Abstract
Objectives
To test the association of low-grade inflammation with socioeconomic status (SES) and determine the relative contribution of prevalent chronic diseases and health-related behaviours in explaining such association.
Methods
Cross-sectional analysis on 19,867 subjects (age ≥35, 48.1% men) recruited within the Moli-sani study from 2005 to 2010 (Italy). A score of low-grade inflammation, including platelet and leukocyte counts, the granulocyte-to-lymphocyte ratio, and C-reactive protein was applied. SES was measured by education, household income, and occupational social class.
Results
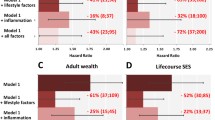
Low SES was associated with elevated levels of low-grade inflammation. Health behaviours (including adiposity, smoking, physical activity, and Mediterranean diet adherence) explained 53.5, 53.9, and 84.9% of the association between social class, income, and education with low-grade inflammation, respectively. Adiposity and body mass index showed a prominent role, while prevalent chronic diseases and conditions only marginally attenuated SES inequalities in inflammation.
Conclusions
Low-grade inflammation was socioeconomically patterned in a large Mediterranean population. Potentially modifiable behavioural factors explained the greatest part of this association with a leading contribution of adiposity, body mass index, and physical activity.

Similar content being viewed by others
References
Ambring A, Johansson M, Axelsen M, Gan L, Strandvik B, Friberg P (2006) Mediterranean-inspired diet lowers the ratio of serum phospholipid n-6 to n-3 fatty acids, the number of leukocytes and platelets, and vascular endothelial growth factor in healthy subjects. Am J Clin Nutr 83:575–581
Barbaresko J, Koch M, Schulze MB, Nöthlings U (2013) Dietary pattern analysis and biomarkers of low-grade inflammation: a systematic literature review. Nutr Rev 71:511–527
Bonaccio M, Di Castelnuovo A, De Curtis A, Costanzo S, Persichillo M, Donati MB et al (2014) Adherence to the Mediterranean diet is associated with lower platelet and leukocyte counts: results from the MOLI-SANI study. Blood 123:3037–3044
Bonaccio M, Di Castelnuovo A, Costanzo S, Persichillo M, Donati MB, de Gaetano G et al (2016) Interaction between education and income on the risk of all-cause mortality: prospective results from the MOLI-SANI study. Int J Public Health 61:765–776
Casas R, Sacanella E, Urpí-Sardà M, Chiva-Blanch G, Ros E, Martínez-González MA et al (2014) The effects of the Mediterranean diet on biomarkers of vascular wall inflammation and plaque vulnerability in subjects with high risk for cardiovascular disease. a randomized trial. PLoS One 9(6):e100084
Centritto F, Iacoviello L, di Giuseppe R, De Curtis A, Costanzo S, Zito F et al (2009) Dietary patterns, cardiovascular risk factors and C-reactive protein in a healthy Italian population. Nutr Metab Cardiovasc Dis 19:697–706
Coussens LM, Werb Z (2002) Inflammation and cancer. Nature 420:860–867
Danesh J, Collins R, Appleby P, Peto R (1998) Association of fibrinogen, C-reactive protein, albumin, or leukocyte count with coronary heart disease: meta-analyses of prospective studies. JAMA 279:1477–1482
Danesh J, Whincup P, Walker M, Lennon L, Thomson A, Appleby P et al (2000) Low-grade inflammation and coronary heart disease: prospective study and updated meta-analyses. BMJ 321:199–204
Deverts DJ, Cohen S, Kalra P, Matthews KA (2012) The prospective association of socioeconomic status with C-reactive protein levels in the CARDIA study. Brain Behav Immun 26:1128–1135
