Abstract
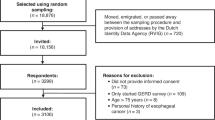
In order to analyze factors that influence an interviewer's judgement of the validity of responses given by patients on the duration of their neoplastic signs and symptoms, 183 consecutive symptomatic patients hospitalized for a digestive tract neoplasm were personally interviewed. The validity of the answers was judged by the interviewers to be high in 156 cases (85%), and low in 27 (15%). The subjective validity of the interview (SVI) was inversely related to the time elapsed from first medical symptom to interview (TFMSI), even after adjusting for the duration of the interview (p < 0.05). SVI was not influenced by whether patient and interviewer agreed on the first symptom. SVI was inversely related to educational level (p < 0.01) and to occupational class (p = 0.04).
Patients whose Karnofsky's Index (KI) was ⩾ 80 were over twice as likely to yield valid responses (TFMSI-adjusted odds ratio [OR] = 2.82, p = 0.037). Multivariate analyses selected education, TFMSI and KI as independent predictors of the interviewer assessment. The SVI of patients admitted to the hospital through the Emergency Department was lower than that of subjects whose admission was planned (OR = 6.49, p = 0.005). In this study SVI related in a logical manner to the characteristics of the interview, of the subjects and of their clinical course. It hence appeared to reasonably estimate the validity of data collected. Identifying factors that affect the reliability of patients' responses would help increase the validity of studies on the duration of cancer symptoms.
Similar content being viewed by others
Abbreviations
- FMS:
-
First medical symptom
- FPS:
-
First symptom according to the patient
- IAFMS:
-
Importance attributed by the patient to the first symptom
- KI:
-
Karnofsky's Index
- SVI:
-
Subjective validity of the interview
- TFMSI:
-
Time from first medical symptom to interview
References
Farr CE. Delay in the treatment of cancer. Am J Med Sciences 1922; 64: 712–715.
Pack GT, Gallo JS. The culpability for delay in the treatment of cancer. Am J Cancer 1938; 33: 443–462.
King RA, Leach JE. Factors contributing to delay by patients in seeking medical care. Cancer 1950; 3: 571–579.
Robbins GF, Conte AJ, Leach JE, MacDonald M. Delay in diagnosis and treatment of cancer. JAMA 1950; 143: 346–348.
Gray DB, Ward GE. Delay in diagnosis of carcinoma of the stomach. An analysis of 104 cases. Am J Surg 1952; April: 524–526.
Mustard RA, Ibberson O. Carcinoma of the esophagus: A review of 381 cases admitted to Toronto General Hospital 1937–1953 inclusive. Ann Surg 1956; 144: 927–940.
Goldsen RK, Gerhardt PR, Handy VH. Some factors related to patient delay in seeking diagnosis for cancer symptoms. Cancer 1957; 10: 1–7.
Kutner B, Makover HB, Oppenheim A. Delay in the diagnosis and treatment of cancer: A critical analysis of the literature. J Chron Dis 1958; 7: 95–120.
Kutner B, Gordon G. Seeking care for cancer. J Health Human Behav 1961; 2: 171–178.
Barber KW, Gage RP, Priestley JT. Significance of duration of symptoms and size of lesion in the prognosis of gastric carcinoma. Surg Gynecol Obstetr 1961; 113: 673–676.
Whitted HH. Determinants of acceptance to education and utilization of services for cancer detection and care among low income groups. Medical Annals District Columbia 1962; 31: 6–11.
Rowe-Jones DC, Aylett SO. Delay in treatment in carcinoma of colon and rectum. Lancet 1965; 2: 973–976.
Blackwell B. The literature of delay in seeking medical care for chronic illnesses. Health Educ Monogr 1963; 16: 3–31.
Sweet R, Twaddle A. An exploration of delay in hospitalization. Inquiry 1969; 6: 35–41.
Battistella RM. Factors associated with delay in the initiation of physicians' care among late adulthood persons. Am J Public Health 1971; 61: 1348–1361.
