Abstract
Aims/hypothesis
Gestational diabetes mellitus is a heterogeneous disorder characterised by impaired insulin secretion and action. Our aim was to study whether autoimmunity, variations in genes affecting insulin secretion and action, or both, contribute to the development of gestational diabetes and whether the pathogenesis of the disease differs between women with a Scandinavian or Arabian background.
Methods
We studied a total of 500 unrelated women with gestational diabetes (400 Scandinavian and 100 Arabian) and 550 unrelated pregnant non-diabetic control women (428 Scandinavian and 122 Arabian) matched for ethnicity.
Results
Arabian women with gestational diabetes were 50% more insulin resistant for the same BMI compared with Scandinavian women with the disease (homeostasis model assessment [HOMA-IR]; 3.2±0.3 vs 2.2±0.2, p=0.02). Both Scandinavian (4.2% vs 0.9%, p=0.008) and Arabian (4.6% vs 0.0%, p=0.03) women with gestational diabetes had a higher frequency of GAD antibodies (GAD65Ab) than the matched controls. The frequency of HLA-DQB1 risk genotypes was slightly higher in Scandinavian women with gestational diabetes than in the Scandinavian controls (46.3% vs 38.8%, p=0.03) but no significant difference was found between the Arabian women with gestational diabetes and the Arabian controls (47% vs 51.6%, p=0.47). There were no significant differences in the frequency of the insulin gene variable number of tandem repeat (INS VNTR) alleles and genotypes or the peroxisome proliferator-activated receptor-gamma 2 (PPARγ2-Pro12Ala) polymorphism between the women with gestational diabetes and the control women either in Arabian or in Scandinavian women.
Conclusions/interpretation
Gestational diabetes mellitus was associated with the presence of GAD65Ab in both study groups. Scandinavian women with gestational diabetes may share some genetic features with Type 1 diabetes. In addition, Arabian women with gestational diabetes are more insulin resistant than Scandinavian women with gestational diabetes and with the same BMI.
Similar content being viewed by others
Introduction
Gestational diabetes mellitus (GDM) is defined as carbohydrate intolerance with onset or first recognition during pregnancy [1]. It is characterised by impaired insulin secretion and action [2, 3]. Gestational diabetes complicates about 1 to 3% of all pregnancies in the western world [4], whereas higher rates are reported among small ethnic groups [5]. There is no international consensus regarding the definition of diagnostic criteria for GDM. In Sweden the diagnosis of GDM is based on a 75-g OGTT and defined as a 2-h capillary glucose concentration of at least 9 mmol/l. According to these criteria approximately 1.2% of pregnant women in Sweden develop GDM [6]. In Arabian women a GDM prevalence from 5 to 38% has been reported [7, 8]. Although most women with GDM revert to normal after delivery, impaired glucose tolerance and/or diabetes develop in about 50% within 10 years postpartum [9, 10]. Women with GDM often have a history of maternal diabetes, which suggests a genetic component for the disease [11]. Moreover, the offspring of women with abnormal glucose tolerance during pregnancy are at a higher risk of developing insulin resistance, obesity or diabetes at an early age [12]. To date, several genetic studies have been carried out to identify susceptibility genes predisposing for the development of GDM. Associations have been reported between GDM and variants in the glucokinase [13], mitochondrial DNA [14, 15], β3-adrenergic receptor [16], sulphonylurea receptor 1 (SUR1) [17], insulin receptor and insulin-like growth factor 2 (IGF2) genes [18]. Some of these associations have not been replicated [19, 20]. This inconsistency may be due, in part, to ethnic heterogeneity between different populations.
HLA class II alleles on the short arm of chromosome 6 and autoantibodies including islet cell antibodies (ICA), GAD65 autoantibodies and insulin autoantibodies (IAA) are strongly associated with immune-mediated Type 1 diabetes, which is characterised by beta-cell destruction and absolute insulin deficiency [21]. Increased frequencies of HLA-risk antigens and high prevalence of ICA, insulinoma-associated antigen 2 (IA-2) and GAD antibodies have also been reported in women with GDM [22, 23].
