Abstract
Background
The COVID-19 pandemic disproportionately affected minorities in population rates of infection, hospitalization, and mortality. However, little is known about the broader racial disparities in fears and perceptions about the pandemic and getting treated.
Objective
To examine disparities in perceived risks of COVID-19 and getting medical care.
Methods
Using the nationally representative Stanford University School of Medicine Coronavirus Attitudes and Behaviors Survey fielded in May of 2020, we examine racial and ethnic disparities in eight measures on the perceived risks of COVID-19. We use regression analysis to risk adjust perceptions controlling for 10 socioeconomic, demographic, and health variables.
Results
Black respondents were 15 percentage points more likely than White respondents to believe the pandemic would not end by Summer 2020 (92% vs 77%, p < .01), and were 19 percentage points more likely than any other race to feel a need to protect their family from COVID-19 (81% vs 62%, p < .01). Latinx respondents were 10 percentage points more fearful than White respondents of catching COVID-19 in public places (55% vs 45%, p < 0.01). Black respondents were 20 percentage points more likely than White respondents to think they would need medical care if infected (71% vs 51%, p < .01), and 18 percentage points more likely to think they would need to be hospitalized (59% vs 41%, p < .01). The proportion of Black respondents believing that the hospital would not have enough capacity to treat them if infected with COVID-19 was 12 percentage points higher than White respondents (41% vs 29%, p < 0.05).
Conclusion
Disparities in the COVID-19-related perceived risks and mistrust in healthcare across racial and ethnic groups existed at the beginning of the COVID-19 pandemic. As we enter into a post-COVID New Normal, new policies must ensure that the causes of this widespread fear and distrust in the healthcare system are understood and reversed.
Similar content being viewed by others
Structural inequities in health have been present in the USA for a very long time [1,2,3,4]. Compared to White patients, Black patients tend to have lower insurance coverage, lower access to care, poorer health, and poorer quality of care and health outcomes [1, 5, 6]. Persistent social and economic inequalities further put strain on Black people’s health [2, 4, 7]. While the COVID-19 pandemic has exacted an enormous toll on the overall general population, its disproportionate effect on people who are Black, Latinx, and American Indian, has drawn renewed attention to health disparities in the US [2, 6]. Compared to White people, Non-White people were at higher risk of exposure to COVID-19 and have had higher population rates of infection, hospitalizations, and deaths per 100,000 capita [2, 6,7,8,9,10,11,12,13,14]. As an example, in Wisconsin Black people account for 6% of the population but 50% of all COVID-19 deaths [15].
At the federal level, several policy actions were taken to address these disparities. President Trump made COVID-19 testing more accessible and affordable by expanding testing at Federally Qualified Health Centers and local retail outlets (e.g., pharmacies) and funded state and local jurisdictions to support contact tracing, surveillance, and testing in order to protect vulnerable populations. In addition, he expanded telehealth options for needed care, such as audio-only telehealth to bridge the digital divide for those without broadband access [16]. In January, 2021, President Biden signed an Executive Order on Ensuring an Equitable Pandemic Response and Recovery, creating a COVID-19 Health Equity Task Force to formulate recommendations for mitigating the health inequities caused by the pandemic and for preventing such inequities in the future. This has so far resulted in 300 recommendations on topics including interpersonal stress linked to racism, addressing the behavioral health consequences of the pandemic in communities of color, and vaccine access and acceptance [17]. In March, 2021, the American Rescue Plan (ARP) lowered health plan premiums in the Marketplaces, and the percent of new enrollees in 2021 that were Black increased by 60% compared to 2019. The ARP also provided $160 billion for COVID-19 vaccines, tests, personal protective equipment, and public health workforce needed to address the spread of COVID-19 [17]. Between November 2020 and February 2021, the willingness for vaccination increased by nine and nineteen percentage points among all Americans and Black Americans, respectively [18], and a recent survey showed gains in equity in vaccination rates [19]. With the expanded vaccine support, more than 75% of people vaccinated at Community Health Centers were people of color [17]. In April 2021, President Biden issued a proclamation addressing disproportionately higher rates of maternal mortality and morbidity among Black women. The Centers for Medicare and Medicaid Services approved several waivers to extend the Medicaid postpartum coverage period, which will become available as a state option starting in 2022 [20]. Finally, the President’s proposed Build Back Better Plan will further lower health care costs, expand coverage to millions of low-income Americans by closing the Medicaid coverage gap, and extend the ARP’s child tax credit expansion, reducing Black poverty by 29% relative to the projected poverty rate for 2022 [17].