Antonovsky A, Hartman H. Delay in the detection of cancer: A review of the literature. Health Educ Monogr 1974; 2: 98–128.
Porta M, Belloc J, Malats N. Estudios españoles sobre la demora diagnóstica y terapéutica en el cáncer. Un análysis crítico de su metodología y resultados. In: Porta M, Alvarez-Dardet C (eds), Revisiones en Salud Pública, 1. Barcelona: Masson, 1989: 197–226.
Hackett TP, Cassem NH, Raker JW. Patient delay in cancer. N Engl J Med 1973; 289: 14–20.
Greenwald HP, Becker SW, Nevitt MC. Delay and noncompliance in cancer detection. A behavioral perspective for health planners. Milbank Memorial Fund Quart 1978; 56: 212–230.
Gardner B. The relationship of delay in treatment to prognosis in human cancer. Progr Clin Cancer 1978; 7: 123–133.
Keddie N, Hargreaves A. Symptoms of carcinoma of the colon and rectum. The Lancet 1968; 2: 749–750.
Younghusband JD, Aluwihare APR. Carcinoma of the oesophagus: Factors influencing survival. Br J Surg 1970; 57: 422–430.
Lim BS, Dennis CR, Gardner B, Newman J. Analysis of survival versus patient and doctor delay of treatment in gastrointestinal cancer. Am J Surg 1974; 127: 210–214.
Irvin TT, Greaney MG. Duration of symptoms and prognosis of carcinoma of the colon and rectum. Surg Gynecol Obstetr 1977; 144: 883–886.
Holliday HW, Hardcastle JD. Delay in diagnosis and treatment of symptomatic colorectal cancer. The Lancet 1979; 1: 309–311.
Bassett ML, Bennett SA, Goulston KJ. Colorectal cancer. A study of 230 patients.Med J Aust 1979; 1: 589–592.
Pescatori M, Maria G, Beltrani B, Mattana C. Site, emergency, and duration of symptoms in the prognosis of colorectal cancer. Dis Col Rect 1982; 25: 33–40.
Robinson E, Mohilever J, Zidan J, Sapir D. Delay in diagnosis of cancer. Possible effects on the stage of disease and survival. Cancer 1984; 54: 1454–1460.
Robinson E, Mohilever J, Zidan J, Sapir D. Colorectal cancer: Incidence, delay in diagnosis and stage of disease. Eur J Cancer Clin Oncol 1986; 22: 157–161.
Akdas A, Kirkali Z, Remzi D. The role of delay in stage-III testicular tumors. Eur Urol 1986; 12: 151–153.
Mikulin T, Hardcastle JD. Gastric carlcer-Delay in diagnosis and its causes. Eur J Cancer Clin Oncol 1987; 23: 1683–1690.
Saunders LD. Differences in the timeliness of diagnosis, breast and cervical cancer, San Francisco 1974–85. Am J Public Health 1989; 79: 69–70.
Kulkarni PR, Vernon SW, Jackson GL, et al. Stage at diagnosis of breast cancer. Comparison in a FeeFor-Service and Health Maintenance Organization Practice. Med Care 1989; 27: 608–622.
Zilling TL, Walther BS, Ahren B. Delay in diagnosis of pastric cancer: A prospective study evaluating doctors' and patients' delay and its influence on five year survival. Anticancer Res 1990; 10: 411–426.
Kaufman S, Grabau JC, Lore JM. Symptomatology in head and neck cancer: A quantitative review of 385 cases. Am J Public Health 1980: 70: 520–522.
Elwood JM, Moorehead WP. Delay in diagnosis and long-term survival in breast cancer. Br Med J 1980; 280:1291–1294.
Bosl GJ, Vogelzang NJ, Goldman A, et al. Impact of delay in diagnosis on clinical stage of testicular cancer. Lancet 1981; 2: 970–972.
Nilsson E, Bolin S, Sjödahl R. Carcinoma of the colon and rectum. Delay in diagnosis. Acta Chir Scand 1982; 148: 617–622.