Studies have shown that variation in the variable number of tandem repeat (VNTR) mini-satellite located in the promoter region of the insulin gene (INS) is associated with several diseases or phenotypes including Type 1 diabetes, central obesity, insulin resistance, polycystic ovary syndrome, birth weight and Type 2 diabetes [24, 25, 26]. Depending on the number of repeats, INS VNTR can be divided into class I (26–63 repeats), II (64–140 repeats) and III (141–209 repeats) [27]. The number of repeats is considered to influence expression of the insulin gene in both the thymus and the pancreas [28, 29]. Whereas the class I allele has been associated with increased risk of Type 1 diabetes, the class III genotype has been suggested to increase risk of Type 2 diabetes. Cross-sectional studies have shown that the protective Ala allele of the PPARγ2-Pro12Ala polymorphism is associated with reduced risk of Type 2 diabetes [30]. The maternally inherited mutation A3243G in the mitochondrial tRNA leu (UUR) gene is associated with maternally inherited diabetes and deafness (MIDD), which is characterised by pancreatic beta cell dysfunction [31].
We investigated whether autoimmunity, variations in genes affecting insulin secretion and action, or both, contribute to the development of GDM and whether GDM pathogenesis differs between women with a Scandinavian or Arabian background.
Subjects and methods
Study population
All pregnant women in the southern part of Sweden are routinely offered a 75-g OGTT at 27 to 28 weeks of pregnancy. The tests are carried out in the local antenatal care clinics, using HemoCue devices (HemoCue, Ängelholm, Sweden) for capillary whole blood analysis. Women at high risk (previous GDM or a family history of diabetes) are also offered an OGTT at 12 to 13 weeks of pregnancy. GDM is defined as a 2-h capillary glucose concentration (double-test) of at least 9 mmol/l. We recruited 500 unrelated GDM women (400 Scandinavian and 100 Arabian) and 550 unrelated non-diabetic pregnant controls (428 Scandinavian and 122 Arabian) consecutively from the screening procedure in southern Sweden. The Arabian women were immigrants from most of the Arab countries (Iraq, Lebanon, Morocco, Palestine, Syria, etc.). The reason for the different sample size between the two populations was the limited number of Arabs living in Sweden. The clinical and metabolic characteristics were available only for GDM women living in the city of Malmö who were invited to take part in a 5-year follow-up study with repeated OGTTs at 1, 2 and 5 years postpartum. The population in the southern part of Sweden is very homogenous and we therefore considered this subset to be representative of the larger group of 500 women with GDM. Before participating in the study, the purpose, nature and potential risks were explained, and informed written voluntary consent was obtained from each subject. The study protocol was approved by the ethics committee of Lund University.
Genetic analyses
A3243G mutation in the mitochondrial tRNAleu gene
Total DNA was isolated from peripheral blood lymphocytes or blood samples were collected as dried blood spots on Whatman filters (VWR International, Stockholm, Sweden), and punch-outs in 96-well plates were soaked directly in PCR amplification buffer. PCR was carried out using primers specific to mtDNA [31]. A 427-bp fragment was digested overnight with ApaI (New England Biolabs, Beverly, Mass., USA) at 37 °C. Samples were electrophoresed on 5% polyacrylamide gel under non-denaturing conditions and stained with ethidium bromide to visualise the fragments using GELSCAN2000 (Applied Biosystems, Foster City, Calif., USA).
HLA-DQB1 genotyping
The second exon of the DQB1 gene was amplified using biotinylated PCR primers as described previously with modification of the forward primer (5′-CA TGT GCT ACT TCA CCA ACG G) [32]. After amplification, DNA was captured onto streptavidin-coated microtitre wells and denatured using mild alkaline solution. Hybridisation was done with a panel of lanthanide-labelled probes specific for HLA-DQB1 alleles and with a probe controlling DNA amplification. We used five probes to distinguish DQB1 alleles. Of them, four (0602/3, 0201, 0301 and 0302) have been described previously [32] in addition to (0603/4; 5′-TTG TTA CCA GAC ACA). After washing and adding the enhancement solution, several fluorescent signals were detected simultaneously by time-resolved flurometry using Victor 2 (Wallac Oy, Turku, Finland).
