Abstract
Among the complex network of inflammatory cells involved in the pathogenesis of rheumatoid arthritis (RA), Th17 cells have recently been identified as key cells in the promotion of autoimmune processes, and joint destruction. The IL-23/Th17 signalling pathway, consisting of IL-23/IL-23R, IL-17A and IL-17F encoding genes, represents a candidate way for RA development with possible involvement in disease susceptibility and effect on disease progression. The present study aimed to determine the association between the polymorphic variants of the IL-17A (rs2275913), IL-17F (rs763780) and IL-23R (rs11209026) genes and RA susceptibility, progression and response to therapy with TNF-α inhibitors. Eighty-nine patients and 125 healthy individuals were investigated. The IL-17A polymorphism was found to affect RA progression and response to anti-TNF treatment. Female patients carrying the IL-17A wild-type genotype more frequently presented with stage 4 (8/24 vs. 6/47; p = 0.058) and were characterized by more active disease (the highest DAS28 score >5.1) after 3 months of therapy with the TNF inhibitors (12/23 vs. 15/45; p = 0.040). The IL-17F polymorphism appeared to be associated with susceptibility to the disease. The presence of the IL-17F minor variant (OR 3.97; p < 0.001) and its homozygosity (OR 29.62; p < 0.001) was more frequent among patients than healthy individuals. These results suggest that the polymorphisms within the IL-17A and IL-17F genes play a significant role in RA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rheumatoid arthritis (RA) is a chronic autoimmune disorder characterized by systemic inflammation and persistent synovitis that affects the joints and promotes joint destruction (Lee and Weinblatt 2001). Among the complex network of inflammatory cells involved in the pathogenesis of RA, Th17 cells have recently been identified as key cells in the promotion of autoimmune processes, joint destruction and angiogenesis (Annunziato et al. 2009). Th17 cells and their cytokines are associated with several autoimmune and inflammatory diseases, such as RA, systemic lupus erythematosus, multiple sclerosis (MS), psoriasis, inflammatory bowel disease (IBD) and allergy and asthma (Miossec et al. 2009; Wilke et al. 2011). The hallmark of the Th17 subset is the production of interleukin IL-17A and IL-17F, which share strong homology, and surface expression of the IL-23 receptor (IL-23R) (Hot et al. 2011). Therefore, IL-17A, IL-17F and IL-23 may play an important role in T cell-triggered inflammation by upregulating some of the gene products involved in cell activation, proliferation and growth, and it is an important inductor of various cytokines and chemokines that are crucial in regulating the inflammatory response. IL-23 plays a key role in the development of pathogenic Th17 cells that produce the cytokine IL-17, which induces the production of several pro-inflammatory cytokines, such as TNF-α and IL-6, chemokines, and some other additional novel factors responsible for RA and other autoimmune diseases (Bettelli et al. 2008; Langrish et al. 2005). IL-23 is an essential promoter of chronic joint inflammation and mediates proinflammatory activity, in part, via production of IL-17 through Th17 lymphocyte activation (Aggarwal et al. 2003; McKenzie et al. 2006). Interestingly, in RA, IL-23 levels correlate with IL-17 levels in the joint fluid and with IL-17 and TNF-α levels in the serum (Wendling 2008). In addition, the serum level of IL-23 in patients with RA is correlated with the number of swollen joints, the Disease Activity Scores of 28 (DAS28) joints, and the serum level of IL-17. IL-17 has also been found in the synovial membrane and synovial fluid of RA patients (Kotake et al. 1999; Li et al. 2013).
Thus, the IL-23/Th17 signalling pathway, consisting of IL-23/IL-23R, IL-17A and IL-17F encoding genes, represents a candidate way for RA development with possible involvement in disease susceptibility and effect on disease progression (Iwakura and Ishigame 2006; Lubberts 2010).
Thus in the present study the associations between genetic variants within the IL-23/Th17 signalling pathway were analysed. We aimed to assess the significance of three biallelic polymorphisms: IL-17A (rs2275913; G-197A), IL-17F (rs763780; A7488G; His161Arg) and IL-23R (rs11209026, G1142A; Arg381Gln) for RA susceptibility, progression of the disease and response to therapy with TNF-α inhibitors.
