Abstract
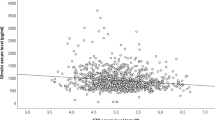
Hyperthyroidism is characterized by hyperphagia and increased basal metabolic rate. Ghrelin peptide is implicated in food intake through activation of the orexigenic neuropeptide Y/agouti related protein in the arcuate nucleus of hypothalamus. Also different studies suggested that ghrelin might play a role in states of energy insufficiency, controlling body weight. We therefore evaluate ghrelin levels in severe hyperthyroidism before and after medical treatment when euthyroidism was achieved, in order to evaluate its possible role in the increase of apettite and in the metabolic changes observed in hyperthyroidism. Serum ghrelin and insulin levels were measured after an oral glucose tolerance test (OGTT), in 7 severe hyperthyroid female patients, before and after medical treatment when euthyroidism was achieved. Body mass index (BMI), percentage of body fat and lean mass was also estimated in hyperthyroidism as well as in euthyroidism. Basal insulin levels were statistically higher in hyperthyroid patients with respect to euthyroid state after treatment (p=0.02, t=3.379), while homeostasis model assessment (HOMA) index for insulin sensitivity was statistically higher in hyperthyroidism (group 1) compared to euthyroidism (group 2) (1.64±0.69 vs 0.78±0.44, p=0.019, t=3.389). Fasting ghrelin concentrations were significantly reduced in group 1 compared to group 2 (938±578 pg/ml vs 1402±566 pg/ml, p<0.05, t=−2.489). Oral glucose loading induced suppression of ghrelin level in both groups, but the area under the curve for ghrelin during the OGTT in euthyroidism was greater compared to hyperthyroidism (p=0.05, t=−2.485). After medical treatment, a statistically significant increase in BMI (23.1 ±4.3 vs 25.9±5.1) (p=0.007, t=−4.399) was also observed. In hyperthyroidism, basal ghrelin levels showed a negative correlation with BMI (p=0.042, r=−0.829), insulin (p<0.001, r=−1.000), and HOMA index (p=0.019, r=−0.886). No correlation was found between ghrelin levels and thyroid hormone values. Ghrelin levels are decreased in hyperthyroidism and increase when euthyroidism is achieved. BMI and insulin are the main factors that influence ghrelin concentration in hyperthyroidism. T3 and T4 levels do not influence ghrelin levels. There is no evidence that ghrelin is responsible for the increase apetitte seen in hyperthyroidism.
Similar content being viewed by others
References
Danforth E Jr. The role of thyroid hormones and insulin in the regulation of energy metabolism. Am J Clin Nutr 1983, 38: 1006–17.
Danforth E, Burger A. The role of thyroid hormones in the control of energy expenditure. Clin Endocrinol Metab 1984, 13: 581–95.
Pijl H, de Meijer PHEM, Langius J, et al. Food choice in hyperthyroidism: potential influence of the autonomic nervous system and brain serotonin precursor availability. J Clin Endocrinol Metab 2001, 86: 5848–53.
Kojima M, Hosoda H, Date Y, Nakazato M, Matsuo H, Kangawa K. Ghrelin is a growth-hormone-releasing acylated peptide from stomach. Nature 1999, 402: 656–60.
Tschöp M, Smiley DL, Heiman ML. Ghrelin induces adiposity in rodents. Nature 2000, 407: 908–13.
Nakazato M, Murakami N, Date Y, et al. A role for ghrelin in the central regulation of feeding. Nature 2001, 409: 194–8.
Wren AM, Small CJ, Ward HL, et al. The novel hypothalamic peptide ghrelin stimulates food intake and GH secretion. Endocrinology 2000, 141: 4325–8.
Asakawa A, Inui A, Kaga T, et al. Ghrelin is an appetite-stimulatory signal from stomach with structural resemblance to motilin. Gastroenterology 2001, 120: 337–45.
Wren AM, Seal LJ, Cohen MA, et al. Ghrelin enhances appetite and increases food intake in humans. J Clin Endocrinol Metab 2001, 86: 5992–5.
Howard AD, Feighner SD, Cully DF, et al. A receptor in pituitary and hypothalamus that functions in growth hormone release. Science 1996, 273: 974–7.
Guan XM, Yu H, Palyha OC, et al. Distribution of mRNA encoding the growth hormone secretagogue receptor in brain and peripheral tissues. Brain Res Mol Brain Res 1997, 48: 23–9.
Yokote R, Sato M, Matsubara S, et al. Molecular cloning and gene expression of growth hormone-releasing peptide receptor in rat tissues. Peptides 1998, 19: 15–20.
