Abstract
Aims/hypothesis
The aim of this study was to investigate whether air pollution from traffic at a residence is associated with mortality related to type 1 or type 2 diabetes.
Methods
We followed up 52,061 participants in the Danish Diet, Cancer and Health cohort for diabetes-related mortality in the nationwide Register of Causes of Death, from baseline in 1993–1997 up to the end of 2009, and traced their residential addresses since 1971 in the Central Population Registry. We used dispersion-modelled concentration of nitrogen dioxide (NO2) since 1971 and amount of traffic at the baseline residence as indicators of traffic-related air pollution and used Cox regression models to estimate mortality-rate ratios (MRRs) with adjustment for potential confounders.
Results
Mean levels of NO2 at the residence since 1971 were significantly associated with mortality from diabetes. Exposure above 19.4 μg/m3 (upper quartile) was associated with a MRR of 2.15 (95% CI 1.21, 3.83) when compared with below 13.6 μg/m3 (lower quartile), corresponding to an MRR of 1.31 (95% CI 0.98, 1.76) per 10 μg/m3 NO2 after adjustment for potential confounders.
Conclusions/interpretation
This study suggests that traffic-related air pollution is associated with mortality from diabetes. If confirmed, reduction in population exposure to traffic-related air pollution could be an additional strategy against the global public health burden of diabetes.
Similar content being viewed by others
Introduction
Type 1 diabetes is an autoimmune disorder with defective insulin production usually presenting in younger ages and accounting for less than 10% of diabetes cases [1]. Genetics play a major role but environmental, lifestyle and dietary exposures, such as air pollution [2], might interact with genetic susceptibility in development of the disease [3]. Type 2 diabetes is a metabolic disorder caused by inadequate secretion of insulin in response to overnutrition, physical inactivity and insulin resistance and accounts for more than 90% of diabetes cases [4]. The disease is one of the most prevalent chronic diseases worldwide and is projected to increase dramatically over the next decades due to ageing populations and rising levels of obesity and physical inactivity [5]. In addition to age, obesity, diet and inactivity, active smoking has been convincingly associated with type 2 diabetes [6] and two recent studies also link environmental tobacco smoke to risk for type 2 diabetes [7, 8]. It has been suggested that such environmental and lifestyle factors account for more than 90% of adult-onset diabetes [9]. It is well known that ambient air pollution is associated with cardiovascular diseases, possibly mediated by systemic oxidative stress and inflammation [10]. The same mechanisms seem to be relevant for promotion of insulin resistance and development of type 2 diabetes [10–13] but ambient air pollution has only recently been investigated as a risk factor for type 2 diabetes in epidemiological studies. Cross-sectional studies have linked diabetes prevalence to exposure to fine particles with an aerodynamic diameter ≤2.5 μm (PM2.5) [14] and nitrogen dioxide (NO2) [15] in ambient air but another cross-sectional study found no consistent association [16]. Time-series and case-crossover studies have linked short-term exposure to air pollution with diabetes-related death [17–19] and data from three prospective cohort studies on long-term exposure to ambient air pollution and diabetes collectively indicate an association between traffic-related air pollution and incident type 2 diabetes [20–22]. Diabetes mortality might particularly reflect long-term exposure and was found to be increased among construction workers exposed to diesel particulates [23].
We have previously found an association between air pollution and incidence of confirmed diabetes among participants in an elderly cohort in Denmark [22]. The aim of the present study was to investigate the association between long-term levels of traffic-related air pollution at residential locations and mortality due to diabetes of either type in the same cohort.
Methods
Design and study participants
Between 1993 and 1997, a population-based sample of 57,053 men (48%) and women (52%) aged 50–64 years were recruited into the Diet, Cancer and Health cohort study [24]. Participants lived in the Copenhagen and Aarhus areas, were born in Denmark and had no previous cancer diagnosis. Most participants lived in urban areas with dense population and road network but participants were also recruited from areas up to 25 km outside the city centres. The baseline examination included a self-administered questionnaire on dietary habits, which covered 192 food and beverage items. The participants also filled in a questionnaire on smoking habits, occupation, length of school attendance, physical activity, history of diseases and medication and a number of other health-related items [24]. Staff in the study clinics obtained anthropometrics measurements, including height and weight. Relevant Danish ethical committees and data protection agencies approved the study and written informed consent was obtained from all participants.