Feldman JG, Saunders M, Carter AC, Gardner B. The effects of patient delay and symptoms other than a lump on survival in breast cancer. Cancer 1983; 51: 1226–1229.
Bosch FX, Español J, Campillo M, et al. Análisis general del Registro de Tumores del Hospital de Sta. Caterina de Girona. Descripción de la serie y estudio del retardo diagnóstico y terapéutico. Rev Esp Oncol 1983; 30: 209–223.
Fowler WC, Freeman AC, Hulka BS, et al. Delays in cervical cancer treatment: an assessment of patient and provider characteristics. In: Advances in cancer control: Epidemiology and research. New York: Alan R. Liss, 1984: 265–274.
Smith EM, Anderson B. The effects of symptoms and delay in seeking diagnosis on stage of disease at diagnosis among women with cancers of the ovary. Cancer 1985; 56: 2727–2732.
GIVIO (Interdisciplinary Group for Cancer Care Evaluation). Reducing diagnostic delay in breast cancer. Possible therapeutic implications. Cancer 1986; 58: 1756–1761.
Marshall JR, Funch DP. Gender and illness behavior among colorectal cancer patients. Women Health 1986; 11: 67–82.
Weissman JS, Stern R, Fielding SL, Epstein AM. Delayed access to health care: Risk factors, reasons, and consequences. Ann Intern Med 1991; 114: 325–331.
Vineis P, Fornero G, Magnino A, et al. Diagnostic delay, clinical stage, and social class: a hospital based study. J Epidemiol Community Health 1993; 47: 229–231.
Porta M, Gallén M, Malats N, Planas J. Influence of ‘diagnostic delay’ upon cancer survival: An analysis of five tumour sites. J Epidemiol Community Health 1991; 45: 225–230.
Maguire A, Porta M, Malats N, et al. Cancer survival and the duration of symptoms. An analysis of possible forms of the risk function. Eur J Cancer 1994; 30A: 785–792.
Cobb B, Clark RL, McGuire C, Howe CD. Patient-responsible delay of treatment in cancer. Cancer 1954; 7: 920–926.
Cassileth BR, Clark WH, Heiberger RM, et al. Relationship between patients' early recognition of melanoma and depth of invasion. Cancer 1982; 49: 198–200.
MacArthur C, Smith A. The symptom presentation of breast cancer: Is pain a symptom? Community Med 1983; 5: 220–3.
MacArthur C, Smith A. Factors associated with speed of diagnosis, referral, and treatment in colorectal cancer. J Epidemiol Community Health 1984; 38: 122–126.
Merletti F, Faggiano F, Boffetta P, et al. Topographic classification, clinical characteristics, and diagnostic delay of cancer of the larynx/hypopharynx in Torino, Italy. Cancer 1990; 66: 1711–1716.
Funch DP. The role of patient delay in the evaluation of breast self-examination. J Psychosoc Oncol 1984; 2: 31–39.
Funch DP. Diagnostic delay in symptomatic colorectal cancer. Cancer 1985; 56: 2120–2124.
Retchin SM, Brown B. Management of colorectal cancer in Medicare Health Maintenance Organizations. J Gen Intern Med 1990; 5: 110–114.
Feigl P, Glaeflke G, Ford L, et al. Studying patterns of cancer care: How useful is the medical record?. Am J Public Health 1988; 78: 526–533.
Funch DP. Predictors and consequences of symptom reporting behaviors in colorectal cancer patients. Med Care 1988; 26: 1000–1008.
Steptoe A, Sutcliffe I, Allen B, Coombes C. Satisfaction with communication, medical knowledge, and coping style in patients with metastatic cancer. Soc Sci Med 1991; 32: 627–632.
Malats N, Belloc J, Gallén M, Porta M. Disagreement between hospital medical records and a structured patient interview on the type and date of the first symptom in cancers of the digestive tract. Rev Epidemiol Santé Publique 1995; 43: 533–540.
