Abstract
Aims/hypothesis
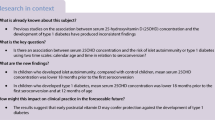
Vitamin D deficiency is common in people with type 1 diabetes, but its role in disease progression is unclear. Our aim was to assess the prevalence of vitamin D deficiency in prediabetes (defined as the presence of multiple islet autoantibodies), and investigate whether or not progression to type 1 diabetes is faster in children with vitamin D deficiency and multiple islet autoantibodies.
Methods
Levels of 25-hydroxyvitamin D [25(OH)D] were measured in 108 children with multiple islet autoantibodies within 2 years of islet autoantibody seroconversion, in 406 children who remained islet autoantibody-negative and in 244 patients with newly diagnosed type 1 diabetes. Children with multiple islet autoantibodies were prospectively followed for a median of 5.8 years (interquartile range 3.4–8.6 years) to monitor progression to type 1 diabetes.
Results
In the cross-sectional analysis, 25(OH)D levels were lower and the prevalence of vitamin D deficiency (<50 nmol/l) was higher in children with prevalent multiple islet autoantibodies than in islet autoantibody-negative children (59.9 ± 3.0 vs 71.9 ± 1.5 nmol/l; p < 0.001; 39.8% vs 28.3%; p = 0.021). The differences in vitamin D levels between the groups were greatest in summer. The cumulative incidence of type 1 diabetes at 10 years after seroconversion was similar between children with vitamin D deficiency and those with sufficient vitamin D levels (51.8% [95% CI 29.3, 74.3] vs 55.4% [95% CI 35.5, 72.3], p = 0.8).
Conclusions/interpretation
Vitamin D levels were lower in children with multiple islet autoantibodies and in children with type 1 diabetes than in autoantibody-negative children. However, vitamin D deficiency was not associated with faster progression to type 1 diabetes in children with multiple islet autoantibodies.




Similar content being viewed by others
Abbreviations
- 25(OH)D:
-
25-Hydroxyvitamin D
- IQR:
-
Interquartile range
References
Eisenbarth GS (1986) Type I diabetes mellitus. A chronic autoimmune disease. N Engl J Med 314:1360–1368
Ziegler AG, Rewers M, Simell O et al (2013) Seroconversion to multiple islet autoantibodies and risk of progression to diabetes in children. JAMA 309:2473–2479
Atkinson MA, Eisenbarth GS (2001) Type 1 diabetes: new perspectives on disease pathogenesis and treatment. Lancet 358:221–229
Luong K, Nguyen LT, Nguyen DN (2005) The role of vitamin D in protecting type 1 diabetes mellitus. Diabetes Metab Res Rev 21:338–346
Chakhtoura M, Azar ST (2013) The role of vitamin D deficiency in the incidence, progression, and complications of type 1 diabetes mellitus. Int J Endocrinol 2013:148673
Baumgartl HJ, Standl E, Schmidt-Gayk H, Kolb HJ, Janka HU, Ziegler AG (1991) Changes of vitamin D3 serum concentrations at the onset of immune-mediated type 1 (insulin-dependent) diabetes mellitus. Diabetes Res 16:145–148
Pozzilli P, Manfrini S, Crino A et al (2005) Low levels of 25-hydroxyvitamin D3 and 1,25-dihydroxyvitamin D3 in patients with newly diagnosed type 1 diabetes. Horm Metab Res 37:680–683
Littorin B, Blom P, Scholin A et al (2006) Lower levels of plasma 25-hydroxyvitamin D among young adults at diagnosis of autoimmune type 1 diabetes compared with control subjects: results from the nationwide Diabetes Incidence Study in Sweden (DISS). Diabetologia 49:2847–2852
Bierschenk L, Alexander J, Wasserfall C, Haller M, Schatz D, Atkinson M (2009) Vitamin D levels in subjects with and without type 1 diabetes residing in a solar rich environment. Diabetes Care 32:1977–1979
Ziegler AG, Baumgartl HJ, Ede G et al (1990) Low-pigment skin type and predisposition for development of type I diabetes. Diabetes Care 13:529–531
Baeke F, Takiishi T, Korf H, Gysemans C, Mathieu C (2010) Vitamin D: modulator of the immune system. Curr Opin Pharmacol 10:482–496
Badenhoop K, Kahles H, Penna-Martinez M (2012) Vitamin D, immune tolerance, and prevention of type 1 diabetes. Curr Diab Rep 12:635–642
Fassbender WJ, Goertz B, Weismuller K et al (2002) VDR gene polymorphisms are overrepresented in German patients with type 1 diabetes compared to healthy controls without effect on biochemical parameters of bone metabolism. Horm Metab Res 34:330–337
Frederiksen B, Liu E, Romanos J et al (2013) Investigation of the vitamin D receptor gene (VDR) and its interaction with protein tyrosine phosphatase, non-receptor type 2 gene (PTPN2) on risk of islet autoimmunity and type 1 diabetes: the Diabetes Autoimmunity Study in the Young (DAISY). J Steroid Biochem Mol Biol 133:51–57
Gorham ED, Garland CF, Burgi AA et al (2012) Lower prediagnostic serum 25-hydroxyvitamin D concentration is associated with higher risk of insulin-requiring diabetes: a nested case-control study. Diabetologia 55:3224–3227
Munger KL, Levin LI, Massa J, Horst R, Orban T, Ascherio A (2013) Preclinical serum 25-hydroxyvitamin D levels and risk of type 1 diabetes in a cohort of US military personnel. Am J Epidemiol 177:411–419
Hyppönen E, Läärä E, Reunanen A, Järvelin M-R, Virtanen SM (2001) Intake of vitamin D and risk of type 1 diabetes: a birth-cohort study. Lancet 358:1500–1503