More long-range policies will require a deeper understating of disparities. To understand the causes of COVID-19 disparities and to formulate policy solutions, one needs to first examine how racial and ethnic groups actually perceived COVID-19 and access to health care during the pandemic. In this paper, we take a step back from looking at disparities in COVID-19 mortality statistics and develop a different approach to assessing disparities in COVID-19 outcomes. We examine the self-reported perceived risk of COVID-19 outcomes and the perceived lack of access to needed care. Were there racial and ethnic disparities in the fear of catching COVID-19 and then not being able to get treatment, and to what extent? Racial and ethnic discrimination and mistreatment experienced in the healthcare environment has engendered a high level of distrust in the health care system among minorities [1, 5, 21,22,23]. In the presence of such distrust and a higher exposure risk to COVID-19, minorities are likely to differ severely from White people with respect to the perceived risks and consequences of the COVID-19 pandemic.
While three recent surveys (the American Trends Panel survey, the Diffusion of Fear survey, and a survey from the Ipsos Knowledge Panel) have examined race and perceptions of COVID-19 risks, their survey questions were limited to general health concerns, such as the impact of COVID-19 on the “population’s health” [24, 25]. These general measures are difficult to use to parse out disparities in fears of infection, death, hospitalization, and access to care. Thus, here, we examine more detailed questions about perceived risks and health care under COVID-19. We ask, “what were people’s perceived risks of COVID-19 infection, hospitalization, and death during the height of the first wave of the pandemic in 2020, as well as their perceived access to treatment for COVID-19?” To ascertain the magnitude of these potential disparities during the height of the first wave of the pandemic, we used a survey that was fielded across the nation to assess racial and ethnic disparities in people’s risk perceptions of COVID-19 and their access to needed medical care if infected with COVID-19. Here, we report the findings of the Stanford University School of Medicine Coronavirus Attitudes and Behaviors Survey.
Methods
Data Samples
For the actual case rates of COVID-19 outcomes, we use the CDC’s “COVID-19 Case Surveillance Public Use Data with Geography” across 50 states [26], as well as reported state data from Ohio, Illinois, and California [27]. We have 1.42 million confirmed COVID-19 cases in the CDC data from March to June, 2020. This is a 53% subsample with non-missing race and ethnicity for the cases. We use the CDC’s direct method for age-adjusting hospitalization, ICU, and death rates [28]. These rates are reported in Table 1.
For the perceptions of COVID-19 risks, we use the Stanford University School of Medicine Coronavirus Attitudes and Behaviors Survey, a nationally representative survey fielded by Westat in May of 2020. This survey collected information on individuals’ perceived COVID-19 infection risks and infection-related health implications, and changes made in individuals’ activities in response to the pandemic. The survey details, including the survey design and survey questions, are provided in depth in a study coauthored by Stanford University and Westat [29]. An invitation to participate in an online survey was sent to 13,590 randomly selected residential addresses in the USA from the US Postal Service Delivery Sequence File. Within each selected household, an adult individual was selected by randomly including instructions in the invitation letter for the youngest male, oldest male, youngest female or oldest female to complete the survey. Our analytical sample included all 1,222 individuals who completed the survey. The survey includes nonresponse-adjusted weights to make national estimates. The nonresponse-adjusted weights were also adjusted to account for the selection of one adult among the adults in the household. Finally, the adjusted weights were raked to population estimates from the American Community Survey (2018; 1-year tables).
COVID-19 Perception Measures
We used the following eight measures to examine disparities across racial and ethnic groups:
-
1.
Pandemic Will Last Beyond Summer (> = 3 months). We used valid responses to the question “How Long Will the Pandemic Last?” A dummy variable was set to 1 for those who responded that it would last at least 3 months or longer. Otherwise, the variable was set equal to zero.
The following measures were presented to the respondents with these instructions, “Answer these questions with a number from 0 to 100, where “0” means that you think there is absolutely no chance, and “100” means that you think it is absolutely sure to happen. For example, no one can ever be sure about tomorrow’s weather, but if you think that rain is very unlikely tomorrow, you might say that there is a 10 percent chance of rain. If you think there is a very good chance that it will rain tomorrow, you might say that there is an 80 percent chance of rain.”
Thus, we can consider these measures as perceived probabilities:
-
2.
Risk of Catching COVID-19 if Stayed Home (> = 0 and < = 100). All valid responses (on a scale from 0 to 100) to the question “How likely is it that you or someone like you would catch the coronavirus if you stayed at home the vast majority of the time?” were used.
-
3.
Risk of Catching COVID-19 in Public Places (> = 0 and < = 100). We used the mean of individuals’ perceived risk of catching COVID-19 on a scale ranging from 0 to 100 with regard to each of the seven public places (going to the gym, exercising outside, eating at a restaurant, seeing a movie in a theater, using shared transport, going to a grocery store, and going to work outside the home).
-
4.