Each cohort member was followed up for death from diabetes (International Classification of Diseases (ICD)-10 codes E10–E14; see www.who.int/classifications/icd/en/), including date and up to four causes (underlying and contributing), from the date of inclusion into the cohort until 31 December 2009 in the Danish Register of Causes of Death [25]. We used the unique personal identification number to link data. We extracted the date of emigration or disappearance and the addresses of all cohort members between 1 January 1971 and 31 December 2009 from the Central Population Registry, including the dates of moving to and from each address. The addresses were linked to the Danish address database and geographical coordinates (‘geocodes’) were obtained for 94% of the addresses.
Exposure assessment
The outdoor concentration of NO2 was calculated for each year at the residential addresses of each cohort member with the Danish AirGIS dispersion modelling system (see www.dmu.dk/en/air/models/airgis/, accessed 11 April 2012 and [26]). AirGIS provides estimates of traffic-related air pollution with high temporal and address-level spatial resolution. Air pollution at a location was calculated as the sum of: (1) local air pollution from street traffic, calculated from traffic (intensity and type), emission factors for the car fleet, street and building geometry and meteorology; (2) urban background, calculated from data on urban vehicle emission density, city dimensions and building heights and (3) regional background, estimated from trends at rural monitoring stations and data for national vehicle emissions. Air pollution was calculated for 2 m height at the façade of the address building. The AirGIS system has been described and validated in several studies (see electronic supplementary material [ESM] Methods) [27–29].
We used the concentration of NO2 as an indicator of air pollution from traffic. We calculated yearly averages of NO2 concentration at all addresses from 1 January 1971 until date of death, censoring or end of follow-up and entered the time-weighted average from 1971 as a time-dependent variable into the statistical risk model, thus recalculating exposure for survivors at the time of each death due to diabetes. If an address could not be geocoded, the preceding address was used for NO2 calculation; if the first address was missing, the subsequent address was used. We included only participants for whom the residential addresses were known and geocoded for 80% or more of the time from 1 January 1971 to death, censoring or end of follow-up.
Potential confounders and effect modifiers
We defined potential confounding factors a priori and modelled them as categorical, linear or a spline function. The covariates, assessed at baseline, were: sex; calendar year (spline); length of school attendance (<8, 8–10 and >10 years) used as proxy for health behaviour, use of healthcare system, compliance with medical treatment and income level; risky occupation, defined as job held for a minimum of 1 year with potential exposure to smoke, particles, fumes or chemicals (yes/no) (mining, rubber industry, tannery, chemical industry, wood-processing industry, metal processing [welding, painting, electroplating], foundry, steel-rolling mill, shipyard, glass industry, graphics industry, building industry [roofer, asphalt worker, demolition worker], truck, bus or taxi driver, manufacture of asbestos or asbestos cement, asbestos insulation, cement article industry, china and pottery industry, painter, welder, hairdresser, auto mechanic); smoking status (never, former, current); smoking intensity (lifetime average, linear, calculated by equating a cigarette to 1 g, a cheroot or a pipe to 3 g and a cigar to 4.5 g of tobacco); smoking duration (linear); environmental tobacco smoke (indicator of exposure, e.g. ‘smoker in the home or/and exposure at work for at least 4 h/day’); physically active sport (indicator and linear intensity among active people); BMI (spline); waist circumference (linear); alcohol intake (indicator and spline for intensity among drinkers); fat intake (linear); fruit and vegetable intake (linear); hypertension (self reported) and hypercholesterolaemia (self reported).
The pre-specified potential effect modifiers, assessed at baseline, were: sex, BMI, physical activity, smoking status, educational level and intake of fruit and vegetables.
Statistical methods
Mortality-rate ratios (MRRs) were estimated from Cox proportional hazards models with left truncation, age as the time scale and right censoring at the date of death due to causes other than diabetes, the date of loss to follow-up due to emigration or disappearance or 31 December 2009, whichever came first. The models were fit in Stata 11.0 (www.stata.com).
We investigated interactions with the likelihood ratio test, comparing models with and without an interaction term. Exposure–response functions with 95% CIs were visualised using restricted cubic splines (library Survival and library Design in R statistical software 2.9.0) adjusting for the potential confounders [30].
