Abstract
Introduction and hypothesis
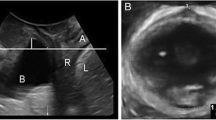
The goal of this study was to use a well-described system of quantifying levator ani defect (LAD) severity using magnetic resonance imaging (MRI) to examine the relationship between defect severity and the presence or absence of prolapse.
Methods
This is a secondary analysis of two case–control studies comparing 284 cases (with prolapse) to 219 controls (normal support) defined by using Pelvic Organ Prolapse Quantification (POP-Q) exams. LAD were assessed on MRI, with scores from 0 (no defects) to 6 (complete, bilateral defects). The number of cases and controls at each score were compared. Logistic regression and receiver operating characteristic (ROC) analyses were used to quantify relationships between LAD and prolapse.
Results
The proportion of cases exceeds the overall prolapse rate in this study at LAD scores ≥3, with higher rates of prolapse at higher LAD scores (p < 0.0000001). Prolapse risk stratifies into low risk at LAD scores 0–2, moderate at 3–5, and high at 6. ROC analysis for classification of prolapse based on LAD scores has an area under the curve of 69.9 % (p < 0.001), suggesting LAD alone can discriminate between normal support and prolapse for nearly 70 % of patients. Logistic regression identified higher parity and higher LAD scores as independent predictors of prolapse.
Conclusions
There are three clusters of prolapse risk: low (0–2), moderate (3–5), and high (6). Although LAD have a dose-response-like effect for prolapse, other factors are clearly involved.


Similar content being viewed by others
Abbreviations
- PFD:
-
Pelvic floor disorders
- POP:
-
Pelvic organ prolapse
- LAD:
-
Levator ani defects
- MRI:
-
Magnetic resonance imaging
- ROC:
-
Receiver operating characteristic
- HRT:
-
Hormone replacement therapy
References
Nygaard I, Barber MD, Burgio KL, Kenton K, Meikle S, Schaffer J, Spino C, Whitehead WE, Wu J, Brody DJ (2008) Prevalence of symptomatic pelvic floor disorders in US women. JAMA 300:1311–1316
Sung VW, Hampton BS (2009) Epidemiology of pelvic floor dysfunction. Obstet Gynecol Clin N Am 36:421–443
Wu JM, Hundley AF, Fulton RG, Myers ER (2009) Forecasting the prevalence of pelvic floor disorders in U.S. Women: 2010 to 2050. Obstet Gynecol 114:1278–1283
Lammers K, Futterer JJ, Prokop M, Vierhout ME, Kluivers KB (2012) Diagnosing pubovisceral avulsions: a systematic review of the clinical relevance of a prevalent anatomical defect. Int Urogynecol J 23:1653–1664
Morgan DM, Umek W, Stein T, Hsu Y, Guire K, DeLancey JO (2007) Interrater reliability of assessing levator ani muscle defects with magnetic resonance images. Int Urogynecol J Pelvic Floor Dysfunct 18:773–778
Dietz HP (2007) Quantification of major morphological abnormalities of the levator ani. Ultrasound Obstet Gynecol 29:329–334
Kearney R, Miller JM, Ashton-Miller JA, DeLancey JO (2006) Obstetric factors associated with levator ani muscle injury after vaginal birth. Obstet Gynecol 107:144–149
DeLancey JO, Morgan DM, Fenner DE, Kearney R, Guire K, Miller JM, Hussain H, Umek W, Hsu Y, Ashton-Miller JA (2007) Comparison of levator ani muscle defects and function in women with and without pelvic organ prolapse. Obstet Gynecol 109:295–302
Bump RC, Mattiasson A, Bo K, Brubaker LP, DeLancey JO, Klarskov P, Shull BL, Smith AR (1996) The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol 175:10–17
Dean AG, Sullivan KM, Soe MM (last updated 2013/04/06) OpenEpi: Open Source Epidemiologic Statistics for Publich Health, www.OpenEpi.com. Accessed 05 November 2013
Dietz HP, Simpson JM (2008) Levator trauma is associated with pelvic organ prolapse. BJOG 115:979–984
Rostaminia G, White D, Hegde A, Quiroz LH, Davila GW, Shobeiri SA (2013) Levator ani deficiency and pelvic organ prolapse severity. Obstet Gynecol 121:1017–1024
Grimes DA, Schulz KF (2005) Refining clinical diagnosis with likelihood ratios. Lancet 365:1500–1505
Kerkhof MH, Hendriks L, Brolmann HA (2009) Changes in connective tissue in patients with pelvic organ prolapse–a review of the current literature. Int Urogynecol J 20:461–474
de Boer TA, Slieker-Ten Hove MC, Burger CW, Kluivers KB, Vierhout ME (2011) The prevalence and factors associated with previous surgery for pelvic organ prolapse and/or urinary incontinence in a cross-sectional study in The Netherlands. Eur J Obstet Gynecol Reprod Biol 158:343–349
Conflict of interest
This research was funded by NICHD grant R01 HD38665 and ORWH grant P50 HD44406. Dr. DeLancey has consulted with Proctor & Gamble during the last year on topics not relevant to this manuscript. No conflicts of interest are declared for Drs. Berger and Morgan.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Berger, M.B., Morgan, D.M. & DeLancey, J.O. Levator ani defect scores and pelvic organ prolapse: is there a threshold effect?. Int Urogynecol J 25, 1375–1379 (2014). https://doi.org/10.1007/s00192-014-2388-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-014-2388-8