Simpson M, Brady H, Yin X et al (2011) No association of vitamin D intake or 25-hydroxyvitamin D levels in childhood with risk of islet autoimmunity and type 1 diabetes: the Diabetes Autoimmunity Study in the Young (DAISY). Diabetologia 54:2779–2788
Skyler JS (2013) Primary and secondary prevention of type 1 diabetes. Diabet Med 30:161–169
Ziegler AG, Hummel M, Schenker M, Bonifacio E (1999) Autoantibody appearance and risk for development of childhood diabetes in offspring of parents with type 1 diabetes: the 2-year analysis of the German BABYDIAB Study. Diabetes 48:460–468
Ziegler AG, Meier-Stiegen F, Winkler C, Bonifacio E (2012) Prospective evaluation of risk factors for the development of islet autoimmunity and type 1 diabetes during puberty—TEENDIAB: study design. Pediatr Diabetes 13:438–443
Hummel S, Pflüger M, Hummel M, Bonifacio E, Ziegler AG (2011) Primary dietary intervention study to reduce the risk of islet autoimmunity in children at increased risk for type 1 diabetes: the BABYDIET study. Diabetes Care 34:1301–1305
Thümer L, Adler K, Bonifacio E et al (2010) German new onset diabetes in the young incident cohort study: DiMelli study design and first-year results. Rev Diabet Stud 7:202–208
Puavilai G, Chanprasertyotin S, Sriphrapradaeng A (1999) Diagnostic criteria for diabetes mellitus and other categories of glucose intolerance: 1997 criteria by the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus (ADA), 1998 WHO consultation criteria, and 1985 WHO criteria. World Health Organization. Diabetes Res Clin Pract 44:21–26
Achenbach P, Lampasona V, Landherr U et al (2009) Autoantibodies to zinc transporter 8 and SLC30A8 genotype stratify type 1 diabetes risk. Diabetologia 52:1881–1888
Törn C, Mueller PW, Schlosser M, Bonifacio E, Bingley PJ (2008) Diabetes Antibody Standardization Program: evaluation of assays for autoantibodies to glutamic acid decarboxylase and islet antigen-2. Diabetologia 51:846–852
Schlosser M, Mueller PW, Torn C, Bonifacio E, Bingley PJ (2010) Diabetes Antibody Standardization Program: evaluation of assays for insulin autoantibodies. Diabetologia 53:2611–2620
Lampasona V, Schlosser M, Mueller PW et al (2011) Diabetes antibody standardization program: first proficiency evaluation of assays for autoantibodies to zinc transporter 8. Clin Chem 57:1693–1702
Kumar J, Muntner P, Kaskel FJ, Hailpern SM, Melamed ML (2009) Prevalence and associations of 25-hydroxyvitamin D deficiency in US children: NHANES 2001-2004. Pediatrics 124:e362–e370
Frederiksen BN, Kroehl M, Fingerlin TE et al (2013) Association between vitamin D metabolism gene polymorphisms and risk of islet autoimmunity and progression to type 1 diabetes: the Diabetes Autoimmunity Study in the Young (DAISY). J Clin Endocrinol Metab 98:E1845–1851S
Acknowledgements
We thank C. Ried, A. Wosch, L. Lachmann, F. Haupt, M. Scholz, A. Gavrisan, A. Knopff, S. Krause, C. Matzke, V. Dietrich and J. Stock for data collection and expert technical assistance, R. Chmiel and A. Huppert for clinical care of the children, R. Puff for laboratory management and A. Beyerlein for statistical assistance (all from Institute of Diabetes Research, Helmholtz Zentrum München, and Forschergruppe Diabetes, Klinikum rechts der Isar, Technische Universität München, Neuherberg, Germany). We also thank all of the children, paediatricians and family doctors for participating in the BABYDIAB, BABYDIET and TEENDIAB studies and all of the clinics who enrolled children into DiMelli.
Funding
The work was supported by grants from the Kompetenznetz Diabetes mellitus (Competence Network for Diabetes mellitus), funded by the Federal Ministry of Education and Research (FKZ 01GI0805-07, FKZ 01GI0805), from Deutsche Forschungsgemeinschaft (DFG ZI-310/14-1 to -4) and the Juvenile Diabetes Research Fund (JDRF-No 17-2012-16).
Duality of interest
The authors declare that there is no duality of interest associated with this manuscript.
Contribution statement
JR and CW collected and reviewed the data, performed statistical analyses, interpreted the results and drafted the manuscript. SS assisted with follow-up assessments and data collection, and critically reviewed the manuscript for intellectual content. KW, EZG and MK contributed to statistical analyses, interpreted the results, and critically reviewed the manuscript for intellectual content. A-GZ is the principal investigator of the BABYDIAB, BABYDIET, TEENDIAB and DiMelli studies, designed the studies, wrote the manuscript and critically reviewed it for intellectual content. A-GZ had primary responsibility for the final content of the manuscript. All authors read and approved the final version.
Author information
Authors and Affiliations
Corresponding author
Additional information
Christiane Winkler and Anette-Gabriele Ziegler are joint last authors of this article
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM Table 1
(PDF 20 kb)
Rights and permissions
About this article
Cite this article
Raab, J., Giannopoulou, E.Z., Schneider, S. et al. Prevalence of vitamin D deficiency in pre-type 1 diabetes and its association with disease progression. Diabetologia 57, 902–908 (2014). https://doi.org/10.1007/s00125-014-3181-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-014-3181-4