Hph1 polymorphism genotyping of the INS VNTR
The T/A polymorphism located 23 bp 5′ of the start codon is in linkage disequilibrium with VNTR alleles. The T allele is in linkage disequilibrium with the short (Class I) and the A allele with the long (Class III) VNTR alleles [24]. We used a restriction fragment length polymorphism method involving digestion of the PCR-amplified DNA with HphI (New England Biolabs, Beverly, Mass., USA) enzyme [33]. The VNTR classes were inferred directly from the Hph1 genotypes. The T/T genotype was referred to as I/I, the T/A as I/III and the A/A as III/III.
PPARγ2-Pro12Ala genotyping
The exon B of the PPARγ2 gene was genotyped by PCR-RFLP using primers 5′-GAT AGA GAC AAA ATA TCA GTG (forward primer) and 5′-GTA TCA GTG AAG GAA TCG CTT TCC G (reverse primer). PCR was carried out with 25 ng genomic DNA or dried blood spots in a total volume of 20 µl containing 1×(NH4)2SO4-buffer [16 mmol/l (NH4)2SO4, 67 mmol/l TRIS pH 8.8, 0.01 TWEEN 20], 10 µmol/l each dNTP, 2.4 mmol/l MgCl2, 0.5 U Taq polymerase (Amersham Pharmacia Biotech, Uppsala, Sweden), 1.5% Formamide and 10 pmol of each primer. The cycling conditions were 94 °C for 5 min, 35 cycles of 94 °C for 30 s, 56 °C for 30 s and 72 °C for 60 s followed by final extension at 72 °C for 10 min. PCR was followed by digestion with BstUI (New England Biolabs, Beverly, Mass., USA) at 60 °C for 2 h, and digests were separated on 4.5% aragose gel (SeaKem, Rockland, Me., USA) and stained with ethidium bromide to visualise the fragments. The Pro12 allele gives a 113-bp fragment, whereas the Ala12 allele gives fragments of 87 bp and 25 bp.
GAD65 autoantibodies (GAD65Ab)
GAD65Ab were measured by a radio-immunoprecipitation assay using 35S-labelled recombinant human GAD65 produced by coupled in vitro transcription-translation as described [34]. Punch-outs from dried blood spots were incubated in assay buffer overnight to elute antibodies [34]. The results are expressed as relative units (RU): RU=(sample cpm−mean cpm of three negative controls)/(cpm of a positive internal reference−mean cpm of three negative controls)×100. The cut-off limit for positivity was 5 RU. According to standardised international units, 5 RU is equal to 32 U/ml. At the Combined Autoantibody Workshop [35], the specificity and sensitivity of the GAD65Ab assay were 99 and 75% respectively. GAD65Ab were analysed in all control subjects and in 376 GDM women (289 Scandinavian and 87 Arabian).
Metabolic measurements
Blood glucose was measured using HemoCue devices or by a glucose oxidation method. Serum insulin concentrations were measured using an enzyme immunoassay from Dako (Cambridgeshire, UK). BMI was calculated as weight/height2 (kg/m2). Homeostasis model assessment (HOMA-IR; fasting serum insulin × fasting plasma glucose/22.5) was used to estimate the degree of insulin resistance [36]. Beta cell function was estimated as the insulinogenic index during the first 30 min of the OGTT (I/G30: serum insulin 30 min−fasting serum insulin/plasma glucose 30 min−fasting plasma glucose) [37]. Since insulin resistance is known to modulate insulin secretion, we adjusted insulin secretion measured as I/G30 for insulin resistance by dividing I/G30 by the HOMA-IR [38].
Statistical analyses
Clinical data are presented as means ± SEM. Significance of differences between group means was tested by the Mann-Whitney U test or analysis of variance or covariance (ANCOVA) with BMI and PPARγ2 genotype as covariates. Logarithmic transformation was used for data with right-skewed distribution. Allele and genotype frequencies were compared between groups by chi square or Fisher’s exact test. The statistical analyses were carried out using the Number Cruncher Statistical Systems (NCSS, Kaysville, Utah, USA) and BMDP Statistical Software, Version 1.12 (BMDP, Los Angeles, Calif., USA). Two-sided p values of less than 0.05 were considered statistically significant.