Materials and Methods
Patients and Controls
For the study 89 patients (female/male: 72/17) diagnosed with RA and hospitalized at the Rheumatology Clinic of the Medical University in Wroclaw, Poland were included. The following inclusion criteria were accepted: consent to participate in the study; confirmed RA based on criteria of the American College of Rheumatology; active form of the disease: DAS28 > 5.1; age over 18 years; women and men with reproductive potential had to use reliable contraception; taking nonsteroidal anti-inflammatory drugs and glucocorticosteroids in stable doses was allowed.
There were the following exclusion criteria: pregnancy or breastfeeding; coexistence of other systemic diseases of connective tissue besides RA; clinically significant impairment of hepatic and renal function; alcohol abuse; infection with hepatotropic viruses; infections resistant to therapy; ongoing history of cancer if no cure was achieved; uncontrolled diabetes; patient unwilling or unable to cooperate.
Patients who had been treated with recommended doses of TNF-α inhibitors (adalimumab, etanercept, infliximab, certolizumab) for at least 3 months or had stopped therapy because of adverse events were investigated. To examine the response to anti-TNF therapy in RA, blood samples, laboratory data and clinical data were collected at baseline (prior to anti-TNF therapy) and 3 months after treatment. Clinical evaluation was based on medical history, number of painful and swollen joints, pain intensity assessed by the patient on a 100-mm visual analogue scale and laboratory tests (ESR, CRP). The parameters allowed determination of improvement according to the criteria based on DAS28 suggested by the European League Against Rheumatism.
All the patients provided written informed consent. The study was approved by the Wroclaw Medical University Ethics Committee. For patient characteristics see Table 1.
Stages of RA were assessed according to Wheeless (2012). According to this classification the first stage RA is characterized by synovitis, or an inflammation of the synovial membrane, causing swelling of involved joints and pain upon motion. However, there is no x-ray evidence of joint destruction, with the exception of swelling of soft tissues or early stages of osteoporosis. In stage II, there is a spread of inflammation in synovial tissue, affecting joint cavity space across joint cartilage. This inflammation will gradually result in a destruction of cartilage, accompanied by a narrowing of the joint. Severe RA, stage III, is marked by formation of pannus in the synovium. Loss of joint cartilage exposes bone beneath the cartilage. These changes will become evident on x-ray, along with erosions and signs of deformation. Stage IV is called terminal or end stage RA. The inflammatory process has subsided and formation of fibrous tissue and/or fusing of bone results in ceased joint function. Rheumatoid nodules may also be present in patients in stage IV of the disease.
In addition 125 Polish healthy individuals of both sexes (female/male: 63/62) served as controls.
IL-17A, IL-17F and IL-23R Genotyping
Three biallelic polymorphisms were studied: IL-17A (rs2275913; G-197A), IL-17F (rs763780; A7488G; His161Arg) and IL-23R (rs11209026, G1142A) as previously described (Wróbel et al. 2014). In brief, DNA was extracted from peripheral blood taken on EDTA using the Maxwell 16 Blood DNA Purification Kit (Promega Corp., Madison, WI, USA) following the recommendations of the manufacturer.
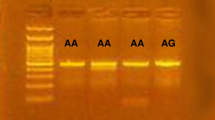
The IL-17F (rs763780; A7488G) polymorphism was analysed using a polymerase chain reaction (PCR) restriction fragment length polymorphism assay, which amplified a fragment of the promoter region of the gene using primers as previously described (Saitoh et al. 2011) (forward: 5′-GTT CCC ATC CAG CAA GAG AC-3′, and reverse: 5′-AGC TGG GAA TGC AAA CAA AC-3′). The PCR conditions were as follows: 94 °C for 3 min; 35 cycles at 94 °C for 30 s, 60 °C for 30 s and 72 °C for 30 s; and a final elongation step at 72 °C for 7 min. The PCR products were digested with the NlaIII restriction endonuclease (New England BioLabs Inc.) and analysed in 2 % agarose gel stained with ethidium bromide and visualized under UV light. Three patterns were observed following digestion and electrophoresis: a single 412 bp fragment (individuals homozygous for the IL-17F G allele, lacking the NlaIII site), three fragments of 412, 288 and 124 bp in length (heterozygous individuals) or two fragments of 288 and 124 bp (individuals homozygous for the IL-17F A allele).