Polissar L, Sim D, Francis A. Survival of colorectal cancer patients in relation to duration of symptoms and other prognostic factors. Dis Col Rect 1981 24: 364–369.
MacDonald I, Kotin P. Biological predeterminism in gastric carcinoma and the limiting factor of curability. Surg Gynecol Obstetr 1954; 98: 148–152.
Becker MH, Maiman LA. Sociobehavioral determinants of compliance with health and medical care recommendations. Med Care 1975; 13: 10–24.
Twaddle AC. Sickness and the sickness career: Some implications. In: Eisenberg L, Kleinman A (eds), The relevance of social science for medicine. Dordrecht: D. Reidel, 1981: 111–133.
MacArthur C, Pendleton LL, Smith A. Treatment delay in patients with bladder tumours. J Epidemiol Community Health 1985; 39: 63–66.
Berman SH, Wandersman A. Measuring knowledge of cancer. Soc Sci Med 1991; 32: 1245–1255.
Belloc J, Porta M, Malats N, et al. El síntoma inicial atribuible al cáncer en los tumours del tubo digestivo. Un análisis de la concordancia entre el paciente y el médico. Med Clin (Barc) 1994; 103: 401–407.
Porta M, Gallén M, Belloc J, Malats N. Predictors of the interval between onset of symptoms and first medical visit in patients with digestive tract cancer. Int J Oncol 1996; 8: 941–949.
SAS Institute Inc. SAS/STAT guide for personal computers. Version 6 edition. Cary, NC: SAS Institute Inc., 1987.
Kleinbaum DG, Kupper LL, Morgenstern H. Epidemiologic research. Principles and quantitative methods. Belmont, CA: Lifetime Learning Publications, 1982: 320–376.
Sudman S, Bradburn NM. Asking questions. A practical guide to questionnare design. San Francisco: Jossey-Bass, 1987.
Loftus EF, Smith KD, Klinger MR, Fiedler J. Memory and mismemory for health events. In: Tanur JM (ed), Questions about questions: Inquiries into the cognitive bases of surveys. New York: Rissel Sage Foundation, 1992: 102–137.
Molina MC, Porta M, Malats N, et al. Percepción del inicio y la evolución de la sintomatología en pacientes hospitalizados con cáncer del tubo digestivo. Neoplasia 1994; 11: 119–125.
Feinstein AR, Pritchett JA, Schimpff CR. The epidemiology of cancer therapy. IV. The extraction of data from medical records. Arch Intern Med 1969; 123:571–590.
McKenna MT, Speers M, Mallin K, Warnecke R. Agreement between patient self-reports and medical records for pap smear histories. Am J Prev Med 1992; 8: 287–291.
Bush TL, Miller SR, Golden AL, Hale WE. Selfreport and medical record report agreement of selected medical conditions in the elderly. Am J Public Health 1989; 79: 1554–1556.
Whitman S, Lacey L, Ansell D, et al. Do chart reviews and interviews provide the same information about breast and cervical cancer screening? Int J Epidemiol 1993; 22: 393–397.
Mechanic D. Social psychologic factors affecting the presentation of bodily complaints. N Engl J Med 1972; 286: 1132–1139.
Becker MH, Maiman LA. Models of health-related behavior. In: Mechanic D (ed), Handbook of health, health care and the health professions. New York: The Free Press, 1982: 539–568.
Boyle P, Veronesi U, Tubiana M, et al. European School of Oncology Advisory Report to the European Commission for the ‘Europe Against Cancer Programme’ European Code Against Cancer. Eur J Cancer 1995; 31A: 1395–1405.
Calman K (Chairman). A policy framework for commisioning cancer services. A report by the Expert Advisory Group on cancer to the Chief Medical Officers of England and Wales. London: Department of Health, 1995: 22.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Porta, M., Malats, N., Belloc, J. et al. Do we believe what patients say about their neoplastic symptoms?. Eur J Epidemiol 12, 553–562 (1996). https://doi.org/10.1007/BF00499453
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF00499453