Results
The Arabian GDM women had a higher HOMA-IR index (3.2±0.3 vs 2.2±0.2, p=0.02) and a lower disposition index, i.e. their beta cell compensation for the degree of insulin resistance [(I/G30)/HOMA-IR] was impaired (3.3±0.6 vs 5.7±0.6, p=0.01), compared with Scandinavian GDM women after adjustment for BMI (Table 1).
GAD65 autoantibodies
The presence of GAD65Ab was associated with GDM in both study populations. Among Scandinavian women with GDM, 12/289 (4.2%) were positive for GAD65Ab compared with 4/428 (0.9%, p=0.008) in the controls. Similar frequency was observed in Arabians where 4/87 (4.6%) of GDM women were positive for GAD65Ab compared with 0/122 (0.0%, p=0.03) in the controls.
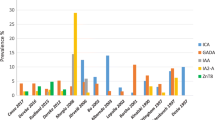
HLA-DQB1 genotypes
The frequency of HLA-DQB1*0201/0302 or *0201/X or *0302/X (X excludes 0602/3) risk genotypes was slightly higher in Scandinavian women with GDM than in the Scandinavian controls (46.3% vs 38.8%, p=0.03; corrected p value for multiple comparisons p>0.1) but no significant difference was seen between Arabian women with GDM and the Arabian controls (47% vs 51.6%, p=0.47) (Table 2). In Scandinavian GDM patients, the presence of GAD65Ab was associated with HLA-DQB1 risk genotypes (p=0.04).
PPARγ2
The Pro12Ala allele and genotype frequencies of the PPARγ2 gene are shown in Table 3. There was no significant difference in the frequency of the Pro12Ala variant between Arabian or Scandinavian women with GDM and the controls matched for race. We also tested whether, as previously shown, there was a difference in HOMA-IR between carriers of the different PPARγ2 genotypes. In this study, HOMA-IR also differed significantly between carriers of the Ala/Ala or Pro/Ala and Pro/Pro (1.9±0.1 vs 2.5±0.2, p=0.11; one-tailed p value <0.05) genotypes. However, HOMA-IR still differed significantly between Arabian and Scandinavian GDM women after adjusting for the PPARγ2-Pro12Ala genotype (p=0.02).
INS VNTR
There were no significant differences in the frequency of the INS VNTR alleles or genotypes between GDM and control subjects in either Arabian or Scandinavian women (Table 4).
The A3243G mutation in the mitochondrial tRNA leu gene was rare in the study populations. It was found in only one Arabian (1.0%) and one Scandinavian (0.3%) woman with GDM but not in the controls. The Arabian GDM woman had a maternal history of diabetes. She was 38 years old at the time of diagnosis, had a fasting C-peptide concentration of 0.28 nmol/l and was GAD65Ab negative. She had no hearing loss. The Scandinavian woman had no family history of diabetes. She was 34 years old at diagnosis and also GAD65Ab negative. She had no hearing loss.
Discussion
We demonstrate that the relative distribution of genotypes conferring risk for Type 1 diabetes and variants known to impair insulin secretion and action differ between Scandinavian and immigrant Arabian women living in Sweden. Our finding that Scandinavian women with GDM have a higher frequency of GAD65Ab than Scandinavian control women supports a Finnish study that concluded that GDM in some Scandinavian women may represent an autoimmune form of diabetes [39]. A similar difference was observed between Arabian GDM and control women, suggesting that autoimmunity may contribute to the development of GDM in Arabian women as well. To our knowledge, this is the largest report on GAD65Ab in GDM and control women and the first report studying the potential role of GAD65Ab in Arabian GDM women. Whether Type 1 diabetes-associated markers such as GAD65Ab, ICA and insulin autoantibodies are associated with GDM is, however, still controversial. A lower frequency (2.2%) of GAD65Ab was reported in GDM women from other Scandinavian countries [40]. The frequency of GAD65Ab has been shown to vary between different populations. In Maine (USA), about 6% of the women with GDM were positive for GAD65Ab [41], whereas the frequency in GDM women from Germany was as high as 9.5% [23]. In Italy, the frequency of GAD65Ab varied from 0 to 3.6% in GDM women [42, 43]. Although the confidence interval for these frequencies may overlap, it suggests a significant contribution of Type 1 diabetes in the GDM population in some but not all populations. These discrepancies between studies might be due to differences in selection criteria, in ethnic background of the subjects and in GAD65Ab assay methodology. In our study, GDM women were recruited irrespectively of the type of treatment or family history of diabetes.
