Abstract
Background
Galectin-3 (gal-3) is an emerging prognostic biomarker in heart failure (HF). Clinical and experimental studies suggest that gal-3 is an important mediator of HF. Here we aimed to examine the relationship between gal-3 and diastolic dysfunction in patients undergoing maintenance hemodialysis (HD).
Methods
We examined the relationship between plasma gal-3 levels and left ventricular diastolic function. Plasma gal-3 was measured in 87 subjects with chronic HD and in 45 healthy controls using biochemical evaluations. Conventional echocardiography and pulsed tissue Doppler assessment were performed in all patients. Left ventricular diastolic dysfunction (LVDD) was defined as E’ < 8 cm/s. The E/E’ ratio was used as the main determinant of LVDD grade.
Results
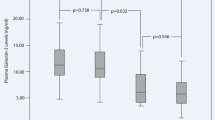
The mean gal-3 concentrations were: 16.05 ng/ml (13.89–19.75) in healthy controls; 14.54 ng/ml (10.85–17.65) in HD patients with normal diastolic function; and 23.30 ng/ml (20.12–26.87) in HD patients with LVDD (p < 0.01). Plasma gal-3 levels correlated with E/E’ (r = 0.933, p < 0.01), left atrial volume index (r = 0.713, p < 0.01), and E’ (r = -0.685, p < 0.01). ROC analysis showed that the best gal-3 cut-off point for the diagnosis of LVDD was 20.12 ng/ml with a sensitivity of 67.6 % and specificity of 84.6 % (AUC = 0.803).
Conclusion
We suggest that gal-3 may be a promising biomarker for the detection of LVDD in HD patients.
Zusammenfassung
Hintergrund
Galectin-3 (gal-3) stellt einen prognostischen Biomarker mit zunehmender Bedeutung bei Herzinsuffizienz dar. Klinischen und experimentellen Studien zufolge ist gal-3 wohl ein entscheidender Mediator der Herzinsuffizienz. In der vorliegenden Studie bestand das Ziel darin, den Zusammenhang zwischen gal-3 und diastolischer Dysfunktion bei Patienten unter Erhaltungshämodialyse (HD) zu untersuchen.
Methoden
Die Autoren untersuchten die Beziehung zwischen gal-3-Spiegeln im Plasma und linksventrikulärer Funktion. gal-3 im Plasma wurde bei 87 Teilnehmern mit chronischer HD und 45 gesunden Kontrollen anhand biochemischer Untersuchungen gemessen. Eine konventionelle Echokardiographie und die Untersuchung mit gepulstem Gewebsdoppler erfolgten bei sämtlichen Patienten. Eine linksventrikuläre diastolische Dysfunktion (LVDD) wurde definiert als E’ < 8 cm⁄s. Die E/E’-Ratio stellte das Hauptkriterium für den Grad der LVDD dar.
Ergebnisse
Die durchschnittliche gal-3-Konzentration betrug 16,05 ng/ml (13,89–19,75) bei den gesunden Kontrollen; 14,54 ng/ml (10,85–17,65) bei HD-Patienten mit normaler diastolischer Funktion und 23,30 ng/ml (20,12–26,87) bei HD-Patienten mit LVDD (p < 0,01). Die Plasma-gal-3-Spiegel korrelierten mit E/E’ (r = 0,933; p < 0,01), LAVI (r = 0,713; p < 0,01) und E’ (r = -0,685; p < 0,01). Die ROC-Analyse zeigte, dass der beste gal-3-Grenzwert für die Diagnose einer LVDD bei 20,12 ng/ml lag – mit einer Sensitivität von 67,6 % und einer Spezifität von 84,6 % (AUC: 0,803).
Schlussfolgerung
Die Autoren schätzen gal-3 als vielversprechenden Biomarker zur Erkennung einer LVDD bei HD-Patienten ein.