Importance of Changing Behavior to Protect Family (= 1 if extremely important). For this measure, we used responses to the question “How important was it to change your behavior to protect you and your family?” A dummy variable was set to 1 for those who responded that it was extremely important. Otherwise, for all other valid responses, the variable was set equal to zero.
-
5.
Likelihood of Needing Medical Care if COVID-19-Infected (> = 0 and < = 100). Valid answers to the question “If you or someone like you caught the coronavirus, how likely is it that you would need medical care?” were used.
-
6.
Likelihood of Dying if COVID-19-Infected (> = 0 and < = 100). We used individuals’ reported likelihood (on a scale of 0 to 100) of dying if the respondent or someone like the respondent caught COVID-19.
-
7.
Likelihood of Hospitalization if COVID-19-Infected (> = 0 and < = 100). We used valid reports for the question “If you or someone like you caught the coronavirus, how likely is it that you would need to be hospitalized?”
-
8.
Likelihood that the Hospital will not have Capacity to Treat You if COVID-19-Infected (> = 0 and < = 100). A variable was set equal to the difference between 100 and an individual’s reported likelihood (on a scale from 0 to 100) that the hospital would have the staff and supplies needed for treatment if a respondent or someone like the respondent caught COVID-19.
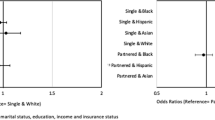
Risk-Adjusting: Health Status and Sociodemographic
Our primary independent variable was a five-category race and ethnicity variable—White non-Hispanic (= 0), Hispanic (= 1), Asian (= 2), Black non-Hispanic (= 3), and Other (= 4). The group “Other” (3%) is not shown in the tables but is included in all regression models. To risk adjust outcomes, we control for the following covariates. Firstly, we include a count variable indicating the number of self-reported diseases (7 possible diseases: hypertension or high blood pressure, diabetes, depression or anxiety, heart disease, respiratory diseases, kidney disease, and auto-immune disease) ever diagnosed by a health care professional. Respondents were divided into three age categories (1 = 18–44 years; 2 = 45–59 years; and 3 = 60 + years old). Dummy variables were used to control for an individual’s family size (0 = one family member, 1 = 2 to 10 family members), marital status, education, income, gender, essential worker status, and residence in a state where the governor or other state official’s stay home or shelter in place orders were in effect. An indicator variable was used to show an individual’s COVID-19 experience—ever tested positive, has COVID-19 symptoms, or had COVID-19 symptoms. We also used a dummy variable to indicate that someone in the respondent’s family or close friends tested positive for COVID-19. Means and frequencies of covariates are displayed in Table 2.
Statistical Analysis
This study used Stata SE 16.1 (Stata Corporation, College Station, TX) to examine disparities in the eight COVID-19 perception measures after risk-adjustments. The analyses used the nonresponse-adjusted survey weights to make national estimates and the Jackknife method to estimate standard errors of estimates. To risk adjust the perception measures for the above covariates, we used logistic regressions for two of the perception measures: perceived duration of the pandemic and importance of changing behaviors to protect self and family. Linear regressions were used to risk-adjust each of the remaining six measures—likelihood of catching COVID-19 at home, catching COVID-19 in public places, needing medical care if infected, dying if infected, hospitalizing if infected, and hospital not having enough capacity to treat if infected. All regressions are displayed in the Supplemental Appendix.
For each measure, the average predicted likelihoods were calculated for each race and ethnic group. Then we examined disparities by comparing the predicted likelihood for White people against each of the three racial and ethnic groups, Asian, Black and Hispanic. We did not show the likelihood of the race “Other” because of small number of people in the group. Due to the large number of comparisons, we made a Bonferroni correction to the standard errors. In addition, to analyze disparities across the entire distribution of the population (and not just at the means), we estimated Lorenz curves by race for the final measure: the perceived likelihood that the hospital would not have enough capacity to treat if infected with COVID-19. Lorenz curves have recently been used to study racial disparities with the COVID-19 vaccines [30]. To create these curves, we used the Lorenz Stata module designed by Jann [30, 31].
Results
In terms of actual aged-adjusted case rates for outcomes of COVID, the national CDC data in Table 1 shows that Black and Asian people had the highest rates of hospitalization after infection. Asian people with COVID-19 had the highest rate of ICU visits. However, White people had the highest rate of death after infections in the CDC data. While this is corroborated in the Ohio state data, Blacks were more likely to die after a COVID-19 infection in the Illinois and California databases.