Di Castelnuovo A, Costanzo S, Persichillo M, Olivieri M, de Curtis A, Zito F et al (2012) Distribution of short and lifetime risks for cardiovascular disease in Italians. Eur J. Prev Cardiol 19:723–730
Donati MB (2010) The “common soil hypothesis”: evidence from population studies? Thromb Res 125(Suppl 2):S92–S95
Drewnowski A (2009) Obesity, diets, and social inequalities. Nutr Rev 67(Suppl 1):S36–S39
Empana JP, Sykes DH, Luc G, Juhan-Vague I, Arveiler D, Ferrieres J et al (2005) Contributions of depressive mood and circulating inflammatory markers to coronary heart disease in healthy European men: the Prospective Epidemiological Study of Myocardial Infarction (PRIME). Circulation 111:2299–2305
Federico B, Mackenbach JP, Eikemo TA, Sebastiani G, Marinacci C, Costa G et al (2013) Educational inequalities in mortality in northern, mid and southern Italy and the contribution of smoking. J Epidemiol Community Health 67:603–609
Fraga S, Marques-Vidal P, Vollenweider P, Waeber G, Guessous I, Paccaud F et al (2015) Association of socioeconomic status with inflammatory markers: a two cohort comparison. Prev Med 71:12–19
Jousilahti P, Salomaa V, Rasi V, Vahtera E, Palosuo T (2003) Association of markers of systemic inflammation, C reactive protein, serum amyloid A, and fibrinogen, with socioeconomic status. J Epidemiol Community Health 57:730–733
Kaplan GA, Keil JE (1993) Socioeconomic factors and cardiovascular disease: a review of the literature. Circulation 88:1973–1998
Kershaw KN, Mezuk B, Abdou CM, Rafferty JA, Jackson JS (2010) Socioeconomic position, health behaviors, and C-reactive protein: a moderated-mediation analysis. Health Psychol 29:307–316
Khang YH, Lynch JW, Yang S, Harper S, Yun SC, Jung-Choi K et al (2009) The contribution of material, psychosocial, and behavioural factors in explaining educational and occupational mortality inequalities in a nationally representative sample of South Koreans: relative and absolute perspectives. Soc Sci Med 68:858–866
Koster A, Bosma H, Penninx BW, Newman AB, Harris TB, van Eijk JT et al (2006) Association of inflammatory markers with socioeconomic status. J Gerontol A Biol Sci Med Sci 61:284–290
Lind L (2003) Circulating markers of inflammation and atherosclerosis. Atherosclerosis 169:203–214
Mackenbach JP, Stirbu I, Roskam AJ, Schaap MM, Menvielle G, Leinsalu M et al (2008) Socioeconomic inequalities in health in 22 European countries. N Engl J Med 358:2468–2481
Mathur N, Pedersen BK (2008) Exercise as a mean to control low-grade systemic inflammation. Mediat Inflamm 2008:109502. doi:10.1155/2008/109502
McFadden E, Luben R, Wareham N, Bingham S, Khaw KT (2008) Occupational social class, educational level, smoking and body mass index, and cause-specific mortality in men and women: a prospective study in the European Prospective Investigation of Cancer and Nutrition in Norfolk (EPIC-Norfolk) cohort. Eur J Epidemiol 23:511–522
Mendall MA, Strachan DP, Butland BK, Ballam L, Morris J, Sweetnam PM et al (2000) C-reactive protein: relation to total mortality, cardiovascular mortality and cardiovascular risk factors in men. Eur Heart J 21:1584–1590
O’Connor MF, Irwin MR (2010) Links between behavioral factors and inflammation. Clin Pharmacol Ther 87:479–482
Pampel FC, Krueger PM, Denney JT (2010) Socioeconomic disparities in health behaviors. Annu Rev Sociol 36:349–370
Panagiotakos DB, Pitsavos CE, Chrysohoou CA, Skoumas J, Toutouza M, Belegrinos D et al (2004) The association between educational status and risk factors related to cardiovascular disease in healthy individuals: the ATTICA study. Ann Epidemiol 14:188–194
