Abstract
Purpose
Antidepressant medications are commonly prescribed for the treatment of depression, anxiety, and chronic pain. Their use may lead to a number of side effects with important implications in the perioperative period. Our aim was to examine the effect of preoperative antidepressant administration on post-surgical hospital length of stay (LOS) in elective non-cardiac surgery patients.
Design
Historical cohort study.
Methods
Demographic and preoperative data were collected by chart review for all non-cardiac surgery patients who were assessed in the preoperative consult clinic from April 2008 through February 2009. Patients were grouped according to whether or not they were taking antidepressant medications. Median length of stay was compared between patients who took antidepressants preoperatively and those who did not.
Results
Data were collected for 3,692 patients. Two hundred eighty-nine (7.8%) patients were taking antidepressants preoperatively. Use of antidepressants was not associated with an increased hospital LOS. The median LOS was four days both for patients who took antidepressants preoperatively (95% confidence interval [CI] 4 to 4) and for those who did not (95% CI 3 to 5) (P = 0.13).
Conclusions
The preoperative use of antidepressant medications was not associated with increased postoperative hospital LOS following elective non-cardiac surgery.
Résumé
Objectif
Les antidépresseurs sont couramment prescrits pour le traitement de la dépression, de l’anxiété et de la douleur chronique. Leur utilisation peut entraîner plusieurs effets secondaires ayant des implications importantes pour la période périopératoire. Notre objectif était d’examiner l’effet de l’administration préopératoire d’antidépresseurs sur la durée de séjour hospitalier (DSH) postchirurgical de patients ayant subi une chirurgie non cardiaque non urgente.
Méthodologie
Étude de cohorte historique.
Méthode
Les données démographiques et préopératoires ont été colligées en passant en revue les dossiers de tous les patients de chirurgie non cardiaque évalués en clinique préopératoire entre avril 2008 et février 2009. Les patients ont été regroupés en fonction de leur consommation ou non d’antidépresseurs. La durée moyenne de séjour a été comparée entre les patients prenant des antidépresseurs avant l’opération et ceux n’en prenant pas.
Résultats
Au total, des données ont été recueillies à propos de 3 692 patients. Deux cent quatre-vingt-neuf (7,8 %) patients prenaient des antidépresseurs avant leur opération. L’utilisation d’antidépresseurs n’a pas été associée à une DSH accrue. La DSH était de quatre jours pour les patients prenant des antidépresseurs en préopératoire (intervalle de confiance [IC] 95 % 4 à 4) et pour les patients n’en prenant pas (IC 95 % 3 à 5) (P = 0,13).
Conclusion
L’utilisation préopératoire de médicaments antidépresseurs n’a pas été associée à une DSH postopératoire prolongée après une chirurgie non cardiaque non urgente.
Similar content being viewed by others
Antidepressants modify neurotransmitters in the central nervous system (CNS) in order to alleviate the symptoms of depression. Additionally, they are now often prescribed for both anxiety disorders and chronic pain.1-3 Tricyclic antidepressants (TCAs) act as serotonin-norepinephrine reuptake inhibitors in the CNS.4 These include amitriptyline, clomipramine, desipramine, doxepin, imipramine, and nortriptyline.5 Monamine oxidase inhibitors (MAOIs) inhibit the activity of monamine oxidases and therefore prevent the degradation of monoamine neurotransmitters in the CNS, including serotonin, melatonin, epinephrine, dopamine, and norepinephrine.6 Monamine oxidase inhibitors include isocarboxazid, phenelzine, and tranylcypromine. Selective serotonin reuptake inhibitors (SSRIs), as the name suggests, inhibit the reuptake of serotonin at the post-synaptic cleft. Selective serotonin reuptake inhibitors include citalopram, escitalopram, fluoxetine, fluvoxamine, paroxetine, and sertraline. Bupropion inhibits the reuptake of both norepinephrine and dopamine in the CNS.7,8 Serotonin-norepinephrine reuptake inhibitors (SNRIs) include duloxetine, venlafaxine, and desvenlafaxine.9