Table 2 presents nationally representative characteristics of the survey of perceptions of the risks of COVID-19, showing the significant differences between White people and the other racial groups for each characteristic. More than seven-tenths of respondents for each race group lived in states where official stay at home or shelter in place orders were issued. Compared to the other three races and ethnicities, White people had more comorbidities (1.06), a higher proportion (91%) residing in states with stay at home orders, a higher proportion in older age groups (41% in the 60 + year of age group), a lower proportion of “having a family member or a close friend infected with COVID-19” (12%), and a higher proportion living in a single person household (14%). Compared to each of the three other races, Latinx people had a higher proportion in the age group 44 years and younger, a higher proportion “testing positive for COVID-19 or have had symptoms,” a higher proportion having a family member or a close friend who tested COVID-19-positive, a higher proportion with less than a college education, and a higher proportion with household annual income less than $75,000.
Figure 1 presents the adjusted predicted likelihood of belief that the COVID-19 pandemic would end after the Summer of 2020 (e.g., beyond three months). The predicted probability that the pandemic would not be over by the end of Summer ranged from 76.6% among White people to 92.4% among Black people. A significant difference in predicted probability emerged only between Black and White respondents (p < 0.05).
Table 3 presents the regression results of the remaining seven measures. White people had the lowest (53.8%) likelihood of stating that the need to change behavior to protect self and their family was extremely important. Black people had the highest (81.2%) need to change behavior to protect self and their family. Compared to the White population, the predicted level of concern for the family was significantly higher only for Black people (p < 0.05). The perceived likelihood of catching the COVID-19 infection if one stayed the vast majority of the time at home varied across races (20.8% among White people, 18.1% among Latinx people, 14% among Asian people, and 25.2% among Black people), but the perceived likelihood of such for White people differed significantly only from that of Asian people. In contrast, White people were the most optimistic about public places. The perceived probability of catching a COVID-19 infection in public places was lowest in the White population (44.8%), and it was highest in the Latinx population (54.6%) (p < 0.05%, compared to White people). Overall, for all races and ethnicities, the perceived risk of COVID-19 was much higher than the actual risk of COVID-19, which was under 2% at this time [10].
Among the four racial and ethnic groups, White people reported the lowest perceived risk of experiencing negative outcomes (needing medical care, hospitalization, or dying) if infected with COVID-19. The perceived risks of needing medical care if infected with COVID-19 were 51.2%, 63.5%, 56.7%, and 71.1% among the White, Latinx, Asian and Black populations, respectively. These estimates for Latinx people and Black people differed significantly from that of White people (p < 0.05). While the perceived risk of hospitalization if infected in the White population was 41.2%, estimates of both the Latinx and Black population’s perceived risks of hospitalizations were 13 and 17.3 percentage points higher than that of the White population (p < 0.05), respectively. Compared to White people at a perceived 27% risk of dying after COVID-19, the Asian, Latinx and Black populations each perceived a higher likelihood of dying (i.e., at least more than 8 percentage points higher). However, the difference in estimates between White and Latinx people was marginally significant (p < 0.10), and the estimates for the other two races did not differ significantly from that of White people. Overall, for all races and ethnicities, the perceived risk of COVID-19 outcomes once infected were much higher than the actual risks shown in Table 1.
The estimated perceived likelihood of hospitals not having enough capacity to treat if infected with COVID-19 by White, Latinx, Asian and Black populations was 29.2%, 33.1%, 29.4%, and 40.7%, respectively. The estimate for Black people differed significantly from that of White people by 11.5 percentage points (p < 0.05). To see how these disparities varied over the entire population distribution (and not just at the means), we also generated Lorenz curves for the distribution of disparities in the perceived likelihood of hospitals not having enough capacity to treat people if infected with COVID-19, normalized to Black people. We plotted the cumulative likelihood of “hospitals not having enough capacity to treat if infected” on the y-axis and the cumulative proportion of the population for each race on the x-axis. The most optimistic people are on the left side of the x-axis, and the most pessimistic on the right. If all people had the same exact belief, everyone would be on the equitable distribution curve, the straight red line at 450 in Fig. 2. However, curvature of the lines indicates that people within-race have differing beliefs—some optimistic, some pessimistic [31]. Overall, at 100% of the population on the right of the x-axis, we see that in general Black people are more pessimistic. White people expect 24% and 37% fewer untreated COVID-19 cases due to hospital lack of staff and supplies than do Latinx people and Black people, respectively. However, there is also more perception variation within the White population. Black people are more uniform or similar in their beliefs (e.g., the Black population curve is closer to the 45 degree line). White people are more extreme in their range of beliefs. For example, at 40% of the population on the x-axis, the beliefs of the 40% most optimistic Black (White) people account for only 33% (19%) of their race's perceived total expected untreated cases. This is a 42% Black-White difference ((33–19)/33) for the 40% most optimistic people, compared to the 37% Black-White difference at 100%. Thus, even though Black people do have optimistic people, White people have a wider range of optimism within their race than do Black people. That is, White people have more extreme views within their race. Asian people were very similar to White people as well in this respect. Overall, the differences in estimated curves between White people and other races were significant only for Latinx people and Black people, at the 5% significance level.