PCR amplifications for the IL-17F gene polymorphism studies were carried out in the 2,720 Thermal Cycler (Applied Biosystems, Foster City, USA).
The IL-17A (rs2275913; G-197A) and IL-23R (rs11209026, G1142A) alleles were determined by real-time PCR amplifications and analysis of the typing results were performed using Roche LightCycler 480 instrument. The LightSNiP (rs2275913) assay designed by TIB MOLBIOL (GmbH, Berlin, Germany) or TaqMan SNP Genotyping Assay (rs11209026) (Life Technologies, USA) was used for detection of IL-17A and IL-23R alleles, respectively.
The IL-17F and IL-23R polymorphisms were analysed in 89 patients and 125 healthy individuals while the IL-17A genotyping was performed for 88 RA patients (71 women and 17 men) and 125 controls.
Statistical Analysis
Genotype and allele frequencies were compared between the study groups by the χ 2 test with Yates correction or Fisher’s exact test when necessary using Statistica 5.5 for Windows software. The odds ratio (OR) was calculated by Haldane’s modification of Woolf’s method and the significance of its deviation from unity was estimated by Fisher’s exact test. All p values were corrected for the number of comparisons. Probability values <0.05 were considered statistically significant.
Results
Distribution of IL-17A and IL-23R Alleles and Genotypes in Patients and Controls
IL-17A and IL-23R alleles and genotypes segregated similarly in patients and controls.
The IL-17A (rs2275913) GG, GA and AA genotypes were detected in 12 (13.6 %), 44 (50 %) and 32 (36.4 %) patients, and in 20 (16 %), 67 (53.6 %) and 38 (30.4 %) controls, respectively (Table 2). The allelic frequencies of the A variant of the IL-17A gene were 0.614 and 0.572, in patients and controls, respectively, which closely resemble those observed in other studies of the healthy European populations.
The IL-23R A variant was very rarely detected. None of the individuals tested was carrying the IL-23R AA homozygous genotype. Eighty-three patients (93.3 %) and 111 (88.8 %) healthy individuals were homozygous for the IL-23R (rs11209026) G wild-type allele. There were only 6 (6.7 %) and 14 (11.2 %) GA heterozygotes among RA patients and controls, respectively (Table 2). The allelic frequencies of the A variant of IL-23R were 0.034 and 0.044, in patients and controls, respectively.
Associations with Predisposition to the Disease, Impact of the IL-17F Polymorphism
As expected, the occurrence of RA was more frequent among female than male patients as compared to controls (72/89 vs. 63/125, OR 4.08; p < 0.001).
Among the polymorphisms studied, IL-17F (A7488G) polymorphism was found to be associated with RA. The presence of the IL-17F G variant was more frequently observed among patients than healthy individuals. This allelic variant was detected in 25 out of 89 patients with RA and only in 11 out of 125 controls (OR 3.97; p < 0.001). The allelic frequencies of the G variant of the IL-17F gene were 0.191 and 0.044, in patients and controls, respectively.
An even stronger association was observed when the IL-17F GG homozygous genotype was considered. The IL-17F GG homozygosity was detected in 9 RA patients (7 females and 2 men) and none of the controls (OR 29.62; p < 0.001) (Table 2). Similar relationships were observed when patients and controls were stratified with respect to sex (OR 13.20, p = 0.021 and OR 14.54, p = 0.071, for females and men, respectively).
Relationships of the IL-17A Genotypes with Disease Progression and Anti-TNF Treatment
There were only females among RA patients with stage 4 of the disease (14/72 vs. 0/17, for stage 4 cases among female and male patients; p = 0.063).
Interestingly, the majority of these women were carrying the IL-17A GG wild-type homozygous genotype. Among female patients, 8 out of 24 with the IL-17A GG genotype and 6 out of 47 carrying the A variant (GA or AA genotypes) were in the most advanced stages of the disease (8/24 vs. 6/47, p = 0.058; Fig. 1a).