Sensitivity analyses
To test the sensitivity for defining exposure, we applied five alternative measures: NO2 concentration at addresses since 1991; NO2 at the baseline address; NO2 at addresses the year preceding death and two simple indicators of traffic at the baseline address (first, presence of a street with a traffic density >10,000 vehicles per day within 50 m of the residence and, second, total number of kilometres driven by vehicles within 200 m of the residence each day). We considered the NO2 concentration since 1971 as our primary exposure variable because it takes into account a number of factors that affect traffic-related air pollution and because it reflects exposure over several decades. Further, we repeated our main analyses for the subcohort of participants who lived at the same address during follow-up. We considered a death to be due to diabetes if diabetes was stated as either the underlying or a contributing cause of death, and in a sensitivity analysis only if diabetes was stated as the underlying cause.
Results
Of 160,725 eligible individuals, 57,053 accepted the invitation and were enrolled into the cohort. Of these, 571 were excluded because of a cancer diagnosis before baseline, two because of uncertain date of cancer diagnosis, 960 for whom an address history was not available in the Central Population Registry or their address at baseline could not be geocoded, 948 because exposure was assessed for less than 80% of the time between 1 January 1971 and death or censoring and 2,511 for whom a value was missing for a potential confounder or effect modifier, leaving 52,061 cohort members for the study. These participants were followed up for an average of 13.0 years, during which 122 died from diabetes, providing a crude diabetes mortality rate of 18.0 per 100,000 person-years at risk. Of the 122 cohort members who died from diabetes, 14 were coded in the Mortality Register as ‘insulin-dependent’ (E10), 54 as ‘non-insulin-dependent’ (E11) and 54 as ‘unspecified diabetes mellitus’ (E14). For 32 of the 122 who died from diabetes, diabetes was stated as a contributing cause of death and the underlying cause of death being: cardiovascular or cerebrovascular disease (n = 13), obesity (n = 2), chronic obstructive pulmonary disease (n = 2), alcohol-related disease (n = 4), cancer (n = 7), tuberculous adenitis (n = 1) and ‘unknown’ (n = 3).
Table 1 shows the baseline characteristics of the 52,061 cohort members, with a median age of 56.1 years and slightly more women than men. Cohort members who died due to diabetes during follow-up had shorter school attendance than the whole cohort, were more often men, occupationally exposed to air pollution, smokers and exposed to environmental tobacco smoke, had a higher intake of fat, a lower intake of fruit and vegetables, a higher BMI, a greater waist circumference, were rarely physically active in leisure-time sports, had pre-existing hypertension and hypercholesterolaemia at baseline and were living at higher NO2 levels and close to dense traffic. Furthermore, among those living at locations with high NO2 levels, more were smokers and exposed to environmental tobacco smoke and fewer were physical active. Many characteristics were, however, similar for people living at residences with high and low levels of NO2. The mean NO2 concentration at the residences of all participants after 1971 was 16.9 μg/m3 (minimum, 10.5 μg/m3; median, 15.1 μg/m3; maximum, 59.6 μg/m3). Figures 1 and 2 show right-skewed distributions of NO2 and traffic at the residence.
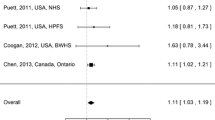
Table 2 shows that NO2 at the residence after 1971 was associated with diabetes mortality, with MRRs of 1.52 (95% CI 0.83, 2.80), 1.65 (95% CI 0.91, 2.98) and 2.15 (95% CI 1.21, 3.83) in association with, respectively, the second, third and fourth exposure quartile, when compared with the lower quartile, after adjustment for potential confounders. In fully adjusted linear models, NO2 after 1971 was associated with an MRR of 1.31 (95% CI 0.98, 1.76), NO2 after 1991 with a MRR of 1.18 (95% CI 0.92, 1.50), NO2 at the baseline address with an MRR of 1.14 (95% CI 0.90, 1.44) and NO2 during the year preceding death with an MRR of 1.30 (95% CI 1.03, 1.63) per 10 μg/m3 NO2 (Table 3). The number of vehicle-km driven within 200 m of the baseline residence was significantly associated with diabetes mortality but the presence of a major road within 50 m of the residence was not (Table 3). Figure 3 a, b shows higher MRR for diabetes in association with higher NO2 since 1971 and traffic at the residence, based on the fully adjusted model. Similar results were obtained in sensitivity analyses among cohort members who lived at the same address during follow-up and when restricting our endpoint to death where diabetes was stated as the underlying cause (ESM Tables 1, 2).