Discussion
To manage a public health crisis like the one posed by COVID-19, it is important for public health officials to devise policies that engender the needed response from the public. However, the pandemic has revealed a host of racial and ethnic disparities entrenched across the US healthcare system. The magnitude of these disparities could quite easily spiral into greater distrust in the healthcare system for minorities. Policy must be carefully crafted to prevent this escalation and to start mitigating disparities. Effective policy requires a greater understanding of racial and ethnic perceptions of the pandemic and access to care. Perceptions are intuitive evaluations based on experiences, beliefs, attitudes, judgments, (mis)conceptions, and feelings, as well as wider social, cultural, and institutional processes [32]. Perceived risks are important determinants of an individual’s behavioral responses to a situation.
Fortunately, a bola of research on racial perceptions of COVID-19 is beginning to emerge. A recent survey of perceptions administered by Harvard University found age-related disparities in perceived risks of COVID-19: younger people overestimated the risk of death and older people underestimated it [33]. Recent analyses of two surveys found that Latinx and Black people perceived COVID-19 to be a greater risk to both the population’s health and to the individual’s health than perceived by White people [24]. However, White people perceived COVID-19 to be a greater risk to the immune-compromised and elderly than perceived by Non-White people [24]. Liu et al. (2021) recently found in the Understanding America Study, administered by the University of Southern California, that perceived fears of COVID-19 drive the use of more preventive measures (e.g., wearing masks) among Non-White people than among White people [14]. However, such increased preventive measures among Non-White people led to increased minority-perceived racial discrimination against them from White people, causing more mental distress. Thus, policy must be carefully designed to avoid these unintended cycles of discrimination.
In this paper, we add to this new literature by examining the fears and perceptions of health care during COVID-19 in finer detail. Past surveys looked at general fears of COVID-19 on “population health” and “individual health,” with not much clarity on what those terms are perceived to mean. We used nationally representative survey data collected in the early-stages of the COVID-19 pandemic in the USA to assess disparities across eight very specific perceived COVID-19 risks. Based on study results, we reached three conclusions—one for each of the Latinx, Black, and Asian populations. Firstly, Latinx people were the most fearful for the two most critical measures: catching COVID-19 in public and dying once you get COVID-19. This has been corroborated in a survey of six states, where Latinx respondents perceived higher risks of dying of COVID-19 than White and Black respondents [34]. However, both this six-state survey and the Understanding America Study found that Latinx people’s perceived risk of infection was no different than White people’s perceived risk [34, 35]. Our result differs because we split this question into two parts: perceived risk of infection at home and in public. With this distinction, we see that the Latinx population’s perceived risk differs from Whites’ exactly for the fear of catching COVID-19 in public.
Secondly, Black people had the most ubiquitous fears and distrust. They were 10 percentage points more likely than any other race to believe the pandemic would not end within 3 months. And, they rated the need to protect their family from COVID-19 at a level of importance that was 19 percentage points higher than any other race and ethnicity. Black people also had the smallest gap (in percent terms) between the fears of catching COVID-19 in public versus while staying at home. They also had the greatest fear of needing medical care if they caught COVID-19, and, were least likely to believe that the hospital could meet their medical needs due to capacity constraints and lack of staff. Overall, Black people did not have confidence in the “system” working, whether from ending the pandemic, to staying home as being protective, or to delivering the needed hospital care. This paints a much different picture than the Understanding America Study, which found no racial and ethnic differences in the perceived risk of hospitalization if infected with COVID-19 compared to White people [35]. This may be because that survey focused more on political party questions about perceptions of COVID rather than health care access questions.
Thirdly, in contrast to Black people, Asian people had the most confidence in the system. They were more likely than White people to think that staying home was protective of COVID-19, and, had the biggest gap between fears of catching COVID-19 at home versus in public. Ironically, this was the case even though Asian people were the least likely of the races to live in an area with stay at home orders issued by their governor. Moreover, like White people, Asian people were the least likely to think that the hospital could not treat them due to capacity constraints.
In the Supplemental Appendix, of all the respondent characteristics in Table 2, besides race, the number of chronic conditions, income, and education were the strongest predictors of disparities in beliefs about COVID-19. We think that some of the racial and ethnic disparities in perceived risks and distrust found in our study could also be due to a mix of other unobserved socio-economic disparities, the quality of their expected hospital, and the political polarization in the USA. A recent study demonstrated that political beliefs affected risk perceptions in the COVID-19 pandemic resulting in a significant disparity in the reaction of households associated with different political party affiliations [36]. Alesina, Ferroni, and Stantcheva (2021) examined the underlying factors that shape one’s views on remedies for disparities, and found that “it is not the perceived magnitudes of racial gaps but rather their perceived causes that have the highest predictive power. Support for race-targeted policies is strongly correlated with the belief that discrimination and racism are to blame. Support for general redistribution is positively correlated with perceptions of racism and discrimination today, more weakly associated with perceived past slavery and discrimination, and negatively correlated with the belief that Black people are poorer because of lack of effort rather than due to adverse circumstances” [37].