The associations of the IL-17A (rs2275913; G-197A) polymorphism with disease progression (a) and therapy with TNF-α inhibitors (b) in women with RA. The IL-17 GG wild-type genotype was more frequently detected among female patients with the most advanced RA and the highest activity of the disease after 3 months of anti-TNF treatment
Moreover, female patients with the IL-17 GG wild-type genotype had more active disease (the highest DAS28 activity score > 5.1) after 3 months of therapy with TNF inhibitors. Among 23 female patients carrying the IL-17 GG genotype, 14 had the most active disease as compared to 15 out of 45 women with the IL-17 A variant (14/23 vs. 15/45, p = 0.040; Fig. 1b).
Relationships with the IL-23R Polymorphism
The presence of the minor allele of the IL-23R polymorphism was slightly more frequently observed among female patients in stage 3 or 4 of the disease. All women in stage 3 or 4 were carrying the IL-23R G allele (were homozygotes) as compared to 49 out of 67 women (70 %) with wild-type genotype (p = 0.164). Of note, patients homozygous for the major allele were reported to have significantly higher serum IL-17A concentrations compared with patients with the minor allele (Hazlett et al. 2012). Thus lower IL-17A producers seemed to prevail among women in stage 3 or 4 of the disease.
As the presence of the IL-17A -197A allele in healthy individuals was also found to be associated with increased IL-17A production (Espinoza et al. 2011), in further analyses we considered both genotypes associated with increased IL-17A expression (homozygosity for the major rs11209026 IL-23R allele, the presence of the minor rs2275913 IL-17A allele).
Female patients lacking both high-producer genotypes were more frequently observed among women in stage 4 disease (37/43 vs. 20/28; p = 0.220) and those with more advanced disease (with DAS28 > 5.1; 13/28 vs. 25/40; p = 0.220). However, these relationships did not reach statistical significance. Thus it seemed that the presence of the IL-23R high-producer genotype in patients carrying the IL-17A wild-type genotype weakened the (described in the previous paragraph) association with the IL-17A polymorphism.
Discussion
The polymorphisms located within genes coding for IL-17A and IL-17F appeared to play a role as genetic factors associated with susceptibility to RA, disease progression and response to treatment in the Polish population.
In the present study, the rs763780 IL-17F (A7488G) polymorphism was found to be associated with susceptibility to RA, and the presence of the G variant (and the GG genotype) was significantly more frequently observed in patients than in healthy individuals. This is a novel observation not previously described.
The association of the IL-17F (A7488G) polymorphism with susceptibility to the disease was reported, e.g. for the development of asthma (Kawaguchi et al. 2006; Qian et al. 2012), IBD (Arisawa et al. 2008; Seiderer et al. 2008), autoimmune thyroid diseases (Yan et al. 2012) and the most recently with MS (Wang et al. 2014) and acute myeloid leukaemia (Wróbel et al. 2014).
As for the RA patients, this polymorphism was also studied by Paradowska-Gorycka et al. (2010b) together with another coding substitution within the third exon of the IL-17F gene (rs2397084; A7383G; Glu26Gly). The authors did not find any association with susceptibility to the disease. However, their detailed genotype–phenotype analysis indicated that the IL-17F G (161Arg) variant of the IL-17F (rs763780) polymorphism might be associated with disease activity. Its presence was found to be correlated with a higher number of tender joints, higher mean value of DAS28-CRP and higher health assessment questionnaire score (Paradowska-Gorycka et al. 2010b).
Interestingly, Kawaguchi et al. (2006) showed the functional consequences of this IL-17F polymorphism and suggested that the IL-17 expression and activity may be suppressed in carriers of the rare G allele.
Taking the evidence together, the presence of the rare IL-17F G variant (rs763780) associated with lower expression of IL-17F was found to affect the disease susceptibility (present study) and activity of RA (Paradowska-Gorycka et al. 2010b) in the Polish population.
In our study we also found that the rs2275913 IL-17A (G-197A) polymorphism was associated with disease progression and the response to therapy with TNF-α inhibitors. These associations were observed especially in female patients carrying the wild-type homozygous genotype who more frequently presented with the most aggressive/advanced disease and characterized by a poor response to the anti-TNF treatment. These relationships have not been described previously in the literature.