Spline functions (filled lines; 95% CIs indicated by dashed lines) between average NO2 concentration at residences from 1971 onwards (a), traffic load within 200 m of the baseline address (b) and diabetes mortality. The functions were based on fully adjusted models and cohort members with exposure between the 5th and the 95th percentile. The spline function can be interpreted as the dose–response association. The difference on the y-axis for two points on the curve is interpreted as the difference in log MRR for the corresponding difference in exposure, which can be read on the x-axis between the same two points. For example, (a) shows that an increase in exposure from 15 to 20 μg/m3 is associated with an increase in log relative hazard of approximately 0.35, corresponding to a 42% increase in the MRR
Adjustment for potential confounders substantially lowered the MRRs. The impact was caused by adjustment for smoking status, alcohol intake, physical activity and BMI.
Table 4 shows similar diabetes MRRs in association with NO2 for men and women, and for different levels of education, BMI and intake of fruit and vegetables. The table shows higher MRRs for never smokers compared with ever smokers and for participants doing no sport during leisure time compared with those who did. However, none of these differences were statistically significant.
Discussion
We found a statistically significant association between long-term exposure to traffic-related air pollution at the residence and diabetes mortality, which has not been investigated in a prospective cohort previously. The strengths of this study include a 13-year prospective follow-up of a large cohort and adjustment for many potential confounders. Dietary intake was based on a 192-item food frequency questionnaire, which was validated against weighted dietary records [31, 32]. Complete follow-up for mortality and vital status was possible through nationwide population-based registries. Further, exposure was assessed at addresses between 22 and 39 years before death. A limitation of this study is the relatively few deaths due to diabetes resulting in imprecise risk estimates and we cannot exclude the possibility of a chance finding. Moreover, we cannot distinguish clearly between death due to type 1 and type 2 diabetes, although the ICD-10 codes concerning insulin-dependence indicate that the majority of the deaths were due to type 2 diabetes (non-insulin-dependent), as could be expected [4]. The relatively few deaths due to diabetes and the missing specification of insulin dependence for 54 of 122 deaths in the Mortality Register prevent analyses by insulin dependence. The model used to calculate NO2 concentrations at addresses requires comprehensive input data and has been validated [27–29] and applied [22, 33–37]. Although model-based estimates of air pollution concentrations are inevitably somewhat uncertain (e.g. because we estimated air pollution at 2 m height and not for the actual height of the dwelling), any resulting nondifferential misclassification would create artificial associations only in rare situations [38].
It has long been recognised that use of the underlying cause of death from death certificates can underestimate mortality from diabetes [39]. Coding of cause of death is problematic when a decedent has multiple chronic conditions because a single disease may not adequately describe the cause of death [40]. Diabetes is linked to increased incidence of renal disease [41], cardiovascular disease [42, 43] and cancer [44]. For people with diabetes dying with such other diseases, diabetes is unlikely to be registered as the underlying cause of death; instead diabetes might be listed on the death certificate as a contributory cause of death [41]. Problems in defining the underlying cause of death can partly be overcome in epidemiological studies by counting deaths with diabetes stated as being either the underlying or contributing cause of death as death due to diabetes [39]. Such use of underlying and any cause of death provided virtually identical results in the present study and any misclassification of cause of death is unlikely to be associated with air pollution levels and would change the MRRs towards 1.00 rather than create artificial associations.
We found no systematic differences in MRRs for the different time windows of NO2 exposure, with the highest (and similar) MRRs for exposure since 1971 and exposure during the year preceding death. This might be interpreted as both recent exposure and decades of exposure as being of relevance, perhaps explained by effects of air pollution on chronic processes important for the development and progression of diabetes. Alternatively, the similar MMRs for the different exposure periods might be explained by the high correlations between these exposure measures (ESM Table 3). We found an association between NO2 concentration and diabetes mortality but NO2 is ‘only’ an indicator of vehicle engine exhaust, which is a complex mixture of many chemicals, including particulate matter with absorbed polycyclic aromatic hydrocarbons, transition metals and other substances that can cause oxidative stress [45, 46] and inflammation [12, 47, 48]. These mechanisms are considered relevant for the development of type 2 diabetes [9, 12, 13, 20, 46]. Thus, although we found an association with NO2 other pollutants correlating with NO2 might be responsible for the association with diabetes mortality.
