Abstract
Purpose
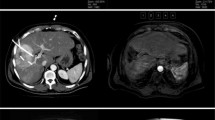
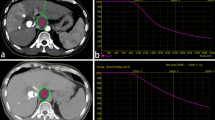
The purpose of the present study was to evaluate the clinical outcome of CT-guided high-dose-rate brachytherapy (CT-HDRBT) in patients with unresectable hepatocellular carcinoma (HCC).
Patients and methods
Over a 6-year period, 98 patients with 212 unresectable HCC underwent CT-HDRBT applying a 192Ir source at our institution. Magnetic resonance imaging (MRI) follow-up was performed 6 weeks after the intervention and then every 3 months. The primary endpoint was local tumor control (LTC); secondary endpoints included progression-free survival (PFS) and overall survival (OS).
Results
Patients were available for MRI evaluation for a mean follow-up of 23.1 months (range 4–64 months; median 20 months). Mean tumor diameter was 5 cm (range 1.8–12 cm). Eighteen of 212 (8.5 %) tumors showed local progression after a mean LTC of 21.1 months. In all, 67 patients (68.4 %) experienced distant tumor progression. The mean PFS was 15.2 months. Forty-six patients died during the follow-up period. Median OS was 29.2 months. Actuarial 1-, 2-, and 3-year OS rates were 80, 62, and 46 %, respectively.
Conclusion
CT-HDRBT is an effective therapy to attain local tumor control in patients with unresectable HCC. Prospective randomized studies comparing CT-HDRBT with the standard treatments like Radiofrequency ablation (RFA) and chemoembolization (TACE) are mandatory.
Zusammenfassung
Ziel
Zweck der vorliegenden Arbeit war die Analyse der klinischen Effektivität der CT-gesteuerten Hochdosis-Brachytherapie (CT-HDRBT) bei Patienten mit inoperablem hepatozellulären Karzinom (HCC).
Patienten und Methoden
Über einen Zeitraum von 6 Jahren, wurden an unserer Klinik 98 Patienten mit 212 inoperablen HCC mittels CT-HDRBT mit 192Ir behandelt. MRT-Verlaufskontrollen erfolgten 6 Wochen nach der Intervention und dann alle 3 Monate. Primärer Endpunkt der Studie war die lokale Tumorkontrolle (LTC); sekundäre Endpunkte waren das progressionsfreie Überleben (PFS) und Gesamtüberleben (OS).
Ergebnisse
Die mittlere Nachbeobachtungszeit betrug 23,1 Monate (Spanne 4–64 Monate, Median 20 Monate). Der mittlere Tumordurchmesser betrug 5 cm (Spanne 1,8–12 cm). Nach einer mittleren LTC von 21,1 Monaten zeigten 18 von 212 Tumoren (8,5 %) eine lokale Progression. Im weiteren Verlauf schritt die Tumorerkrankung bei 67 Patienten (68,4 %)in Form eines nichtlokalen Tumorprogress voran. Das mittlere PFS betrug 15,2 Monate. Während der Nachbeobachtungszeit verstarben 46 Patienten. Das mediane OS betrug 29,2 Monate. Die 1-Jahres-, 2-Jahres- und 3-Jahres-OS-Raten waren 80, 62 und 46 %.
Schlussfolgerung
Die CT-HDRBT ist eine effektive Therapie zur lokalen Kontrolle des Tumors bei Patienten mit inoperablem HCC. Vergleichende prospektive, randomisierte Studien gegenüber den Standardtherapien, wie Radiofrequenzablation (RFA) und Chemoembolisation (TACE) werden benötigt.





Similar content being viewed by others
References
Maluccio M, Covey A (2012) Recent progress in understanding, diagnosing, and treating hepatocellular carcinoma. CA Cancer J Clin 62:394–399
Bolondi L, Burroughs A, Dufour JF et al (2012) Heterogeneity of patients with intermediate (BCLC B) hepatocellular carcinoma: proposal for a subclassification to facilitate treatment decisions. Semin Liver Dis 32:348–359
Forner A, Llovet JM, Bruix J (2010) Hepatocellular carcinoma. Lancet 379:1245–1255
Crocetti L, de Baere T, Lencioni R (2010) Quality improvement guidelines for radiofrequency ablation of liver tumours. Cardiovasc Intervent Radiol 33:11–17
Llovet JM, Real MI, Montaña X et al (2002) Arterial embolisation or chemoembolisation versus symptomatic treatment in patients with unresectable hepatocellular carcinoma: a randomised controlled trial. Lancet 359:1734–1739
Lo CM, Ngan H, Tso WK et al (2002) Randomized controlled trial of transarterial lipiodol chemoembolization for unresectable hepatocellular carcinoma. Hepatology 35:1164–1171
Raoul JL, Sangro B, Forner A et al (2011) Evolving strategies for the management of intermediate-stage hepatocellular carcinoma: available evidence and expert opinion on the use of transarterial chemoembolization. Cancer Treat Rev 37:212–220
Ricke J, Wust P (2011) Computed tomography-guided brachytherapy for liver cancer. Semin Radiat Oncol 21:287–293
Ricke J, Wust P, Stohlmann A et al (2004) CT-guided interstitial brachytherapy of liver malignancies alone or in combination with thermal ablation: phase I-II results of a novel technique. Int J Radiat Oncol Biol Phys 58:1496–1505