So far, only three studies, by Furuya et al. (2007), Nordang et al. (2009) and the present one, have considered the role of the IL-17A promoter polymorphism in RA. The previous studies showed a weak but significant correlation with the rs2275913 IL-17A promoter polymorphism in Norwegian patients with RA (Nordang et al. 2009) and the association of the rs3804513 IL-17A (A52053197T, A > T) gene polymorphism with radiographic progression in Japanese patients with early RA (Furuya et al. 2007).
As for the relationships with susceptibility or progression of other autoimmune diseases the associations of the IL-17A rs2275913 variants with ulcerative colitis in Koreans (Kim et al. 2011) and Japanese (Hayashi et al. 2013), but not for our Caucasian population, were described. In the latter study IL-17A polymorphism was also found to be associated with the noncontinuous and pancolitis phenotypes of ulcerative colitis (Hayashi et al. 2013). Interestingly, this polymorphism was also described to affect carcinogenesis. For example, some associations with the risk of gastric cancer, the development of intestinal-type cancer or diffuse-type cancer, and gastric mucosal atrophy were reported (Shibata et al. 2009).
We observed a higher frequency of females carrying the wild-type genotype of the rs2275913 IL-17A polymorphism among patients with the highest stages of the disease and in those with the most active disease after 3 months of anti-TNF-α treatment. This is a novel observation not previously described.
Interestingly, Espinoza et al. (2011) demonstrated that in vitro stimulated T cells from healthy individuals possessing the 197A allele produced significantly more IL-17 than those without the 197A allele. Thus, in our study the potential low producers of IL-17A appeared to exhibit worse prognosis. It is difficult to discuss this relationship. First of all, it would be of interest to assess whether the association between IL-17A gene polymorphism and expression observed in healthy individuals (Espinoza et al. 2011) is also valid in RA patients, and furthermore to verify the association after subsequent 3 and 6 months of anti-TNF treatment. These issues warrant further studies. Moreover, it should be taken into account that in RA IL-17A acts as an important component of a more complex cytokine network involving such factors as proinflammatory cytokines (TNF-α and IL-6) or chemokines (Bettelli et al. 2008; Langrish et al. 2005). Thus the observed relationship could be more complex. Nevertheless, our results imply that polymorphism located within the IL-17A encoding gene may have prognostic value for patients with RA.
We did not find any significant association with the rs11209026 IL-23R polymorphism with RA. Our observation concurs with the other studies. The results of very recent meta-analyses suggested that other polymorphisms located within the IL-23R gene were potentially associated with the development of RA in Europeans, including the IL-23R rs134315, rs10489629 and rs7517847 polymorphisms (Song et al. 2012; Zhai et al. 2012).
There are, however, a few reports that showed the correlation of the rs11209026 IL-23R polymorphism with the development and course of other human autoimmune disorders, such as psoriatic arthritis (Hinks et al. 2011) or ankylosing spondylitis (Sáfrány et al. 2009).
Moreover, the rs11209026 IL-23R polymorphism was reported to affect the IL-17A serum level in RA patients. Patients homozygous for the major allele had significantly higher serum IL-17A concentrations compared with patients with the minor allele (Hazlett et al. 2012). Therefore, in our study we also considered the genotypes associated with increased IL-17A expression (homozygosity for the major rs11209026 IL-23R allele and the presence of the minor rs2275913 IL-17A allele). However, no significant relationships were detected.
In summary, we were able to detect some associations with IL-17A and IL-17F but not IL-23R gene polymorphism in Polish patients with RA. These relationships might be attributed to the fact that epidemiological results often do not coincide with functional studies because RA is a complex disease with contributions from multiple genes, different genetic backgrounds and environmental factors. One of the factors that could be considered is the signal transducer and activator of transcription (STAT)3 belonging to STAT proteins that play a key role in mediating signals during Th1, Th2 and Th17 differentiation. STAT3 has critical functions in development of IL-17-secreting Th cells in the cytokine environment or the expression of IL-17A, IL-17F, and retinoic acid-related orphan receptor (ROR-γt) in Th17 cultures (Paradowska-Gorycka et al. 2010a, b; Yang et al. 2007). According to our knowledge, these relationships have not been analysed so far.