Three prospective cohort studies have investigated air pollution and diabetes incidence. The first study [20] assessed traffic-related air pollution levels at the baseline addresses of 1,775 non-diabetic elderly women from the Study on the Influence of Air Pollution on Lung, Inflammation and Aging (SALIA) and living in the Ruhr area, Germany. Median NO2 levels were estimated to be 41.7 μg/m3, which is considerably higher than in the present study (15.1 μg/m3). The results showed associations between risk for development of type 2 diabetes and NO2 at the nearest monitoring station, emissions of particulate matter and NO2 from traffic, soot and NO2 assessed by land-use regression models and proximity to major roads. The associations were stronger among women with high serum concentrations of complement factor C3c at baseline, which is a surrogate marker of subclinical inflammation. The second study [21] assessed exposure to particulate matter and distance to the nearest road at the home addresses of 74,412 female participants in the Nurses' Health Study and 15,048 male participants in the Health Professionals Follow Up study. The results showed that there was a weak statistically non-significant increased risk of incident type 2 diabetes associated with particulate matter in both cohorts and a statistically significant association between short distance to road and risk for incident type 2 diabetes among women in the Nurses' Health Study but not among males in the Health Professionals Follow Up Study. The third study [22] followed up 51,818 members of the Danish Diet Cancer and Health cohort for incident diabetes. The type of diabetes was not registered but since the study population was aged 50 years or more, the vast majority of incident cases was expected to be type 2. Exposure to NO2 at home addresses was borderline significantly associated with risk for confirmed diabetes. These results were based on the same cohort as used in the present study. Despite only including a limited number of diabetes-related deaths, the present study showed a statistically significant association between long-term exposure to traffic-related air pollution and diabetes mortality. This result is generally in line with the findings from the three cohort studies that there was an association between traffic-related air pollution and diabetes incidence and also with results of a study [23] that showed higher diabetes mortality among construction workers exposed to diesel engine exhaust. Two previous cross-sectional studies have shown an association between air pollution and diabetes prevalence [14, 15]; the median NO2 levels in one of these studies (15 and 23 μg/m3 in the two subpopulations) [15] were comparable with those in the present study (15 μg/m3). Finally, time-series [17, 18] and case-crossover studies [19] have linked short-term variations in air pollution with diabetes mortality.
Our previous study of diabetes in the Diet Cancer and Health cohort showed, as expected, higher prevalence of several risk factors at baseline among participants who developed diabetes compared with the cohort [22]. The present study showed that most diabetes risk factors were even more prevalent among cohort members who died from diabetes. When comparing the cohort (n = 51,818; incidence study), incident diabetes cases (n = 2,877) and those who died due to diabetes (n = 122), 47, 59 and 75% were men, 36, 40 and 61% were smokers, 45, 59 and 81% were physically inactive (sports) and the fat intake was 81.2, 82.2 and 85.0 g/day, respectively. Thus, risk factors seem to be identified more clearly when studying diabetes mortality compared with diabetes incidence. The same pattern was seen for air pollution, with respective median NO2 levels being 14.5, 15.1 and 18.1 μg/m3 (i.e. 4% higher among incident cases and 20% higher among those who died due to diabetes compared with the cohort). Mortality depends on both incidence and survival and since air pollution might influence both the development of diabetes and the progression towards mortality it would be desirable to unravel the separate contributions. In the Diet Cancer and Health cohort, however, the time of the diabetes diagnosis was unknown for the majority of those who died from diabetes, precluding a meaningful study of survival after a diabetes diagnosis.
Adjustment for potential confounders (in addition to age and sex) decreased the MRRs substantially (Tables 2, 3), which was due to the adjustment for smoking status, alcohol intake, physical activity and BMI. Each of these factors was associated with both death due to diabetes and the level of air pollution in this study (Table 1) and, thus, confounding by these factors is not surprising. We had no information about the severity of diabetes among cohort members precluding adjustment for this predictor of diabetes mortality.