In a previous smaller study, we found that the HLA-DQB1 *02/X (X excludes 0302 or 0602/3) was significantly increased in Swedish GDM women who had a family history of diabetes compared with subjects with NGT, but no significant difference was observed in the frequency of GAD65Ab [44]. In the present study, Scandinavian GDM women had a slightly higher frequency of HLA-DQB1 risk genotypes than the Scandinavian controls. However, these differences were not statistically significant after adjustment for multiple comparisons (corrected p value for multiple comparisons p>0.1). This may, however, represent an over correction, as the HLA genotypes tested are in strong linkage disequilibrium [45] and thereby do not represent independent observations. A report showed a two-fold increase in the frequency of HLA-DR3 and -DR4 antigens in GDM compared with the controls matched for race, and the increase was statistically significant in black women from the United States [22]. Another study found no significant difference in the frequency distribution of HLA-DQB1, -DQA1 and -DRB1 alleles between Caucasian GDM and control women from Germany [46].
A higher frequency of GDM in populations with a high frequency of Type 2 diabetes has been reported [47]. As Type 2 diabetes is more common in the Arabian population [48] compared with Scandinavians [49], we hypothesised that Arabian GDM women would be more insulin resistant than Scandinavian GDM women. This was the case; the Arabian GDM women were 50% more insulin resistant than Scandinavian GDM women, as judged from the HOMA-IR index (3.2±0.3 vs 2.2±0.2, p=0.02). Importantly, this difference was not due to differences in BMI (Fig. 1). We did not observe a significant difference in the frequency of the Pro12Ala variant between the GDM women and the controls in either Arabian or Scandinavian women. This may simply represent a power issue, as the sample size required to demonstrate associations with a susceptibility allele with a relative risk in the range of 1.2 clearly exceeds the numbers included in this study and most studies on GDM. Given the previous data on a genotype–phenotype correlation between the Pro12Ala polymorphism of the PPARγ2 gene [30, 50, 51] and the current finding of a difference in HOMA-IR between carriers of the PPARγ2 genotypes, this polymorphism may partly explain the difference seen in HOMA-IR between the Arabian and Scandinavian women with GDM. However, since adjusting the ethnic difference in HOMA-IR for genotype did not abolish the difference between the two groups, other factors must also contribute to the difference.
A possible association between INS VNTR and GDM has only been investigated in GDM women from Greece. The INS VNTR III/III genotype was shown to be more frequent in GDM women than in the controls (8.7% vs 2.7%, p=0.02) [52]. In our study, there were no differences in allele or genotype frequencies of the INS VNTR between the GDM women and the controls in either, Arabian or Scandinavian women. This discrepancy between the results may be due to ethnic differences and the use of different diagnostic criteria.
The role of mitochondrial mutations in the pathogenesis of GDM has also been studied in different populations. The A3243G mutation was reported in one of twelve Japanese women with GDM [15]. A T to C substitution at nucleotide 3398 in the mitochondrial ND1 gene was associated with GDM in women from Singapore [14]. The frequency of the A3243G mutation in mitochondrial tRNA leu gene was rare in our study in women with GDM, thus excluding it as an important susceptibility factor for GDM, which is consistent with previous observations in other populations [14, 19].
In conclusion, we demonstrate in a large study that GDM is associated with the presence of GAD65Ab in both study populations. Scandinavian women with GDM may share some genetic features with Type 1 diabetes. In addition, Arabian women with GDM were approximately 50% more insulin resistant than Scandinavian women with GDM and with the same BMI.