Similar content being viewed by others
References
Collins AJ, Foley RN, Herzog C et al (2010) Excerpts from the US Renal Data System 2009 Annual Data Report. U.S. Department of Health and Human Services The National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases United States Renal Data System. Am J Kidney Dis 55(Suppl 1):1–420, A6–7
Foley RN, Parfrey PS, Harnett JD et al (1995) Clinical and echocardiographic disease in patients starting end-stage renal disease therapy. Kidney Int 47:186–192
Paoletti E (2012) Left ventricular hypertrophy and progression of chronic kidney disease. J Nephrol 25(6):847–850
Pecoits-Filho R, Barberato SH (2010) Echocardiography in chronic kidney disease: diagnostic and prognostic implications. Nephron Clin Pract 114:c242–c247
Kunz K, Dimitrov Y, Muller S et al (1998) Uraemic cardiomyopathy. Nephrol Dial Transplant 13(Suppl 4):39–43
Ahmed A, Rich MW, Sanders PW et al (2007) Chronic kidney disease associated mortality in diastolic versus systolic heart failure: a propensity matched study. Am J Cardiol 99:393–398
Pecoits-Filho R, Bucharles S, Barberato SH (2012) Diastolic heart failure in dialysis patients: mechanisms, diagnostic approach, and treatment. Semin Dial 25(1):35–41
Redfield MM, Jacobsen SJ, Burnett JC Jr, Mahoney DW, Bailey KR, Rodeheffer RJ (2003) Burden of systolic and diastolic ventricular dysfunction in the community: appreciating the scope of the heart failure epidemic. JAMA 289:194–202
Halley CM, Houghtaling PL, Khalil MK et al (2011) Mortality rate in patients with diastolic dysfunction and normal systolic function. Arch Intern Med 171:1082–1087
Kim MK, Kim B, Lee JY, Kim JS, Han BG, Choi SO, Yang JW (2013) Tissue doppler-derived E/eʼ ratio as a parameter for assessing diastolic heart failure and as a predictor of mortality in patients with chronic kidney disease. Korean J Intern Med 28(1):35–44
Farshid A, Pathak R, Shadbolt B, Arnolda L, Talaulikar G (2013) Diastolic function is a strong predictor of mortality in patients with chronic kidney disease. BMC Nephrol 14:280
Satpathy C, Mishra TK, Satpathy R, Satpathy HK, Barone E (2006) Diagnosis and management of diastolic dysfunction and heart failure. Am Fam Physician 73(5):841–846
Henderson NC, Sethi T (2009) The regulation of inflammation by galectin-3. Immunol Rev 230(1):160–171
Sharma UC, Pokharel S, van Brakel TJ, van Berlo JH, Cleutjens JPM, Schroen B et al (2004) Galectin-3 marks activated macrophages in failure-prone hypertrophied hearts and contributes to cardiac dysfunction. Circulation 110:3121–3128
Yu L, Ruifrok WP, Meissner M, Bos EM, van Goor H, Sanjabi B et al (2013) Genetic and pharmacological inhibition of galectin-3 prevents cardiac remodeling by interfering with myocardial fibrogenesis. Circ Heart Fail 6(1):107–117
van Kimmenade RR, Januzzi JL Jr, Ellinor PT, Sharma UC, Bakker JA, Low AF, Martinez A, Crijns HJ, MacRae CA, Menheere PP, Pinto YM (2006) Utility of amino-terminal pro-brain natriuretic peptide, galectin-3, and apelin for the evaluation of patients with acute heart failure. J Am Coll Cardiol 48:1217–1224
Shah RV, Chen-Tournoux AA, Picard MH, van Kimmenade RR, Januzzi JL (2010) Galectin-3, cardiac structure and function, and long-term mortality in patients with acutely decompensated heart failure. Eur J Heart Fail 12:826–832
Lok DJA, van Der Meer P, de la Porte PWB-A, Lipsic E, Wijngaarden JV, Hillege HL, van Veldhuisen DJ (2010) Prognostic value of galectin-3, a novel biomarker of fibrosis, in patients with chronic heart failure: data from the DEAL-HF study. Clin Res Cardiol 99:323–328
de Boer RA, Lok DJA, Jaarsma T, van Der Meer P, Voors AA, Hillege HL, van Veldhuisen DJ (2011) Predictive value of plasma galectin-3 levels in heart failure with reduced and preserved ejection fraction. Ann Med 43:60–68
Gullestad L, Ueland T, Kjekshus J, Nymo SH, Hulthe J, Muntendam P, McMurray JJ, Wikstrand J, Aukrust P (2012) The predictive value of galectin-3 for mortality and cardiovascular events in the Controlled Rosuvastatin Multinational Trial in Heart Failure (CORONA). Am Heart J 164:878–883