Thus, one must consider a wide spectrum of policies to address these perceived gaps during the pandemic. Orom et al. [25] find that Black and Latinx people respond positively to pro-social policies—that is, “this policy (such as masks) will be good not just for you but for others.” Pro-social policies do not resonant as much with White people [25]. At the other end of the spectrum are bias-reducing educational programs, such as the implicit bias training for healthcare providers proposed in the 2021 Senate Bill S.1234 (The Maternal CARE Act) to help mitigate the racial disparities in maternal mortality and morbidity [38]. Moreover, these policies need to take a long-term approach, especially as we move into a New Normal involving continuous preventive measures (such as masking, which we saw does incite racial discrimination) and where receiving care regularly will be needed for “long” COVID, chronic post-acute symptoms that disproportionately affect Non-Whites patients. While President Biden has been seeking to set up a new $6.5 billion agency called ARPA-Health (or ARPA-H, modeled after the US Defense Advanced Research Projects Agency (DARPA)) to counter new pandemic threats and the long term effects of COVID, and while others envision an ARPA-C to counter climate change, one could also imagine an ARPA-R (R for “racial”) to create countermeasures to mitigate racial and ethnic disparities in access to care during current and future pandemics [39].
Similarly, as the WHO works internationally to improve the surveillance of detecting pathogens, the collection of data, and the scientific development and equitable distribution of therapies and vaccines, there should be increased international efforts to understand the science of racial and ethnic disparities during COVID-19 [40]. The estimated cost of this pandemic is about $22 trillion, with much of that disproportionately borne by Non-Whites [41]. The basic mechanisms of COVID-19 coagulopathy complications, particularly in Black, Latinx, and American Native Indian populations, are not yet fully understood [42, 43]. Future research should jointly explore the biological and socio-economic underpinnings of these disparities and their interactions.
The contribution of our study is that we show that racial disparities in perceptions of COVID-19 extend far beyond the fear of being infected with COVID-19. They extend deep into the healthcare system—fears that they cannot get the needed treatment at their hospital. This has ramifications for the New Normal, where we are shifting from acute treatment to post-acute chronic care treatment especially needed for “long” COVID, chronic post-acute symptoms that disproportionately affect Non-Whites patients. Thus, understanding the New Normal, as highlighted by the WHO, is crucial [44]. Even though COVID-19 has waned, it is not gone. Just as COVID-19 is not gone, the fear of COVID-19 among Non-Whites has also likely not waned. Minorities are still at the frontline of risk as essential workers, public transportation users, and multi-generational household dwellers, all with multiple chronic conditions. These persistent disparities in perceived COVID-19 risks even under the New Normal can take a toll on mental health. More than 28% of Black and Hispanic people reported that the pandemic had a major negative impact on their mental health, compared to 19% of Whites [1].
Limitations
This study has some limitations. Firstly, the survey was conducted online. Thus, it pre-excluded those not having access to the internet, and thereby, its results are applicable to only those having internet access. Secondly, we did not have access to the respondent’s address to control for the COVID-19 rate in their immediate area. However, we do proxy for this by controlling for their own COVID infection and their friends’ and family’s COVID cases. Thirdly, the survey was conducted in the early stages of the pandemic, when even the experts were still trying to understand the virus. With time, one can expect racial perceptions to have had changed.
References
Hamel L, Lopes L, Munana C, Artiga S, Brodie M. KFF/the undefeated survey on race and health. The Henry J. Kaiser Family foundation; 2020. https://www.kff.org/racial-equity-and-health-policy/report/kff-the-undefeated-survey-on-race-and-health/. Accessed 11 Nov 2021.
Marrett CB. Racial disparities and COVID-19: the social context. J Racial Ethn Health Disparities. 2021;8:794–7.
Ndugga N, Artiga S. Disparities in health and health care: 5 key questions and answers. The Henry J Kiaiser Family Foundation; 2021. https://www.kff.org/racial-equity-and-health-policy/issue-brief/disparities-in-health-and-health-care-5-key-question-and-answers/view/footnotes/. Accessed 11 Nov 2021.
Williams DR, Cooper LA. COVID-19 and health equity—a new kind of “Herd Immunity.” JAMA. 2020;323(24):2478–80.
Carter RT. Racism and psychological and emotional injury: recognizing and assessing race-based traumatic stress. Couns Psychol. 2007;35(1):13–105. https://doi.org/10.1177/0011000006292033.