Abbreviations
- GAD65Ab:
-
GAD antibodies
- GDM:
-
Gestational diabetes mellitus
- INS VNTR :
-
Insulin gene variable number of tandem repeat
- mtDNA:
-
Mitochondrial DNA
- PPARγ2 :
-
Peroxisome proliferator-activated receptor-gamma2
References
Metzger BE, Coustan DR, the Organizing Committee (1998) Summary and recommendations of the Fourth International Workshop-Conference on Gestational Diabetes Mellitus. Diabetes Care 21 [Suppl 2]:B161–B167
Buchanan TA, Metzger BE, Freinkel N, Bergman RN (1990) Insulin sensitivity and B-cell responsiveness to glucose during late pregnancy in lean and moderately obese women with normal glucose tolerance or mild gestational diabetes. Am J Obstet Gynecol 162:1008–1014
Ryan EA, O’Sullivan MJ, Skyler JS (1985) Insulin action during pregnancy. Studies with the euglycemic clamp technique. Diabetes 34:380–389
Hadden DR (1985) Geographic, ethnic, and racial variations in the incidence of gestational diabetes mellitus. Diabetes 34 [Suppl 2]:8–12
Yue DK, Molyneaux LM, Ross GP, Constantino MI, Child AG, Turtle JR (1996) Why does ethnicity affect prevalence of gestational diabetes? The underwater volcano theory. Diabet Med 13:748–752
Aberg A, Rydhstroem H, Frid A (2001) Impaired glucose tolerance associated with adverse pregnancy outcome: a population-based study in southern Sweden. Am J Obstet Gynecol 184:77–83
El-Shafei AM, Bashmi YA, Beischer NA, Henry OA, Walstab JE (1989) Incidence and severity of gestational diabetes in Bahrain and Australia. Aust NZ J Obstet Gynaecol 29:204–208
Agarwal MM, Hughes PF, Punnose J, Ezimokhai M, Thomas L (2001) Gestational diabetes screening of a multiethnic, high-risk population using glycated proteins. Diabetes Res Clin Pract 51:67–73
Mohammed N, Dooley J (1998) Gestational diabetes and subsequent development of NIDDM in aboriginal women of northwestern Ontario. Int J Circumpolar Health 57:355–358
Damm P (1998) Gestational diabetes mellitus and subsequent development of overt diabetes mellitus. Dan Med Bull 45:495–509
Martin AO, Simpson JL, Ober C, Freinkel N (1985) Frequency of diabetes mellitus in mothers of probands with gestational diabetes: possible maternal influence on the predisposition to gestational diabetes. Am J Obstet Gynecol 151:471–475
Pettitt DJ, Bennett PH, Saad MF, Charles MA, Nelson RG, Knowler WC (1991) Abnormal glucose tolerance during pregnancy in Pima Indian women. Long-term effects on offspring. Diabetes 40 [Suppl 2]:126–130
Ellard S, Beards F, Allen LI et al. (2000) A high prevalence of glucokinase mutations in gestational diabetic subjects selected by clinical criteria. Diabetologia 43:250–253
Chen Y, Liao WX, Roy AC, Loganath A, Ng SC (2000) Mitochondrial gene mutations in gestational diabetes mellitus. Diabetes Res Clin Pract 48:29–35
Yanagisawa K, Uchigata Y, Sanaka M et al. (1995) Mutation in the mitochondrial tRNA(leu) at position 3243 and spontaneous abortions in Japanese women attending a clinic for diabetic pregnancies. Diabetologia 38:809–815
Festa A, Krugluger W, Shnawa N, Hopmeier P, Haffner SM, Schernthaner G (1999) Trp64Arg polymorphism of the beta3-adrenergic receptor gene in pregnancy association with mild gestational diabetes mellitus. J Clin Endocrinol Metab 84:1695–1699
Rissanen J, Markkanen A, Karkkainen P et al. (2000) Sulfonylurea receptor 1 gene variants are associated with gestational diabetes and type 2 diabetes but not with altered secretion of insulin. Diabetes Care 23:70–73
Ober C, Xiang KS, Thisted RA, Indovina KA, Wason CJ, Dooley S (1989) Increased risk for gestational diabetes mellitus associated with insulin receptor and insulin-like growth factor II restriction fragment length polymorphisms. Genet Epidemiol 6:559–569