Although TCAs have fallen out of favour as a treatment for depression, it is important to point out that many patients are prescribed these medications for chronic pain, typically at lower doses than those used for the treatment of depression.10 Amitriptyline at low doses (25-50 mg at bedtime vs 150-300 mg for depression) has been shown to be effective in treating chronic pain and is considered first-line therapy for the treatment of the symptoms of fibromyalgia.11 Nortriptyline (75 mg daily vs 150 mg daily for depression) has been used to treat neuropathic and myofascial pain.12 Newer antidepressants of the SNRI family, duloxetine and venlafaxine, have also been used to treat chronic pain, particularly in patients whose primary complaint is fatigue as these drugs are less sedating than TCAs.13,14 In contrast to TCAs, the optimal dose of duloxetine for the treatment of both chronic pain and depression is 60 mg daily.13 Similarly, venlafaxine is prescribed to patients in the range of 75-225 mg daily for both chronic pain and depression.14
Use of antidepressants may lead to a number of side effects with important implications in the perioperative period. Antidepressants may have significant drug-drug interactions, resulting in altered activity or metabolism of anesthetic medication; therefore, interactions should be checked prior to administration. Tricyclic antidepressants can cause cardiac dysrhythmias and are considered cardiotoxic, so drugs that result in QTc prolongation, such as ondansetron, should be avoided.5 The reuptake of vasoactive agents, such as epinephrine and norepinephrine, is inhibited by TCAs; consequently, their action may be amplified or prolonged.5 Ephedrine administered to a patient on an MAOI may result in a hypertensive crisis.15 Patients on an SSRI or SNRI who are administered meperidine or tramadol are at risk of developing serotonin syndrome.5
Both TCAs and MAOIs can cause orthostatic hypotension that may result in hemodynamic instability on induction.5 Furthermore, TCAs have anticholinergic effects that may cause tachycardia.5 Selective serotonin reuptake inhibitors have been associated with an increased risk of spontaneous bleeding. This is thought to be a result of decreased intra-platelet levels of serotonin, a required substrate for platelet aggregation.16,17 The use of SSRIs has been associated with increased rates of transfusion in orthopedic surgery.18
In addition to the risk of drug-drug interactions, antidepressants are associated with weight gain and the development of diabetes mellitus, thus, patients on antidepressants are at increased risk of metabolic syndrome and its attendant anesthetic considerations.19,20
A number of studies have examined the effects of depression on outcome and pain following surgery in orthopedic, oral surgery, and cardiac surgery populations.21-24 Fewer studies have examined the effects from using antidepressants, no matter the clinical indication, and outcome following surgery. A number of studies have examined the effects of SSRIs on hemodynamics and bleeding in orthopedic patients.18,25,26 Another study examined the association between increased postoperative pain and the use of antidepressants in patients undergoing major abdominal surgery.27 In this study, we examine the association between the use of antidepressants and postoperative outcome measured as hospital length of stay in all non-cardiac patients. We chose hospital length of stay as a marker of postoperative outcome as specific adverse outcomes, such as hemorrhage, dysrhythmias, and myocardial infarction, are uncommon following surgery but result in increased stay in hospital. Thus, hospital length of stay is used as a surrogate marker for adverse outcomes following surgery.
Our aim was to determine if there was an association between use of antidepressants and hospital length of stay in non-cardiac surgery patients. We hypothesized that patients taking antidepressants would have longer hospital length of stay than patients who were not taking antidepressants.
Methods
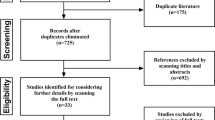
This study was approved by the Research Ethics Board of the University Health Network in January 2009. All non-cardiac surgery inpatients being assessed in the anesthesia preoperative clinic were screened for inclusion in the study. In addition, all patients assessed in the pre-admission units of the University Health Network (UHN) from implementation of the Clinical Anesthesia Information System (CAIS) in April 2008 through February 2009 were included for analysis. Patients being admitted through the emergency department for emergent or urgent surgery were excluded as these patients do not undergo standard preoperative assessment. Patients were grouped according to whether or not they were taking antidepressants before their surgery. Patients were categorized as antidepressant users if they were recorded as taking a drug that is classified as an antidepressant in the CAIS database (Table 2).