In line with one previous study on diabetes incidence in same cohort [22] we found a stronger association between NO2 and diabetes mortality in never compared with ever smokers. If our result reflects a true effect modification, the absolute number of diabetes-related deaths due to air pollution might not be higher in never smokers because the crude diabetes mortality rate in never smokers was less than one-third of that in ever smokers in this study.
Physical activity is important for prevention and management of type 2 diabetes [49]. In accordance, this study showed a fivefold higher crude mortality rate among those who were inactive compared with those who participated in leisure-time sports. If our result showing a stronger association between air pollution and diabetes mortality among the physically inactive represents a true effect modification, then physical inactivity could be even more harmful than indicated by the fivefold higher crude mortality rate, and active participation in sports might reduce or even eliminate the risk of dying from diabetes because of exposure to air pollution.
This study is based on a cohort of elderly white people recruited from the general population. The cohort participants generally had a longer education than non-participants [24] but the association between air pollution and diabetes mortality was not significantly modified by educational level (Table 4). The results can probably be generalised to most ‘western’ populations exposed to similar levels of air pollution.
In conclusion, this cohort study shows that there is a significant association between long-term exposure to traffic-related air pollution at residential addresses and mortality from diabetes after adjustment for potential confounders. Although in line with the limited epidemiological evidence for diabetes incidence, this first result for long-term exposure to ambient air pollution and diabetes mortality needs confirmation.
Abbreviations
- GIS:
-
Geographical information system
- ICD:
-
International Classification of Diseases
- MRR:
-
Mortality-rate ratio
References
Jaidane H, Sauter P, Sane F, Goffard A, Gharbi J, Hober D (2010) Enteroviruses and type 1 diabetes: towards a better understanding of the relationship. Rev Med Virol 20:265–280
Hathout EH, Beeson WL, Nahab F, Rabadi A, Thomas W, Mace JW (2002) Role of exposure to air pollutants in the development of type 1 diabetes before and after 5 yr of age. Pediatr Diabetes 3:184–188
Vehik K, Dabelea D (2011) The changing epidemiology of type 1 diabetes: why is it going through the roof? Diabetes Metab Res Rev 27:3–13
Nolan CJ, Damm P, Prentki M (2011) Type 2 diabetes across generations: from pathophysiology to prevention and management. Lancet 378:169–181
van Dieren S, Beulens JW, van der Schouw YT, Grobbee DE, Neal B (2010) The global burden of diabetes and its complications: an emerging pandemic. Eur J Cardiovasc Prev Rehabil 17(Suppl 1):S3–S8
Willi C, Bodenmann P, Ghali WA, Faris PD, Cornuz J (2007) Active smoking and the risk of type 2 diabetes: a systematic review and meta-analysis. JAMA 298:2654–2664
Zhang L, Curhan GC, Hu FB, Rimm EB, Forman JP (2011) Association between passive and active smoking and incident type 2 diabetes in women. Diabetes Care 34:892–897
Ko KP, Min H, Ahn Y et al (2011) A prospective study investigating the association between environmental tobacco smoke exposure and the incidence of type 2 diabetes in never smokers. Ann Epidemiol 21:42–47
Bhatnagar A (2009) Could dirty air cause diabetes? Circulation 119:492–494
Brook RD, Rajagopalan S, Pope CA III et al (2010) Particulate matter air pollution and cardiovascular disease: an update to the scientific statement from the American Heart Association. Circulation 121:2331–2378
Wellen KE, Hotamisligil GS (2005) Inflammation, stress, and diabetes. J Clin Invest 115:1111–1119
Sun Q, Yue P, Deiuliis JA et al (2009) Ambient air pollution exaggerates adipose inflammation and insulin resistance in a mouse model of diet-induced obesity. Circulation 119:538–546
Yan YH, Chou CC, Lee CT, Liu JY, Cheng TJ (2011) Enhanced insulin resistance in diet-induced obese rats exposed to fine particles by instillation. Inhal Toxicol 23:507–519