Obviously, these results should be confirmed in a more extended study, including patients from other centers. A relatively small size of patients cohort analysed in the present study constitutes the most important limitation of our work.
It would also be of interest to relate the results of the polymorphism studies with the expression and serum concentration of IL-17A, IL-17F and IL-23, and other proinflammatory cytokines, such as TNF-α.
In conclusion, the results of our study strongly suggest that the polymorphisms within the IL-17A and IL-17F genes affect the susceptibility to RA, disease progression and response to treatment with anti-TNF inhibitors.
References
Aggarwal S, Ghilardi N, Xie MH et al (2003) Interleukin-23 promotes a distinct CD4 T cell activation state characterized by the production of interleukin-17. J Biol Chem 278:1910–1914
Annunziato F, Cosmi L, Liotta F et al (2009) Type 17 T helper cells-origins, features and possible roles in rheumatic disease. Nat Rev Rheumatol 5:325–331
Arisawa T, Tahara T, Shibata T et al (2008) The influence of polymorphisms of interleukin-17A and interleukin-17F genes on the susceptibility to Ulcerative Colitis. J Clin Immunol 28:44–49
Bettelli E, Korn T, Oukka M et al (2008) Induction and effector functions of T(H)17 cells. Nature 453:1051–1057
Espinoza JL, Takami A, Nakata K et al (2011) A genetic variant in the IL-17 promoter is functionally associated with acute graft-versus-host disease after unrelated bone marrow transplantation. PLoS One 6:e26229
Furuya T, Hakoda M, Ichikawa N et al (2007) Associations between HLA-DRB1, RANK, RANKL, OPG, and IL-17 genotypes and disease severity phenotypes in Japanese patients with early rheumatoid arthritis. Clin Rheumatol 26:2137–2141
Hayashi R, Tahara T, Shiroeda H et al (2013) Influence of IL17A polymorphisms (rs2275913 and rs3748067) on the susceptibility to ulcerative colitis. Clin Exp Med 13:239–244
Hazlett J, Stamp LK, Merriman T et al (2012) IL-23R rs11209026 polymorphism modulates IL-17A expression in patients with rheumatoid arthritis. Genes Immun 13:282–287
Hinks A, Martin P, Flynn E et al (2011) Subtype specific genetic associations for juvenile idiopathic arthritis: ERAP1 with the enthesitis related arthritis subtype and IL23R with juvenile psoriatic arthritis. Arthritis Res Ther 13:R12
Hot A, Zrioual S, Toh M et al (2011) IL-17A- versus IL-17F-induced intracellular signal transduction pathways and modulation by IL-17RA and IL-17RC RNA interference in rheumatoid synoviocytes. Ann Rheum Dis 70:341–348
Iwakura Y, Ishigame H (2006) The IL-23/IL-17 axis in inflammation. J Clin Invest 116:1218–1222
Kawaguchi M, Takahashi D, Hizawa N et al (2006) IL-17F sequence variant (His161Arg) is associated with protection against asthma and antagonizes wild-type IL-17F activity. J Allergy Clin Immunol 117:795–801
Kim SW, Kim ES, Moon CM et al (2011) Genetic polymorphisms of IL-23R and IL-17A and novel insights into their associations with inflammatory bowel disease. Gut 60:1527–1536
Kotake S, Udagawa N, Takahashi N et al (1999) IL-17 in synovial fluids from patients with rheumatoid arthritis is a potent stimulator of osteoclastogenesis. J Clin Invest 103:1345–1352
Langrish CL, Chen Y, Blumenschein WM et al (2005) IL-23 drives a pathogenic T cell population that induces autoimmune inflammation. J Exp Med 201:233–240
Lee DM, Weinblatt ME (2001) Rheumatoid arthritis. Lancet 358:903–911
Li N, Wang JC, Liang TH et al (2013) Pathologic finding of increased expression of interleukin-17 in the synovial tissue of rheumatoid arthritis patients. Int J Clin Exp Pathol 6:1375–1379
Lubberts E (2010) Th17 cytokines and arthritis. Semin Immunopathol 32:43–53