Allan CJ, Argyropoulos G, Bowker M et al. (1997) Gestational diabetes mellitus and gene mutations which affect insulin secretion. Diabetes Res Clin Pract 36:135–141
Alevizaki M, Thalassinou L, Grigorakis SI et al. (2000) Study of the Trp64Arg polymorphism of the beta3-adrenergic receptor in Greek women with gestational diabetes. Diabetes Care 23:1079–1083
Redondo MJ, Fain PR, Eisenbarth GS (2001) Genetics of type 1A diabetes. Recent Prog Horm Res 56:69–89
Freinkel N, Metzger BE, Phelps RL et al. (1985) Gestational diabetes mellitus. Heterogeneity of maternal age, weight, insulin secretion, HLA antigens, and islet cell antibodies and the impact of maternal metabolism on pancreatic B-cell and somatic development in the offspring. Diabetes 34 [Suppl 2]:1–7
Fuchtenbusch M, Ferber K, Standl E, Ziegler AG (1997) Prediction of type 1 diabetes postpartum in patients with gestational diabetes mellitus by combined islet cell autoantibody screening: a prospective multicenter study. Diabetes 46:1459–1467
Bennett ST, Todd JA (1996) Human type 1 diabetes and the insulin gene: principles of mapping polygenes. Annu Rev Genet 30:343–370
Ong KK, Phillips DI, Fall C et al. (1999) The insulin gene VNTR, type 2 diabetes and birth weight. Nat Genet 21:262–263 (Letter)
Waterworth DM, Bennett ST, Gharani N et al. (1997) Linkage and association of insulin gene VNTR regulatory polymorphism with polycystic ovary syndrome. Lancet 349:986–990
Bell GI, Selby MJ, Rutter WJ (1982) The highly polymorphic region near the human insulin gene is composed of simple tandemly repeating sequences. Nature 295:31–35
Vafiadis P, Bennett ST, Colle E, Grabs R, Goodyer CG, Polychronakos C (1996) Imprinted and genotype-specific expression of genes at the IDDM2 locus in pancreas and leucocytes. J Autoimmun 9:397–403
Pugliese A, Zeller M, Fernandez A Jr et al. (1997) The insulin gene is transcribed in the human thymus and transcription levels correlated with allelic variation at the INS VNTR-IDDM2 susceptibility locus for type 1 diabetes. Nat Genet 15:293–297
Altshuler D, Hirschhorn JN, Klannemark M et al. (2000) The common PPARgamma Pro12Ala polymorphism is associated with decreased risk of type 2 diabetes. Nat Genet 26:76–80 (Letter)
Van den Ouweland JM, Lemkes HH, Ruitenbeek W et al. (1992) Mutation in mitochondrial tRNA(Leu)(UUR) gene in a large pedigree with maternally transmitted type II diabetes mellitus and deafness. Nat Genet 1:368–371
Sjoroos M, Iitia A, Ilonen J, Reijonen H, Lovgren T (1995) Triple-label hybridization assay for type-1 diabetes-related HLA alleles. Biotechniques 18:870–877
Bennett ST, Lucassen AM, Gough SC et al. (1995) Susceptibility to human type 1 diabetes at IDDM2 is determined by tandem repeat variation at the insulin gene minisatellite locus. Nat Genet 9:284–292
Grubin CE, Daniels T, Toivola B et al. (1994) A novel radioligand binding assay to determine diagnostic accuracy of isoform-specific glutamic acid decarboxylase antibodies in childhood IDDM. Diabetologia 37:344–350
Verge CF, Stenger D, Bonifacio E et al. (1998) Combined use of autoantibodies (IA-2 autoantibody, GAD autoantibody, insulin autoantibody, cytoplasmic islet cell antibodies) in type 1 diabetes Combinatorial Islet Autoantibody Workshop. Diabetes 47:1857–1866
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28:412–419
Phillips DI, Clark PM, Hales CN, Osmond C (1994) Understanding oral glucose tolerance: comparison of glucose or insulin measurements during the oral glucose tolerance test with specific measurements of insulin resistance and insulin secretion. Diabet Med 11:286–292