Ricke J, Thormann M, Ludewig M et al (2010) MR-guided liver tumor ablation employing open high-field 1.0 T MRI for image-guided brachytherapy. Eur Radiol 20:1985–1993
Goldberg SN, Grassi CJ, Cardella JF; For the Society of Interventional Radiology Technology Assessment Committee and the International Working Group on Image-guided Tumor Ablation (2009) Image-guided tumor ablation: standardization of terminology and reporting criteria. J Vasc Interv Radiol 20:377–390
Gil-Alzugaray B, Chopitea A, Iňarrairaegui M et al (2013) Prognostic factors and prevention of radioembolization-induced liver disease. Hepatology 57:1078–1087
Llovet JM, Bruix J (2003) Systematic review of randomized trials for unresectable hepatocellular carcinoma: chemoembolization improves survival. Hepatology 37:429–442
Oliveri RS, Wetterslev J, Gluud C (2011) Transarterial (chemo)embolisation for unresectable hepatocellular carcinoma. Cochrane Database Syst Rev 16:CD004787
Salem R, Lewandowski RJ, Kulik L et al (2011) Radioembolization results in longer time-to-progression and reduced toxicity compared with chemoembolization in patients with hepatocellular carcinoma. Gastroenterology 140:497–507
Cárdenes HR (2009) Role of stereotactic body radiotherapy in the management of primary hepatocellular carcinoma. Rationale, technique and results. Clin Transl Oncol 11:276–283
Goodman KA, Wiegner EA, Maturen KE, Zhang Z et al (2010) Dose-escalation study of single-fraction stereotactic body radiotherapy for liver malignancies. Int J Radiat Oncol Biol Phys 78:486–493
Méndez Romero A, Wunderink W, Hussain SM et al (2006) Stereotactic body radiation therapy for primary and metastatic liver tumors: a single institution phase i-ii study. Acta Oncol 45:831–837
Lee SU, Park JW, Kim TH et al (2014) Effectiveness and safety of proton beam therapy for advanced hepatocellular carcinoma with portal vein tumor thrombosis. Strahlenther Onkol 190:806–814 [Epub ahead of print]
Wang PM, Hsu WC, Chung NN et al (2013) Radiotherapy with volumetric modulated arc therapy for hepatocellular carcinoma patients ineligible for surgery or ablative treatments. Strahlenther Onkol 189:301–307
Kim TH, Park JW, Kim YJ et al (2014) Simultaneous integrated boost-intensity modulated radiation therapy for inoperable hepatocellular carcinoma. Strahlenther Onkol 190:882–890 [Epub ahead of print]
Jereczek-Fossa BA, Bossi-Zanetti I, Mauro R et al (2013) CyberKnife robotic image-guided stereotactic radiotherapy for oligometastic cancer: a prospective evaluation of 95 patients/118 lesions. Strahlenther Onkol 189:448–455
Bujold A, Massey CA, Kim JJ et al (2013) Sequential phase I and II trials of stereotactic body radiotherapy for locally advanced hepatocellular carcinoma. J Clin Oncol 31:1631–1639
Ricke J, Wust P, Wieners G et al (2004) Liver malignancies: CT-guided interstitial brachytherapy in patients with unfavorable lesions for thermal ablation. J Vasc Interv Radiol 15:1279–1286
Tselis N, Chatzikonstantinou G, Kolotas C et al (2012) Hypofractionated accelerated computed tomography-guided interstitial high-dose-rate brachytherapy for liver malignancies. Brachytherapy 11:507–514
Collettini F, Schnapauff D, Poellinger A et al (2012) Hepatocellular carcinoma: computed-tomography-guided high-dose-rate brachytherapy (CT-HDRBT) ablation of large (5–7 cm) and very large (> 7 cm) tumours. Eur Radiol 22:1101–1109
Jung J, Yoon SM, Kim SY et al (2013) Radiation-induced liver disease after stereotactic body radiotherapy for small hepatocellular carcinoma: clinical and dose-volumetric parameters. Radiat Oncol 8:249
Mohnike K, Wieners G, Schwartz F et al (2010) Computed tomography-guided high-dose-rate brachytherapy in hepatocellular carcinoma: safety, efficacy, and effect on survival. Int J Radiat Oncol Biol Phys 78:172–179
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
F. Collettini, N. Schreiber, D. Schnapauff, T. Denecke, P. Wust, E. Schott, B. Hamm, and B. Gebauerstate that there are no conflicts of interest.
All studies on humans described in the present manuscript were carried out with the approval of the responsible ethics committee and in accordance with national law and the Helsinki Declaration of 1975 (in its current, revised form). Informed consent was obtained from all patients included in studies.
Rights and permissions
About this article
Cite this article
Collettini, F., Schreiber, N., Schnapauff, D. et al. CT-guided high-dose-rate brachytherapy of unresectable hepatocellular carcinoma. Strahlenther Onkol 191, 405–412 (2015). https://doi.org/10.1007/s00066-014-0781-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-014-0781-3