McKenzie BS, Kastelein RA, Cua DJ (2006) Understanding the IL-23-IL-17 immune pathway. Trends Immunol 27:17–23
Miossec P, Korn T, Kuchroo VK (2009) Interleukin-17 and type 17 helper T cells. N Engl J Med 361:888–898
Nordang GB, Viken MK, Hollis-Moffatt JE et al (2009) Association analysis of the interleukin 17A gene in Caucasian rheumatoid arthritis patients from Norway and New Zealand. Rheumatology 48:367–370
Paradowska-Gorycka A, Grzybowska-Kowalczyk A, Wojtecka-Lukasik E et al (2010a) IL-23 in the pathogenesis of rheumatoid arthritis. Scand J Immunol 71:134–145
Paradowska-Gorycka A, Wojtecka-Lukasik E, Trefler J et al (2010b) Association between IL-17F gene polymorphisms and susceptibility to and severity of rheumatoid arthritis (RA). Scand J Immunol 72:134–141
Qian F, Zhang Q, Zhou L et al (2012) Association between polymorphisms in IL17F and male asthma in a Chinese population. J Investig Allergol Clin Immunol 22:257–263
Sáfrány E, Pazár B, Csöngei V et al (2009) Variants of the IL23R gene are associated with ankylosing spondylitis but not with Sjögren syndrome in Hungarian population samples. Scand J Immunol 70:68–74
Saitoh T, Tsukamoto N, Koiso H et al (2011) Interleukin-17F gene polymorphism in patients with chronic immune thrombocytopenia. Eur J Haematol 87:253–258
Seiderer J, Elben I, Diegelmann J et al (2008) Role of the novel Th17 cytokine IL-17F in inflammatory bowel disease (IBD): upregulated colonic IL-17F expression in activated Crohn’s disease and analysis of the IL-17F p.His161Arg polymorphism in IBD. Inflamm Bowel Dis 14:437–445
Shibata T, Tahara T, Hirata I et al (2009) Genetic polymorphism of interleukin-17A and -17F genes in gastric carcinogenesis. Hum Immunol 70:547–551
Song GG, Bae SC, Choi SJ et al (2012) Associations between interleukin-23 receptor polymorphisms and susceptibility to rheumatoid arthritis: a meta-analysis. Mol Biol Rep 39:10655–10663
Wang S, Zhai H, Su Y et al (2014) IL-17F but not IL-17A gene polymorphism confers risk to multiple sclerosis in a Chinese Han population. J Neurol Sci 342:133–136
Wendling D (2008) Interleukin 23: a key cytokine in chronic inflammatory disease. Joint Bone Spine 75:517–519
Wheeless CR (2012) Rheumatoid arthritis. In: Wheeless CR, Nunley JA, Urbaniak JR (eds) Wheeless’ Text of Orthopaedics. Data Trace Internet Publishing, LLC; Available at www.wheelessonline.com
Wilke CM, Bishop K, Fox D et al (2011) Deciphering the role of Th17 cells in human disease. Trends Immunol 32:603–611
Wróbel T, Gębura K, Wysoczańska B et al (2014) IL-17F gene polymorphism is associated with susceptibility to acute myeloid leukemia. J Cancer Res Clin Oncol 140:1551–1555
Yan N, Yu YL, Yang J et al (2012) Association of interleukin-17A and -17F gene single-nucleotide polymorphisms with autoimmune thyroid diseases. Autoimmunity 45:533–539
Yang XO, Panopoulos AD, Nurieva R et al (2007) STAT3 regulates cytokine-mediated generation of inflammatory helper T cells. J Biol Chem 282:9358–9363
Zhai Y, Xu K, Huang F et al (2012) Association of interleukin 23 receptor gene polymorphisms (rs10489629, rs7517847) with rheumatoid arthritis in European population: a meta-analysis. Mol Biol Rep 39:8987–8994
Acknowledgments
This work was supported in part by the Polish National Science Centre (Grant no. 2011/01/B/NZ5/05367).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Bogunia-Kubik, K., Świerkot, J., Malak, A. et al. IL-17A, IL-17F and IL-23R Gene Polymorphisms in Polish Patients with Rheumatoid Arthritis. Arch. Immunol. Ther. Exp. 63, 215–221 (2015). https://doi.org/10.1007/s00005-014-0319-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00005-014-0319-5