Pisani P, Faggiano F, Krogh V, Palli D, Vineis P, Berrino F (1997) Relative validity and reproducibility of a food frequency dietary questionnaire for use in the Italian EPIC centres. Int J Epidemiol 26(Suppl 1):S152–S160
Pounis G, Bonaccio M, Di Castelnuovo A, Costanzo S, de Curtis A, Persichillo M et al (2016) Polyphenol intake is associated with low-grade inflammation, using a novel data analysis from the Moli-sani study. Thromb Haemost 115:344–352
Ranjit N, Diez-Roux AV, Shea S, Cushman M, Ni H, Seeman T (2007) Socioeconomic position, race/ethnicity, and inflammation in the multi-ethnic study of atherosclerosis. Circulation 116:2383–2390
Samuels MA (2004) Inflammation and neurological disease. Curr Opin Neurol 17:307–309
Santimone I, Di Castelnuovo A, De Curtis A, Spinelli M, Cugino D, Gianfagna F et al (2011) White blood cell count, sex and age are major determinants of heterogeneity of platelet indices in an adult general population: results from the MOLI-SANI project. Haematologica 96:1180–1188
Schnabel RB, Yin X, Larson MG, Yamamoto JF, Fontes JD, Kathiresan S et al (2013) Multiple inflammatory biomarkers in relation to cardiovascular events and mortality in the community. Arterioscler Thromb Vasc Bio 33:1728–1733
Stringhini S, Batty GD, Bovet P, Shipley MJ, Marmot MG, Kumari M et al (2013) Association of lifecourse socioeconomic status with chronic inflammation and type 2 diabetes risk: the Whitehall II Prospective Cohort Study. PLoS Med 10:e1001479
Stringhini S, Polidoro S, Sacerdote C, Kelly RS, van Veldhoven K, Agnoli C et al (2015) Life-course socioeconomic status and DNA methylation of genes regulating inflammation. Int J Epidemiol 44:1320–1330
Trichopoulou A, Costacou T, Bamia C, Trichopoulos D (2003) Adherence to a Mediterranean diet and survival in a Greek population. N Engl J Med 348:2599–60819
Vilahur G, Badimon L (2013) Antiplatelet properties of natural products. Vascul Pharmacol 59:67–75
WHO Expert Consultation (2008) Waist circumference and waist-hip ratio. Geneva, 8–11 December. http://apps.who.int/iris/bitstream/10665/44583/1/9789241501491_eng.pdf. Accessed on June 2016
Acknowledgements
The Moli-sani research group thanks the Associazione Cuore Sano Onlus (Campobasso, Italy) for its financial and cultural support.
Moli-sani Study Investigators: The enrolment phase of the Moli-sani Project was conducted at the Research Laboratories of the Catholic University in Campobasso (Italy), the follow-up of the Moli-sani cohort is being conducted at the IRCCS Neuromed, Pozzilli, Italy.
Steering Committee: Licia Iacoviello (Neuromed, Pozzilli, Italy), Chairperson, Maria Benedetta Donati, and Giovanni de Gaetano (Neuromed, Pozzilli, Italy).
Safety and data monitoring Committee: Jos Vermylen (Catholic Univesity, Leuven, Belgio), Chairman, Ignacio De Paula Carrasco (Accademia Pontificia Pro Vita, Rome, Italy), Simona Giampaoli (Istituto Superiore di Sanità, Roma, Italy), Antonio Spagnuolo (Catholic University, Rome, Italy).
Event adjudicating Committee: Deodato Assanelli (Brescia, Italy), Vincenzo Centritto (Campobasso, Italy), Pasquale Spagnuolo, and Dante Staniscia (Termoli, Italy).
Scientific and organizing secretariat: Francesco Zito (Coordinator), Americo Bonanni, Chiara Cerletti, Amalia De Curtis, Augusto Di Castelnuovo, Licia Iacoviello, Roberto Lorenzet, Antonio Mascioli, Marco Olivieri, and Domenico Rotilio.
Data management and analysis: Augusto Di Castelnuovo (Coordinator), Marialaura Bonaccio, Simona Costanzo, and Francesco Gianfagna.
Informatics: Marco Olivieri (Coordinator), Maurizio Giacci, Antonella Padulo, and Dario Petraroia.
Biobank and biomedical analyses: Amalia De Curtis (Coordinator), Sara Magnacca, Federico Marracino, Maria Spinelli, and Christian Silvestri.