Pearson JF, Bachireddy C, Shyamprasad S, Goldfine AB, Brownstein JS (2010) Association between fine particulate matter and diabetes prevalence in the U.S. Diabetes Care 33:2196–2201
Brook RD, Jerrett M, Brook JR, Bard RL, Finkelstein MM (2008) The relationship between diabetes mellitus and traffic-related air pollution. J Occup Environ Med 50:32–38
Dijkema MB, Mallant SF, Gehring U et al (2011) Long-term exposure to traffic-related air pollution and type 2 diabetes prevalence in a cross-sectional screening-study in the Netherlands. Environ Health 10:76
Kan H, Jia J, Chen B (2004) The association of daily diabetes mortality and outdoor air pollution in Shanghai, China. J Environ Health 67:21–26
Ostro B, Broadwin R, Green S, Feng WY, Lipsett M (2006) Fine particulate air pollution and mortality in nine California counties: results from CALFINE. Environ Health Perspect 114:29–33
Maynard D, Coull BA, Gryparis A, Schwartz J (2007) Mortality risk associated with short-term exposure to traffic particles and sulfates. Environ Health Perspect 115:751–755
Kramer U, Herder C, Sugiri D et al (2010) Traffic-related air pollution and incident type 2 diabetes: results from the SALIA cohort study. Environ Health Perspect 118:1273–1279
Puett RC, Hart JE, Schwartz J, Hu FB, Liese AD, Laden F (2011) Are particulate matter exposures associated with risk of type 2 diabetes? Environ Health Perspect 119:384–389
Andersen ZJ, Raaschou-Nielsen O, Ketzel M et al (2012) Diabetes incidence and long-term exposure to air pollution. Diabetes Care 35:92–98
Finkelstein MM (2008) Diesel particulate exposure and diabetes mortality among workers in the Ontario construction trades. Occup Environ Med 65:215
Tjonneland A, Olsen A, Boll K et al (2007) Study design, exposure variables, and socioeconomic determinants of participation in Diet, Cancer and Health: a population-based prospective cohort study of 57,053 men and women in Denmark. Scand J Public Health 35:432–441
Helweg-Larsen K (2011) The Danish Register of Causes of Death. Scand J Public Health 39:26–29
Jensen SS, Berkowicz R, Hansen SH, Hertel O (2001) A Danish decision-support GIS tool for management of urban air quality and human exposures. Transp Res Part D Transp Environ 6:229–241
Raaschou-Nielsen O, Hertel O, Vignati E et al (2000) An air pollution model for use in epidemiological studies: evaluation with measured levels of nitrogen dioxide and benzene. J Expo Anal Environ Epidemiol 10:4–14
Berkowicz R, Ketzel M, Jensen SS, Hvidberg M, Raaschou-Nielsen O (2008) Evaluation and application of OSPM for traffic pollution assessment for large number of street locations. Environ Model Software 23:296–303
Ketzel M, Berkowicz R, Hvidberg M, Jensen SS, Raaschou-Nielsen O (2011) Evaluation of AIRGIS–a GIS-based air pollution and human exposure modelling system. Int J Environ Pollut 47:226–238
Harrel FE (2001) Regression modeling strategies. Springer, New York
Tjonneland A, Overvad K, Haraldsdottir J, Bang S, Ewertz M, Jensen OM (1991) Validation of a semiquantitative food frequency questionnaire developed in Denmark. Int J Epidemiol 20:906–912
Tjonneland A, Haraldsdottir J, Overvad K, Stripp C, Ewertz M, Jensen OM (1992) Influence of individually estimated portion size data on the validity of a semiquantitative food frequency questionnaire. Int J Epidemiol 21:770–777
Raaschou-Nielsen O, Bak H, Sorensen M et al (2010) Air pollution from traffic and risk for lung cancer in three Danish cohorts. Canc Epidemiol Biomarkers Prev 19:1284–1291
Raaschou-Nielsen O, Andersen ZJ, Hvidberg M et al (2011) Lung cancer incidence and long-term exposure to air pollution from traffic. Environ Health Perspect 119:860–865
Andersen ZJ, Hvidberg M, Jensen SS et al (2011) Chronic obstructive pulmonary disease and long-term exposure to traffic-related air pollution: a cohort study. Am J Respir Crit Care Med 183:455–461
Raaschou-Nielsen O, Andersen ZJ, Hvidberg M et al (2011) Air pollution from traffic and cancer incidence: a Danish cohort study. Environ Health 10:67