Preoperative data were collected from our CAIS (Adjuvant Informatics, Freelton, ON, Canada). The CAIS is a standardized Web-based preoperative assessment tool developed by the UHN to evaluate all elective surgical patients. Advanced practice nurses entered patient information into CAIS for all elective patients at their pre-admission unit appointment. The CAIS collects information using standardized branched logic. The collected data include patient demographics, vital signs, detailed history, preoperative lab values, and full medication history. Postoperative data were collected from the UHN Enterprise Data Warehouse (EDW); the data included information relating to the surgical procedure as well as postoperative patient outcomes and hospital length of stay. The outcome data obtained from the EDW is largely obtained from International Classification of Disease 10th revision (ICD-10) codes. Age, sex, American Society of Anesthesiologists (ASA) score, date of hospital admission, date of surgery, date of hospital discharge, type of surgery performed, and preoperative antidepressant medications were extracted from the databases.
No a priori sample size calculation was made. The sample size was based on all patients assessed within the study period (April 2008 - February 2009). Hospital length of stay (in days) was not normally distributed, so the median postoperative hospital length of stay was compared between groups by the Mann-Whitney U test. Demographic data (age, sex, ASA score) were collected in order to ensure there were no significant differences in demographics between the two groups. Results were reported as mean (SD), median with 95% confidence intervals (CI), or frequency (percent) unless otherwise indicated. Data were analyzed using SPSS® 22.0 for Mac (IBM SPSS Statistics, 2013).
Results
Data were collected for 3,692 non-cardiac surgery patients. Demographic data for the cohort are shown in Table 1. Two hundred eighty-nine (7.8%) patients were on antidepressants preoperatively (Table 2). The antidepressants most commonly taken in the cohort were citalopram, venlafaxine, and amitriptyline (Table 2). Some patients took more than one antidepressant. In the group of patients taking antidepressants, the proportion of females was significantly higher (Table 1) (P = 1 × 10−6); 10.5% of female patients in the cohort were taking antidepressants preoperatively, while only 5.1% of male patients were taking antidepressants.
Hospital length of stay was not normally distributed. The median hospital length of stay after surgery for all patients was 4.0 days (95% CI 4 to 4). The median length of stay was 4.0 days both for patients taking antidepressants (95% CI 4 to 4) and for patients not taking antidepressants preoperatively (95% CI 3 to 5) (P = 0.13).
The median length of stay for females after surgery was 4.0 days (95% CI 4 to 4), while the median length of stay for male patients after surgery was 3.0 days (95% CI 3 to 4) (P = 0.005). As there were significantly more females than males using antidepressants preoperatively and the median hospital length of stay was found to be different for females and males, a post hoc analysis of antidepressant use and hospital length of stay stratified by sex was performed.
When stratified by sex, antidepressant use was still not found to be associated with hospital length of stay. Median hospital length of stay was 4.0 days (95% CI 4 to 5) for female patients taking antidepressants vs 4.0 days (95% CI 4 to 4) for female patients who were not taking antidepressants preoperatively (P = 0.39). Median hospital length of stay was 3.0 days (95% CI 3 to 5) for male patients taking antidepressants vs 3.0 days (95% CI 3 to 4) for male patients who were not taking antidepressants preoperatively (P = 0.34).
Discussion
In this retrospective study, we found that use of antidepressants was not associated with post-surgical hospital length of stay. Rates of antidepressant use were different in males and females, but even when stratified by sex, antidepressant use was not associated with increased hospital length of stay.
In 2005, a national study of patterns of antidepressant use in the United States showed that over 10% of the population were being treated with antidepressants for various indications.28 This was similar to the proportion of our patients (7.8%) who were on antidepressants and suggests that a large proportion of the patients we care for in the operating room will be treated with antidepressants. It is therefore important to examine the effect of antidepressants on postoperative outcome.
In this study, we examined the association between antidepressant use and recovery from all types of surgery performed at a major tertiary care hospital. Preoperative depression is a well-known risk factor for postoperative mortality and morbidity in surgical patients.21-24 Furthermore, antidepressants are known to cause specific adverse perioperative events, such as increased bleeding;16-18 however, there is a lack of studies examining whether antidepressants lead to prolonged postoperative length of stay in hospital. Additionally, the role of depression vs the possible effect of antidepressants on postoperative outcomes has not been well evaluated. In the future, it will be important to compare specific groups of patients with depression, for example, those successfully treated with antidepressants vs those resistant to treatment with antidepressants vs those with untreated depression, in order to assess differences in recovery trajectories following surgery. These patients should be further compared with patients who are on antidepressants for clinical indications other than depression.