Jensen CC, Cnop M, Hull RL, Fujimoto WY, Kahn SE, American Diabetes Association GENNID Study Group (2002) Beta-cell function is a major contributor to oral glucose tolerance in high-risk relatives of four ethnic groups in the U.S. Diabetes 51:2170–2178
Tuomilehto J, Zimmet P, Mackay IR et al. (1994) Antibodies to glutamic acid decarboxylase as predictors of insulin-dependent diabetes mellitus before clinical onset of disease. Lancet 343:1383–1385
Petersen JS, Dyrberg T, Damm P, Kuhl C, Molsted-Pedersen L, Buschard K (1996) GAD65 autoantibodies in women with gestational or insulin dependent diabetes mellitus diagnosed during pregnancy. Diabetologia 39:1329–1333
Mitchell ML, Hermos RJ, Larson CA, Palomaki GE, Haddow JE (2000) Prevalence of GAD autoantibodies in women with gestational diabetes: a retrospective analysis. Diabetes Care 23:1705–1706 (Letter)
Dozio N, Beretta A, Belloni C et al. (1997) Low prevalence of islet autoantibodies in patients with gestational diabetes mellitus. Diabetes Care 20:81–83
Fallucca F, Tiberti C, Torresi P et al. (1997) Autoimmune markers of diabetes in diabetic pregnancy. Ann Ist Super Sanita 33:425–428
Weng J, Ekelund M, Lehto M et al. (2002) Screening for MODY mutations, GAD antibodies, and type 1 diabetes-associated HLA genotypes in women with gestational diabetes mellitus. Diabetes Care 25:68–71
Walsh EC, Mather KA, Schaffner SF et al. (2003) An integrated haplotype map of the human major histocompatibility complex. Am J Hum Genet 73:580–590
Ferber KM, Keller E, Albert ED, Ziegler AG (1999) Predictive value of human leukocyte antigen class II typing for the development of islet autoantibodies and insulin-dependent diabetes postpartum in women with gestational diabetes. J Clin Endocrinol Metab 84:2342–2348
World Health Organization Ad Hoc Diabetes Reporting Group (1992) Diabetes and impaired glucose tolerance in women aged 20–39 years. World Health Stat Q 45:321–327
Kadiki OA, Gerryo SE, Khan MM (1988) Diabetes mellitus in Benghazi. J Trop Med Hyg 91:19–22
Eriksson J, Forsen B, Haggblom M, Teppo AM, Groop L (1992) Clinical and metabolic characteristics of type 1 and type 2 diabetes: an epidemiological study from the Narpes community in western Finland. Diabet Med 9:654–660
Deeb SS, Fajas L, Nemoto M et al. (1998) A Pro12Ala substitution in PPARgamma2 associated with decreased receptor activity, lower body mass index and improved insulin sensitivity. Nat Genet 20:284–287
Hara K, Okada T, Tobe K et al. (2000) The Pro12Ala polymorphism in PPAR gamma2 may confer resistance to type 2 diabetes. Biochem Biophys Res Commun 271:212–216
Litou H, Anastasiou E, Thalassinou L, Sarika HL, Philippou G, Alevizaki M (2002) Increased prevalence of VNTR III of the insulin gene in women with Gestational Diabetes Mellitus (GDM). Diabetologia 45 [Suppl. 2]:A132 (Abstract)
Acknowledgements
This work was supported by grants from the JDF Wallenberg Foundation (99JD-12812), the Swedish Medical Research Council (VR 72X-14064), EC grant (GIFT), the Novo Nordisk Foundation and grants to the Diabetes Prediction in Skåne (DiPiS) study. We thank the patients for their participation, and the DiPiS research group for helping with recruitment of some of the GDM and control women and for helping with HLA typing and GAD65 antibody analyses.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shaat, N., Ekelund, M., Lernmark, Å. et al. Genotypic and phenotypic differences between Arabian and Scandinavian women with gestational diabetes mellitus. Diabetologia 47, 878–884 (2004). https://doi.org/10.1007/s00125-004-1388-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-004-1388-5