.

Similar content being viewed by others
References
Barber MD, Maher C. Epidemiology and outcome assessment of pelvic organ prolapse. Int Urogynecol J. 2013;24(11):1783–1790.
Nygaard I, Barber MD, Burgio KL, Kenton K, Meikle S, Schaffer J, et al. Prevalence of symptomatic pelvic floor disorders in US women. JAMA. 2008;300(11):1311–1316.
Handa VL, Garrett E, Hendrix S, Gold E, Robbins J. Progression and remission of pelvic organ prolapse: a longitudinal study of menopausal women. Am J Obstet Gynecol. 2004;190(1):27–32.
Morrill M, Lukacz ES, Lawrence JM, Nager CW, Contreras R, Luber KM. Seeking healthcare for pelvic floor disorders: a population-based study. Am J Obstet Gynecol. 2007;197(1):86.e1–86.e6.
Smith FJ, Holman CD, Moorin RE, Tsokos N. Lifetime risk of undergoing surgery for pelvic organ prolapse. Obstet Gynecol. 2010;116(5):1096–1100.
Barber MD, Maher C. Apical prolapse. Int Urogynecol J. 2013;24(11):1815–1833.
Vieillefosse S, Thubert T, Dache A, Hermieu JF, Deffieux X. Satisfaction, quality of life and lumbar pain following laparoscopic sacrocolpopexy: suture vs. tackers. Eur J Obstet Gynecol Reprod Biol. 2015;187:51–56.
Dubuisson JB, Yaron M, Wenger JM, Jacob S. Treatment of genital prolapse by laparoscopic lateral suspension using mesh: a series of 73 patients. J Minim Invasive Gynecol. 2008;15(1):49–55.
Toozs-Hobson P, Freeman R, Barber M, Maher C, Haylen B, Athanasiou S, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for reporting outcomes of surgical procedures for pelvic organ prolapse. Int Urogynecol J. 2012;23(5):527–535.
Swift S, Morris S, McKinnie V, Freeman R, Petri E, Scotti RJ, et al. Validation of a simplified technique for using the POPQ pelvic organ prolapse classification system. Int Urogynecol J Pelvic Floor Dysfunct. 2006;17(6):615–620.
Barber MD, Brubaker L, Nygaard I, Wheeler 2nd TL, Schaffer J, Chen Z, et al. Defining success after surgery for pelvic organ prolapse. Obstet Gynecol. 2009;114(3):600–609.
Srikrishna S, Robinson D, Cardozo L. Validation of the patient global Impression of improvement (PGI-I) for urogenital prolapse. Int Urogynecol J. 2010;21(5):523–528.
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250(2):187–196.
Haylen BT, Freeman RM, Swift SE, Cosson M, Davila GW, Deprest J, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint terminology and classification of the complications related directly to the insertion of prostheses (meshes, implants, tapes) and grafts in female pelvic floor surgery. Neurourol Urodyn. 2011;30(1):2–12.
Rozet F, Mandron E, Arroyo C, Andrews H, Cathelineau X, Mombet A, et al. Laparoscopic sacral colpopexy approach for genito-urinary prolapse: experience with 363 cases. Eur Urol. 2005;47(2):230–236.
Paraiso MF, Walters MD, Rackley RR, Melek S, Hugney C. Laparoscopic and abdominal sacral colpopexies: a comparative cohort study. Am J Obstet Gynecol. 2005;192(5):1752–1758.
Rivoire C, Botchorishvili R, Canis M, Jardon K, Rabischong B, Wattiez A, et al. Complete laparoscopic treatment of genital prolapse with meshes including vaginal promontofixation and anterior repair: a series of 138 patients. J Minim Invasive Gynecol. 2007;14(6):712–718.
Claerhout F, De Ridder D, Roovers JP, Rommens H, Spelzini F, Vandenbroucke V, et al. Medium-term anatomic and functional results of laparoscopic sacrocolpopexy beyond the learning curve. Eur Urol. 2009;55(6):1459–1467.
Krause HG, Goh JT, Sloane K, Higgs P, Carey MP. Laparoscopic sacral suture hysteropexy for uterine prolapse. Int Urogynecol J Pelvic Floor Dysfunct. 2006;17(4):378–381.
Gutman R, Maher C. Uterine-preserving POP surgery. Int Urogynecol J. 2013;24(11):1803–1813.
Propst K, Tunitsky-Bitton E, Schimpf MO, Ridgeway B. Pyogenic spondylodiscitis associated with sacral colpopexy and rectopexy: report of two cases and evaluation of the literature. Int Urogynecol J. 2014;25(1):21–31.
Maher C, Feiner B, Baessler K, Schmid C. Surgical management of pelvic organ prolapse in women. Cochrane Database Syst Rev. 2013;4:CD004014.
Birch C, Fynes MM. The role of synthetic and biological prostheses in reconstructive pelvic floor surgery. Curr Opin Obstet Gynecol. 2002;14(5):527–535.
Davila GW, Drutz H, Deprest J. Clinical implications of the biology of grafts: conclusions of the 2005 IUGA grafts roundtable. Int Urogynecol J Pelvic Floor Dysfunct. 2006;17(Suppl 1):S51–S55.
Le TH, Kon L, Bhatia NN, Ostergard DR. Update on the utilization of grafts in pelvic reconstruction surgeries. Curr Opin Obstet Gynecol. 2007;19(5):480–489.
Kockerling F, Schug-Pass C. What do we know about titanized polypropylene meshes? An evidence-based review of the literature. Hernia. 2014;18(4):445–457.
Nygaard IE, McCreery R, Brubaker L, Connolly A, Cundiff G, Weber AM, et al. Abdominal sacrocolpopexy: a comprehensive review. Obstet Gynecol. 2004;104(4):805–823.
Maher CF, Feiner B, DeCuyper EM, Nichlos CJ, Hickey KV, O’Rourke P. Laparoscopic sacral colpopexy versus total vaginal mesh for vaginal vault prolapse: a randomized trial. Am J Obstet Gynecol. 2011;204(4):360.e1–360.e7.
Veit-Rubin N, Dubuisson JB, Lange S, Eperon I, Dubuisson J. Uterus-preserving laparoscopic lateral suspension with mesh for pelvic organ prolapse: a patient-centred outcome report and video of a continuous series of 245 patients. Int Urogynecol J. 2016;27(3):491–493.
Acknowledgements
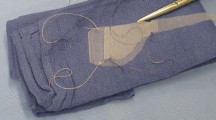
We thank Marc Arcens for the creation of the illustrations.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Jean-Bernard Dubuisson is a medical advisor for pfm medical ag, Köln, Germany.
All other authors declare that they have no conflicts of interest.
Funding
Pfm medical ag, Köln, Germany, contributed to the costs by funding the statistical analysis.
Additional information
Some results of the present study were presented as an e-poster and as a video presentation at the 40th Annual IUGA Meeting in Nice in June 2015, and have been published as an “IUJ video” in this journal (Int Urogynecol J 27(3):491–493, 2016).
Rights and permissions
About this article
Cite this article
Veit-Rubin, N., Dubuisson, JB., Gayet-Ageron, A. et al. Patient satisfaction after laparoscopic lateral suspension with mesh for pelvic organ prolapse: outcome report of a continuous series of 417 patients. Int Urogynecol J 28, 1685–1693 (2017). https://doi.org/10.1007/s00192-017-3327-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-017-3327-2