Strengths of our study were the large size of our cohort and the fact that patients in both groups were similar with regard to age and ASA score, two factors that could influence length of stay. The two groups were not similar, however, with respect to sex distribution, and female sex was associated with an increased median hospital length of stay. Nevertheless, post hoc stratification of the cohort by sex indicated that use of antidepressants was still not associated with increased hospital length of stay. An additional strength of our study was inclusion of all patients who were assessed in the preoperative clinics of the UHN (Toronto General Hospital, Princess Margaret Hospital, and Toronto Western Hospital), so no selection bias was introduced into the cohort. We were able to include all patients who were seen in the preoperative clinics of the UHN as a result of the comprehensive data collected in our well-developed electronic preoperative assessment system (CAIS).
There were several limitations to our study. This was a secondary analysis of administrative data, and information is lacking regarding preoperative depression and precise indications for preoperative use of antidepressants. It is noteworthy that the most frequently prescribed medications were amitriptyline, duloxetine, and venlafaxine, all of which are indicated for chronic pain, although we were not able to differentiate between use of antidepressants for depression vs use for chronic pain in this study. In future assessments of patients in the pre-admission units, it will be important to note the specific indication for which antidepressants are prescribed. This analysis was limited to comparing outcomes in patients on antidepressants with patients who were not on antidepressants, and we did not have a measure of patients’ mood, anxiety, or chronic pain at the time of surgery. By preoperatively administering prospective depression scores to patients, a greater difference in outcome may be found between patients who are not depressed and patients with untreated depression. Given that this is an association study, one of the weaknesses of our work is that causality cannot be determined.
In conclusion, preoperative use of antidepressants was not associated with increased hospital length of stay in elective patients undergoing non-cardiac surgery.
References
Bereza BG, Machado M, Ravindran AV, Einarson TR. Evidence-based review of clinical outcomes of guideline-recommended pharmacotherapies for generalized anxiety disorder. Can J Psychiatry 2012; 57: 470-8.
Moore RA, Derry S, Aldington D, Cole P, Wiffen PJ. Amitriptyline for neuropathic pain and fibromyalgia in adults. Cochrane Database Syst Rev 2012; 12: CD008242.
Pergolizzi JV Jr, Raffa RB, Taylor R Jr, Rodriguez G, Nalamachu S, Langley P. A review of duloxetine 60 mg once-daily dosing for the management of diabetic peripheral neuropathic pain, fibromyalgia, and chronic musculoskeletal pain due to chronic osteoarthritis pain and low back pain. Pain Pract 2013; 13: 239-52.
Tatsumi M, Groshan K, Blakely RD, Richelson E. Pharmacological profile of antidepressants and related compounds at human monoamine transporters. Eur J Pharmacol 1997; 340: 249-58.
Nelson JC. Tricyclic and tetracyclic drugs. In: Schatzberg AF, Nemeroff CB, editors. The American Psychiatric Publishing Textbook of Psychopharmacology. 4th ed. Washington, DC: American Psychiatric Publishing; 2009 .
Liebowitz MR, Hollander E, Schneier F, et al. Reversible and irreversible monoamine oxidase inhibitors in other psychiatric disorders. Acta Psychiatr Scand Suppl 1990; 360: 29-34.
Slemmer JE, Martin BR, Damaj MI. Bupropion is a nicotinic antagonist. J Pharmacol Exp Ther 2000; 295: 321-7.
Terry P, Katz JL. Dopaminergic mediation of the discriminative stimulus effects of bupropion in rats. Psychopharmacology (Berl) 1997; 134: 201-12.
Deecher DC, Beyer CE, Johnston G, et al. Desvenlafaxine succinate: a new serotonin and norepinephrine reuptake inhibitor. J Pharmacol Exp Ther 2006; 318: 657-65.
Pilowsky I, Hallett EC, Bassett DL, Thomas PG, Penhall RK. A controlled study of amitriptyline in the treatment of chronic pain. Pain 1982; 14: 169-79.
O’Malley PG, Balden E, Tomkins G, Santoro J, Kroenke K, Jackson JL. Treatment of fibromyalgia with antidepressants: a meta-analysis. J Gen Intern Med 2000; 15: 659-66.