Yilmaz H, Gurel OM, Celik HT, Bozkurt A, Yildirim ME, Bilgic I, Bilgic MA, Bavbek N, Akcay A (2014) Relationship of galectin-3 to left ventricular geometry and hypertrophy in chronic hemodialysis patients. Herz doi:10.1007/s00059-014-4111-4
Nagueh S, Appleton C, Gillebert T, Marino P, Oh J, Smiseth O et al (2009) Recommendations for the evaluation of left ventricular diastolic function by echocardiography. J Am Soc Echocardiogr 22:107–133
Krumholz HM, Larson M, Levy D (1995) Prognosis of left ventricular geometric patterns in the Framingham study. J Am Coll Cardiol 25:879–884
Lang RM, Bierig M, Devereux RB et al (2005) Recommendations for chamber quantification: a report from the American Society of Echocardiography’s guidelines and standards committee and the chamber quantification writing group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr 18:1440–1463
Alnabhan N, Kerut EK, Geraci SA, McMullan MR, Fox E (2008) An approach to analysis of left ventricular diastolic function and loading conditions in the echocardiography laboratory. Echocardiography 25(1):105–116
Christenson RH, Duh SH, Wu AH et al (2010) Multi-center determination of galectin-3 assay performance characteristics: anatomy of a novel assay for use in heart failure. Clin Biochem 43(7–8):683–690
van der Velde AR, Gullestad L, Ueland T, Aukrust P, Guo Y, Adourian AS, Muntendam P, van Veldhuisen DJ, de Boer RA (2013) Prognostic value of changes in galectin-3 levels over time in patients with heart failure: data from CORONA and COACH. Circ Heart Fail 6:219–226
Januzzi JL Jr, Camargo CA, Anwaruddin S, Baggish AL, Chen AA, Krauser DG, Tung R, Cameron R, Nagurney JT, Chae CU, Lloyd-Jones DM, Brown DF, Foran-Melanson S, Sluss PM, Lee-Lewandrowski E, Lewandrowski KB (2005) The N-Terminal Pro-BNP Investigation of Dyspnea in the Emergency Department (PRIDE) study. Am J Cardiol 95:948–954
Moya-Mur JL, Garcia-Martin A, Garcia-LIedo A, Ruiz-Leria S, Jimenez-Nacher JJ, Megias-Sanz A, Taboada D, Muriel A (2010) Indexed left atrial volume is a more sensitive indicator of filling pressures and left heart function than is anteroposterior left atrial diameter. Echocardiography 27(9):1049–1055
Patel DA, Lavie CJ, Milani RV, Ventura HO (2011) Left atrial volume index predictive of mortality independent of left ventricular geometry in a large clinical cohort with preserved ejection fraction. Mayo Clin Proc 86(8):730–737
Shizuku J, Yamashita T, Ohba T, Kabaya T, Nitta K (2012) Left atrial volume is an independent predictor of all-cause mortality in chronic hemodialysis patients. Intern Med 51(12):1479–1485
Moller JE, Hillis GS, Oh JK, Seward JB, Reeder GS, Wright RS, Park SW, Bailey KR, Pellika PA (2003) Left atrial volume: a powerful predictor of survival after acute myocardial infarction. Circulation 107:2207–2212
Barnes ME, Miyasaka Y, Seward JB et al (2004) Left atrial volume in the prediction of first ischemic stroke in an elderly cohort without atrial fibrillation. Mayo Clin Proc 79:1008–1014
Okada K, Mikami T, Kaga S, Onozuka H, Inoue M, Yokoyama S, Nishino H, Nishida M, Matsuno K, Iwano H, Yamada S, Tsutsui H (2011) Early diastolic mitral annular velocity at the interventricular septal annulus correctly reflects left ventricular longitudinal myocardial relaxation. Eur J Echocardiogr 12(12):917–923
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
O.M. Gurel, H. Yilmaz, T.H. Celik, M. Cakmar, M. Namaslu, A.M. Bilgiç, N. Bavbek, A. Akcay, and B. Eryonucu state that there are no conflicts of interest.
Rights and permissions
About this article
Cite this article
Gurel, O., Yilmaz, H., Celik, T. et al. Galectin-3 as a new biomarker of diastolic dysfunction in hemodialysis patients. Herz 40, 788–794 (2015). https://doi.org/10.1007/s00059-015-4303-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00059-015-4303-6