Abstract
Introduction and hypothesis
We present a technique for quantifying inter-individual variability in normal vaginal shape, axis, and dimension, and report findings in healthy women.
Methods
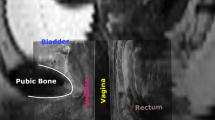
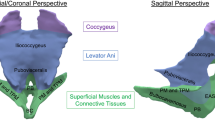
Eighty women (age: 28∼70 years) with normal pelvic organ support underwent supine, multi-planar proton-density MRI. Vaginal width was assessed at five evenly-spaced locations, and vaginal axis, length, and surface area were quantified via ImageJ and MATLAB.
Results
The mid-sagittal plane angles, relative to the horizontal, of three vaginal axes were 90 ± 11, 72 ± 21, and 41 ± 22° (caudal to cranial, p < 0.001). The mean (± SD) vaginal widths were 17 ± 5, 24 ± 4, 30 ± 7, 41 ± 9, and 45 ± 12 mm at the five locations (caudal to cranial, p < 0.001). Mid-sagittal lengths for anterior and posterior vaginal walls were 63 ± 9 and 98 ± 18 mm respectively. The vaginal surface area was 72 ± 21 cm2 (range: 34 ∼ 164 cm2). The coefficient of determination between any demographic variable and any vaginal dimension did not exceed 0.16.
Conclusions
Large variations in normal vaginal shape, axis, and dimensions were not explained by body size or other demographic variables. This variation has implications for reconstructive surgery, intravaginal and surgical product design, and vaginal drug delivery.





Similar content being viewed by others
References
Barnhart K, Izquierdo A, Pretorius ES, Shera DM, Shabbout M, Shaunik A (2006) Baseline dimensions of the human vagina. Hum Reprod 21(6):1618–1622
Nardos R, Thurmond AS, Worstell TR, Clark AL, Gregory WT (2010) Reference lines in dynamic magnetic resonance imaging of the pelvic floor. Female Pelvic Med Reconstr Surg 16(4):242–245
Trowbridge ER, Fultz NH, Patel DA, DeLancey JO, Fenner DE (2008) Distribution of pelvic organ support measures in a population-based sample of middle-aged, community-dwelling African American and white women in southeastern Michigan. Am J Obstet Gynecol 198(5):548.e1–548.e6
Luo J, Larson KA, Fenner DE, Ashton-Miller JA, Delancey JO (2012) Posterior vaginal prolapse shape and position changes at maximal Valsalva seen in 3-D MRI-based models. Int Urogynecol J 23(9):1301–1306
Betschart C, Chen L, Ashton-Miller JA, Delancey JO (2013) On pelvic reference lines and the MR evaluation of genital prolapse: a proposal for standardization using the pelvic inclination correction system. Int Urogynecol J 24(9):1421–1428
DeLancey JO (1992) Anatomic aspects of vaginal eversion after hysterectomy. Am J Obstet Gynecol 166(6 Pt 1):1717–1724, discussion 1724–1718
Sze EH, Meranus J, Kohli N, Miklos JR, Karram MM (2001) Vaginal configuration on MRI after abdominal sacrocolpopexy and sacrospinous ligament suspension. Int Urogynecol J Pelvic Floor Dysfunct 12(6):375–379, discussion 379–380
Guaderrama NM, Nager CW, Liu J, Pretorius DH, Mittal RK (2005) The vaginal pressure profile. Neurourol Urodyn 24(3):243–247
Jung S, Pretorius DH, Padda BS, Weinstein MM, Nager CW, den Boer DJ, Mittal RK (2007) Vaginal high-pressure zone assessed by dynamic 3-dimensional ultrasound images of the pelvic floor. Am J Obstet Gynecol 197(1):52.e1–52.e7
Blaisdell FE (1917) The anatomy of the sacro-uterine ligaments. Anat Rec 12(1):1–42
Campbell RM (1950) The anatomy and histology of the sacrouterine ligaments. Am J Obstet Gynecol 59(1):1–12
Buller JL, Thompson JR, Cundiff GW, Krueger Sullivan L, Schon Ybarra MA, Bent AE (2001) Uterosacral ligament: description of anatomic relationships to optimize surgical safety. Obstet Gynecol 97(6):873–879
Paramore RH (1918) The uterus as a floating organ. The statics of the female pelvic viscera. Lewis, London, p 12
Dutta DC, Konar H (2014) DC Dutta’s textbook of gynecology. Jaypee Brothers, Medical Publishers, New Delhi
Standring S, Gray H (2008) Gray’s anatomy: the anatomical basis of clinical practice, 40th edn. Churchill Livingstone/Elsevier, Edinburgh
Tan JS, Lukacz ES, Menefee SA, Luber KM, Albo ME, Nager CW (2006) Determinants of vaginal length. Am J Obstet Gynecol 195(6):1846–1850
Nichols DH, Milley PS, Randall CL (1970) Significance of restoration of normal vaginal depth and axis. Obstet Gynecol 36(2):251–256
Funt MI, Thompson JD, Birch H (1978) Normal vaginal axis. South Med J 71(12):1534–1535
Pendergrass PB, Belovicz MW, Reeves CA (2003) Surface area of the human vagina as measured from vinyl polysiloxane casts. Gynecol Obstet Investig 55(2):110–113
Acknowledgements
We gratefully acknowledge support from the National Institute of Child Health and Human Development Grants R01 HD 038665, the Office for Research on Women’s Health SCOR on Sex and Gender Factors Affecting Women’s Health P50 HD 044406, the National Center for Advancing Translational Sciences 2UL1TR000433, and a Grant from the Swiss National Science Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Dr. Jiajia Luo does not have any conflicts of interest directly related to this study, but his doctoral studies were partially funded by American Medical Systems and Kimberly-Clark Corporation, and he has also received research support from Boston Scientific Corporation. Dr. John O.L. DeLancey and Dr. James A. Ashton-Miller do not have any conflicts of interest directly related to this study. The University of Michigan received research funding for partial salary support from Johnson & Johnson, American Medical Systems, Kimberly-Clark Corporation, Procter & Gamble, and Boston Scientific Corporation. They received an honorarium and travel reimbursement for giving an invited research seminar at Johnson & Johnson. Dr. Cornelia Betschart received research support from the Swiss National Science Foundation unrelated to the topic of this paper.
Electronic supplementary material
Below is the link to the electronic supplementary material.
The vaginal surface of each patient is presented as anterior (red) and posterior (blue) vaginal wall (Luo©). Size: 5.67 MB. Length: 40 s. (WMV 5666 kb)
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Luo, J., Betschart, C., Ashton-Miller, J.A. et al. Quantitative analyses of variability in normal vaginal shape and dimension on MR images. Int Urogynecol J 27, 1087–1095 (2016). https://doi.org/10.1007/s00192-016-2949-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-016-2949-0