Selden TM, Berdahl TA. COVID-19 and racial/ethnic disparities in health risk, employment, and household composition. Health Aff. 2020;39(9):1624–32.
Laurencin CT, McClinton A. The COVID-19 pandemic: a call to action to identify and address racial and ethnic disparities. J Racial Ethn Health Disparities. 2020;7:398–402.
Laurencin CT, Wu ZH, McClinton A, Grady JJ, Walker JM. Excess deaths among Blacks and Latinx compared with whites during COVID-19. J Racial Ethn Health Disparities. 2021;8:783–9.
Poteat T, Millett GA, Nelson LRE, Beyrer C. Understanding COVID-19 risks and vulnerabilities among black communities in America: the lethal force of syndemic. Ann Epidemol. 2020;47:1–3.
Zelner J, Trangucci R, Naraharisetti R, Cao A, Malosh R, Broen K, Masters N, Delamater P. Racial disparities in Coronavirus Disease 2019 (COVID-19) mortality are driven by unequal infection risks. Clin Infect Dis. 2021;72:e88–95.
Benitez JA, Courtemanche CJ, Yelowitz A. Racial and ethnic disparities in COVID-19: evidence from six large cities. NBER Working Paper No. 27592; 2020.
Price-Haywood EG, Burton J, Fort D, Seoane L. Hospitalization and Mortality among Black Patients and White Patients with Covid-19. New England J Med. 2020;382:26.
Muñoz-Price LS, Nattinger AB, Rivera F, et al. Racial disparities in incidence and outcomes among patients with COVID-19. JAMA Netw Open. 2020;3(9):e2021892.
Bambino Geno Tai D, Sia IG, Doubeni CA, Wieland ML. Disproportionate impact of COVID-19 on racial and ethnic minority groups in the United States: a 2021 update. J Racial Ethn Health Disparities. 2021. https://doi.org/10.1007/s40615-021-01170-w.
Berwick D. Choices for the “new normal.” JAMA. 2020;323(21):2125–6.
HHS Initiatives to Address the Disparate Impact of COVID-19 on African Americans and Other Racial and Ethnic Minorities. https://www.hhs.gov/sites/default/files/hhs-fact-sheet-addressing-disparities-in-covid-19-impact-on-minorities.pdf. Accessed 11 Nov 2021.
White House. Fact Sheet: The Biden-Harris Administration Advances Equity and Opportunity for Black People and Communities Across the Country. October 19, 2021. https://www.whitehouse.gov/briefing-room/statements-releases/2021/10/19/fact-sheet-the-biden-harris-administration-advances-equity-and-opportunity-for-black-people-and-communities-across-the-country/
Dean C, Parker K. Gramlich J. A Year of U.S. Public Opinion on the Corona Virus Pandemic. 2021. Pew Research. https://www.pewresearch.org/2021/03/05/a-year-of-u-s-public-opinion-on-the-coronavirus-pandemic/. Accessed 11 Nov 2021.
Ndugga N, Hill L, Artiga S, Haldar S. Latest Data on COVID-19 Vaccinations by Race/Ethnicity. October 26, 2021. Kaiser Family Foundation. https://www.kff.org/coronavirus-covid-19/issue-brief/latest-data-on-covid-19-vaccinations-by-race. Accessed 11 Nov 2021.
Ndugga N., Artiga S. Disparities in Health and Health Care: 5 Key Questions and Answers. May 11, 2021. https://www.kff.org/racial-equity-and-health-policy/issue-brief/disparities-in-health-and-health-care-5-key-question-and-answers/. Accessed 11 Nov 2021.
Alsan M, Wanamaker M. Tuskegee and the health of Black Men. Q J Econ. 2018;133(1):407–55.
Alsan M, Garrick O, Graziani G. Does diversity matter for health? Experimental evidence from Oakland. Am Econ Rev. 2019;109(12):4071–111.
Alsan M, Stantcheva S, Yang D, Cutler D. Disparities in Coronavirus 2019 reported incidence, knowledge and behavior among US adults. JAMA Netw Open. 2020;3(6):e2012403. https://doi.org/10.1001/jamanetworkopen.2020.12403.
Niño M, Harris C, Drawve G, Fitzpatrick KM. Race and ethnicity, gender, and age on perceived threats and fear of COVID-19: evidence from two national data sources. SSM Popul Health. 2021;13: 100717. https://doi.org/10.1016/j.ssmph.2020.100717.
Orom H, Allard N, Kiviniemi M, Hay J, et al. Racial/ethnic differences in prosocial beliefs and prevention behavior during the COVID-19 pandemic. J Racial Ethn Health Disparities. 2021. https://doi.org/10.1007/s40615-021-01117-1.