Watson CP, Vernich L, Chipman M, Reed K. Nortriptyline versus amitriptyline in postherpetic neuralgia: a randomized trial. Neurology 1998; 51: 1166-71.
Arnold LM, Rosen A, Pritchett YL, et al. A randomized, double-blind, placebo-controlled trial of duloxetine in the treatment of women with fibromyalgia with or without major depressive disorder. Pain 2005; 119: 5-15.
Sayar K, Aksu G, Ak I, Tosun M. Venlafaxine treatment of fibromyalgia. Ann Pharmacother 2003; 37: 1561-5.
Goldberg LI. Monoamine oxidase inhibitors. Adverse reactions and possible mechanisms. JAMA 1964; 190: 456-62.
Hergovich N, Aigner M, Eichler HG, Entlicher J, Drucker C, Jilma B. Paroxetine decreases platelet serotonin storage and platelet function in human beings. Clin Pharmacol Ther 2000; 68: 435-42.
Nair GV, Gurbel PA, O’Connor CM, Gattis WA, Murugesan SR, Serebruany VL. Depression, coronary events, platelet inhibition, and serotonin reuptake inhibitors. Am J Cardiol 1999; 84: 321-3.
Movig KL, Janssen MW, de Waal Malefijt J, Kabel PJ, Leufkens HG, Egberts AC. Relationship of serotonergic antidepressants and need for blood transfusion in orthopedic surgical patients. Arch Intern Med 2003; 163: 2354-8.
Andersohn F, Schade R, Suissa S, Garbe E. Long-term use of antidepressants for depressive disorders and the risk of diabetes mellitus. Am J Psychiatry 2009; 166: 591-8.
Gartlehner G, Gaynes BN, Hansen RA, et al. Comparative benefits and harms of second-generation antidepressants: background paper for the American College of Physicians. Ann Intern Med 2008; 149: 734-50.
Feeney SL. The relationship between pain and negative affect in older adults: anxiety as a predictor of pain. J Anxiety Disord 2004; 18: 733-44.
Perski A, Feleke E, Anderson G, et al. Emotional distress before coronary bypass grafting limits the benefits of surgery. Am Heart J 1998; 136: 510-7.
Thomas V, Heath M, Rose D, Flory P. Psychological characteristics and the effectiveness of patient-controlled analgesia. Br J Anaesth 1995; 74: 271-6.
Vickers ER, Boocock H, Harris RD, et al. Analysis of the acute postoperative pain experience following oral surgery: identification of ‘unaffected’, ‘disabled’ and ‘depressed, anxious and disabled’ patient clusters. Aust Dent J 2006; 51: 69-77.
Kudoh A, Katagai H, Takazawa T. Antidepressant treatment for chronic depressed patients should not be discontinued prior to anesthesia. Can J Anesth 2002; 49: 132-6.
van Haelst IM, van Klei WA, Doodeman HJ, Kalkman CJ, Egberts TC. Selective serotonin reuptake inhibitors and intraoperative blood pressure. Am J Hypertens 2012; 25: 223-8.
Kudoh A, Katagai H, Takazawa T. Increased postoperative pain scores in chronic depression patients who take antidepressants. J Clin Anesth 2002; 14: 421-5.
Marcus SC, Olfson M. National trends in the treatment for depression from 1998 to 2007. Arch Gen Psychiatry 2010; 67: 1265-73.
Funding sources
R. Fraser Elliott Chair, University Health Network.
Competing interests
None declared.
Author information
Authors and Affiliations
Corresponding author
Additional information
Author contributions
Ainsley Sutherland, Rita Katznelson, Gordon Tait, and W. Scott Beattie developed the research protocol. Ainsley Sutherland analyzed the data collected from the database, performed a background literature search, and wrote the first draft of the paper. Rita Katznelson, Hance A. Clarke, and W. Scott Beattie reviewed and revised the manuscript. Gordon Tait and W. Scott Beattie developed the database for clinical data collection.
Rights and permissions
About this article
Cite this article
Sutherland, A.M., Katznelson, R., Clarke, H.A. et al. Use of preoperative antidepressants is not associated with postoperative hospital length of stay. Can J Anesth/J Can Anesth 61, 27–31 (2014). https://doi.org/10.1007/s12630-013-0062-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-013-0062-0