Jobst EE, Enriori PJ, Cowely AM. The electrophysiology of feeding circuits. Trends Endocrinol Metab 2004, 15: 488–99.
Shiiya T, Nakazato M, Mizuta M, et al. Plasma ghrelin levels in lean and obese humans and the effect of glucose on ghrelin secretion. J Clin Endocrinol Metab 2002, 87: 240–4.
Riis AL, Hansen TK, Møller N, Weeke J, Jørgensen JOL. Hyperthyroidism is associated with suppressed circulating ghrelin levels. J Clin Endocrinol Metab 2003, 88: 853–7.
Giménez-Palop O, Giménez-Pérez G, Mauricio D, et al. Circulating ghrelin in thyroid dysfunction is related to insulin resistance and not to hunger, food intake or anthropometric changes. Eur J Endocrinol 2005, 153: 73–9.
Matsuda M, DeFronzo R. Insulin sensitivity indices obtained from oral glucose tolerance testing: comparison with the euglycemic insulin clamp. Diabetes Care 1999, 22: 1462–70.
Lukaski HL. Methods for the assessment of human body composition: traditional and new. Am J Clin Nutr 1987, 46: 537–56.
Caminos JE, Seoane LM, Tovar SA, Casanueva FF, Dieguez C. Influence of thyroid status and growth hormone deficiency on ghrelin. Eur J Endocrinol 2002, 147: 159–163.
Cummings DE, Purnell JQ, Frayo RS, Schmidova K, Wisse BE, Weigle DS. A preprandial rise in plasma ghrelin levels suggests a role in meal initiation in humans. Diabetes 2001, 50: 1714–9.
Nagaya N, Uematsu M, Kojima M, et al. Elevated circulating level of ghrelin in cachexia associated with chronic heart failure: relationships between ghrelin and anabolic/catabolic factors. Circulation 2001, 104: 2034–8.
Holdsworth CD, Besser GM. Influence of gastric emptying rate and of insulin response on oral glucose tolerance in thyroid disease. Lancet 1968, 2: 700–2.
Doar JWH, Stampt TCB, Wynn V, Audhya TK. Effects of oral and intravenous glucose loading in thyrotoxicosis. Studies of plasma glucose, free fatty acid, plasma insulin and blood pyruvate levels. Diabetes 1969, 18: 633–9.
Nilsson OR, Kagedal B, Tegler L. Insulin release and carbohydrate tolerance in hyperthyroid patients during non-selective or selective B-1 adrenoceptor blockade. Acta Endocrinol (Copenh) 1980, 93: 179–85.
Dimitriadis G, Baker B, Marsh H, et al. Effect of thyroid hormone excess on action, secretion, and metabolism of insulin in humans. Am J Physiol 1985, 248: E593–601.
O’Meara NM, Blackman JD, Sturis J, Polonsky KS. Alterations in the kinetics of C-peptide and insulin secretion in hyperthyroidism. J Clin Endocrinol Metab 1993, 76: 79–84.
Date Y, Nakazato M, Hashiguchi S, et al. Ghrelin is present in pancreatic alpha-cells of humans and rats and stimulates insulin secretion. Diabetes 2002, 51: 124–9.
Broglio F, Arvat E, Benso A, et al. Ghrelin, a natural GH secretagogue produced by the stomach, induces hyperglycemia and reduces insulin secretion in humans. J Clin Endocrinol Metab 2001, 86: 5083–6.
Saad FM, Bernaba B, Hwu CM, et al. Insulin regulates plasma ghrelin concentrations. J Clin Endocrinol Metab 2002, 87: 3997–4000.
Cummings DE, Weigle DS, Frayo RS, et al. Plasma ghrelin levels after diet-induced weight loss or gastric bypass surgery. N Engl J Med 2002, 346: 1623–30.
Burggraaf J, Tulen JHM, Lalezari S, et al. Sympathovagal imbalance in hyperthyroidism. Am J Physiol 2001, 281: E190–5.
Pöykkö SM, Kellokoski E, Hörkkö S, Kauma H, Kesäniemi A, Ukkola O. Low plasma ghrelin is associated with insulin resistance, hypertension, and the prevalence of type 2 diabetes. Diabetes 2003, 52: 2546–53.
Schwartz WM, Porte D Jr. Diabetes, obesity, and the brain. Science 2005, 307: 375–9.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Theodoropoulou, A., Psyrogiannis, A., Metallinos, I.C. et al. Ghrelin response to oral glucose load in hyperthyroidism, before and after treatment with antithyroid drugs. J Endocrinol Invest 32, 94–97 (2009). https://doi.org/10.1007/BF03345693
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/BF03345693