CDC COVID-19 Case Surveillance Public Use Data with Geography. August 24, 2021. https://data.cdc.gov/Case-Surveillance/COVID-19-Case-Surveillance-Public-Use-Data-with-Ge/n8mc-b4w4. Accessed 11 Nov 2021.
Pathak I, Choi Y, Jiao D, Yeung D, Liu L. Racial-ethnic disparities in case fatality ratio narrowed after age standardization: A call for race-ethnicity-specific age distributions in State COVID-19 data. MedRxiv. Preprint. 2020. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7536886/. Accessed 11 Nov 2021.
Curtin LR, Klien RJ. Direct Standardization (Age-Adjusted Death Rates). CDC Healthy People 2000, Number 6 (revised), 1995.
Bundorf K, DeMatteis J, Miller G, Polyakova M, Streeter J, Wivagg J. Risk perceptions and protective behaviors: evidence from COVID-19 pandemic NBER working paper No. 28741, 2021.
Jann B. Estimating Lorenz and concentration curves. Stata J. 2016;16:837–66.
Mody A, Pfeifauf K, Geng EH. Using Lorenz curves to measure racial inequities in COVID-19 testing. JAMA Netw Open. 2021;4(1):1–4.
Cori L, Bianchi F, Cadum E, Anthonj C. Risk perceptions and COVID-19. Int J Environ Res Public Health. 2020;17(9):3114.
Bordalo P, KB Coffman, N Gennaioli, A Shleifer. Older People are Less Pessimistic about the Health Risks of COVID-19. NBER Working Paper 27494. Cambridge, MA, July, 2020.
Dickinson KL, Roberts JD, Banacos N, Neuberger L, Koebele E, Blanch Hartigan D, Shanahan EA. Structural racism and the covid-19 experience in the united states. Health Security, 19(S1), 2021. https://doi.org/10.1089/hs.2021.0031
Bruine de Bruin W, Saw HW, Goldman DP. Political polarization in US residents' COVID-19 risk perceptions, policy preferences, and protective behaviors. J Risk Uncertain. 2020:1–18; https://doi.org/10.1007/s11166-020-09336-3
Barrios JM, Hochberg Y. Risk Perception Through the Lens of Politics in the Time of the COVID-19 Pandemic. NBER Working Paper No. 27008 April 2020.
Alesina A, Ferroni MF, Stantcheva S. Perceptions of racial gaps, their causes, and ways to reduce them. Cambridge: National Bureau of Economic Research; 2021.
US Senate. Bill S. 1234 The Maternal CARE Act. https://www.congress.gov/bill/117th-congress/senate-bill/1234/text?q=%7B%22search%22%3A%5B%22Maternal+CARE+Act%22%5D%7D&r=1&s=3. Accessed 11 Nov 2021
Dyani Lewis. Long COVID and kids: scientists race to find answers. Nature. July 14, 2021. https://www.nature.com/articles/d41586-021-01935-7. Accessed 11 Nov 2021.
Maxmen A. Has COVID taught us anything about pandemic preparedness. Nature. 2020;596:332–5.
Dobson AP, Pimm SL, Hannan L, Kaufman L, Ahumada JA, Ando AW, Bernstein A, Busch J, Daszak P, Engelmann J, Kinnaird MF, Li BV, Loch-Temselides T, Lovejoy T, Nowak K, Roehrdanz PR, Vale MM. Ecology and economics for pandemic prevention. Science. 2020;369(6502):379–81.
Chaudhary R, Bliden KP, Kreutz RP, Jeong Y, Tantry US, Levy JH, Gurbel PA. Race-Related disparities in COVID-19 thrombotic outcomes: Beyond social and economic explanations. EClinicalMedicine. 2020;29–30(2020): 100647. https://doi.org/10.1016/j.eclinm.2020.100647.
Esenwa C, Unda SR, Altschul DJ, et al. The effect of race on composite thrombotic events in patients with COVID-19. Thromb Res. 2021;199(2021):10–3.
World Health Organization. COVID-19: New Normal. https://www.who.int/westernpacific/emergencies/covid-19/information/covid-19-new-normal. Accessed 11 Nov 2021.
Acknowledgements
The views expressed in this article are those of the authors, and no official endorsement by the US Department of Health and Human Services, the AHRQ, or Westat is intended or should be inferred.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
This article used the de-identified public use file, and so does not contain any studies with human participants or animals performed by any of the authors.
Informed Consent
Not applicable.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kumar, V., Encinosa, W. Racial Disparities in the Perceived Risk of COVID-19 and in Getting Needed Medical Care. J. Racial and Ethnic Health Disparities 10, 4–13 (2023). https://doi.org/10.1007/s40615-021-01191-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40615-021-01191-5