Andersen ZJ, Bonnelykke K, Hvidberg M et al (2011) Long-term exposure to air pollution and asthma hospitalisations in older adults: a cohort study. Thorax 67:6–11
Dosemeci M, Wacholder S, Lubin JH (1990) Does nondifferential misclassification of exposure always bias a true effect toward the null value? Am J Epidemiol 132:746–748
Fuller JH, Elford J, Goldblatt P, Adelstein AM (1983) Diabetes mortality: new light on an underestimated public health problem. Diabetologia 24:336–341
McEwen LN, Kim C, Haan M et al (2006) Diabetes reporting as a cause of death: results from the Translating Research Into Action for Diabetes (TRIAD) study. Diabetes Care 29:247–253
Rao C, Adair T, Bain C, Doi SA (2012) Mortality from diabetic renal disease: a hidden epidemic. Eur J Public Health 22:280–284
Fuller JH, Stevens LK, Wang SL (2001) Risk factors for cardiovascular mortality and morbidity: the WHO Mutinational Study of Vascular Disease in Diabetes. Diabetologia 44(Suppl 2):S54–S64
Morrish NJ, Wang SL, Stevens LK, Fuller JH, Keen H (2001) Mortality and causes of death in the WHO Multinational Study of Vascular Disease in Diabetes. Diabetologia 44(Suppl 2):S14–S21
Carstensen B, Witte DR, Friis S (2012) Cancer occurrence in Danish diabetic patients: duration and insulin effects. Diabetologia 55:948–958
Moller P, Jacobsen NR, Folkmann JK et al (2010) Role of oxidative damage in toxicity of particulates. Free Radic Res 44:1–46
Xu Z, Xu X, Zhong M et al (2011) Ambient particulate air pollution induces oxidative stress and alterations of mitochondria and gene expression in brown and white adipose tissues. Part Fibre Toxicol 8:20
Sun Q, Wang A, Jin X et al (2005) Long-term air pollution exposure and acceleration of atherosclerosis and vascular inflammation in an animal model. JAMA 294:3003–3010
Chen JC, Schwartz J (2008) Metabolic syndrome and inflammatory responses to long-term particulate air pollutants. Environ Health Perspect 116:612–617
Colberg SR, Sigal RJ, Fernhall B et al (2010) Exercise and type 2 diabetes: the American College of Sports Medicine and the American Diabetes Association: joint position statement. Diabetes Care 33:e147–e167
Acknowledgements
We thank M. Hvidberg, Department of Environmental Science, Aarhus University, Roskilde, Denmark, for geocoding the address data and calculating the traffic exposure variables.
Funding
The project was supported by the Danish Agency for Science, Technology and Innovation, as part of the Danish Centre of Excellence on Air Pollution and Health, AIRPOLIFE (grant 2052-03-0016) and by the Danish Cancer Society. These funding agencies had no role in the design, data collection, analyses or interpretation of the data, writing the manuscript, the decision to submit the manuscript or any other aspect of the scientific work.
Duality of interest
The authors declare that there is no duality of interest associated with this manuscript.
Contribution statement
ORN conceived and designed the study, participated in acquisition of environmental data and exposure assessment, participated in planning data analyses and drafted the manuscript. ZJA participated in planning the statistical analyses and performed record linkages, data processing and statistical analyses. MK and OH developed the air pollution modelling system and conducted the air pollution calculations. AT and KO established the Diet, Cancer and Health cohort and provided cohort data. All authors participated in preparing the analyses and interpretation of the data, critically revised the manuscript and approved the final manuscript for publication.
Author information
Authors and Affiliations
Corresponding author
Additional information
K. Overvad and Z. J. Andersen contributed equally to this study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM Methods
(PDF 31 kb)
ESM Table 1
(PDF 10 kb)
ESM Table 2
(PDF 10 kb)
ESM Table 3
(PDF 47 kb)
Rights and permissions
About this article
Cite this article
Raaschou-Nielsen, O., Sørensen, M., Ketzel, M. et al. Long-term exposure to traffic-related air pollution and diabetes-associated mortality: a cohort study. Diabetologia 56, 36–46 (2013). https://doi.org/10.1007/s00125-012-2698-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-012-2698-7