Communication and Press Office: Americo Bonanni (Coordinator), Marialaura Bonaccio, and Francesca De Lucia.
Moli-family Project: Francesco Gianfagna, Branislav Vohnout.
Recruitment staff: Franco Zito (General Coordinator), Secretariat: Mariarosaria Persichillo (Coordinator), Angelita Verna, Maura Di Lillo, Irene Di Stefano, Blood sample: Agnieszka Pampuch; Branislav Vohnout, Agostino Pannichella, Antonio Rinaldo Vizzarri, Spirometry: Antonella Arcari (Coordinator), Daniela Barbato, Francesca Bracone, Simona Costanzo, Carmine Di Giorgio, Sara Magnacca, Simona Panebianco, Antonello Chiovitti, Federico Marracino, Sergio Caccamo, Vanesa Caruso; Electrocardiograms : Livia Rago (Coordinator), Daniela Cugino, Francesco Zito, Francesco Gianfagna, Alessandra Ferri, Concetta Castaldi, Marcella Mignogna; Tomasz Guszcz, Questionnaires: Romina di Giuseppe (Coordinator), Paola Barisciano, Lorena Buonaccorsi, Floriana Centritto, Antonella Cutrone, Francesca De Lucia, Francesca Fanelli, Iolanda Santimone, Anna Sciarretta, Maura Di Lillo, Isabella Sorella, Irene Di Stefano, Emanuela Plescia, Alessandra Molinaro, and Christiana Cavone.
Call Center: Giovanna Galuppo, Maura Di Lillo, Concetta Castaldi, Dolores D’Angelo, and Rosanna Ramacciato.
Follow-up: Simona Costanzo (Coordinator); Data management: Simona Costanzo, and Marco Olivieri; Event adjudication: Livia Rago (Coordinator), Simona Costanzo, Amalia de Curtis, Licia Iacoviello, and Mariarosaria Persichillo.
Regional Health Institutions: Azienda Sanitaria Regionale del Molise (ASReM, Campobasso, Italy), UOC Servizio Igiene e Sanità Pubblica - Dipartimento di Prevenzione; Offices of vital statistics of the Molise region and Molise Dati Spa (Campobasso, Italy).
Hospitals: Presidi Ospedalieri ASReM (Presidio Ospedaliero A. Cardarelli—Campobasso, Ospedale F. Veneziale—Isernia, Ospedale San Timoteo—Termoli (CB), Ospedale Ss. Rosario—Venafro (IS), Ospedale Vietri—Larino (CB), Ospedale San Francesco Caracciolo—Agnone (IS); Istituto di cura Villa Maria—Campobasso; Fondazione di Ricerca e Cura Giovanni Paolo II—Campobasso; IRCCS Neuromed—Pozzilli (IS).
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
The enrolment phase of the Moli-sani Study (2005–2010) was performed at the Research Laboratories, Catholic University of Campobasso, Italy, and was supported by research grants from Pfizer Foundation (Rome, Italy), the Italian Ministry of University and Research (MIUR, Rome, Italy)—Programma Triennale di Ricerca, Decreto no.1588 and Instrumentation Laboratory, Milan, Italy. Marialaura Bonaccio is presently supported by a Fondazione Umberto Veronesi Fellowship. The analyses reported here were partially supported by the Italian Ministry of Health [Grant number GR-2013-02356060]. Funders had no role in study design, collection, analysis, and interpretation of data; in the writing of the manuscript and in the decision to submit the article for publication. All authors were and are independent from funders.
Ethical approval
All procedures performed in the present study, involving human participants, were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Written informed consent was obtained from all individual participants included in the study.
Additional information
Moli-sani study Investigators are listed in Acknowledgements.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Bonaccio, M., Di Castelnuovo, A., Pounis, G. et al. Relative contribution of health-related behaviours and chronic diseases to the socioeconomic patterning of low-grade inflammation. Int J Public Health 62, 551–562 (2017). https://doi.org/10.1007/s00038-016-0939-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00038-016-0939-0