Abstract
Introduction
This analysis of pooled data from four randomized, controlled-dose adjustment, phase 3 studies (three 15-week, double-blind, placebo- and active-controlled studies and a 1-year, open-label, active-controlled safety study) in patients with chronic osteoarthritis hip or knee pain or low back pain evaluated the safety and tolerability of tapentadol extended release (ER) for the management of moderate to severe, chronic pain.
Methods
In the three 15-week studies, patients were randomized (1:1:1) to twice-daily (bid) doses of placebo, tapentadol ER (100–250 mg), or oxycodone hydrochloride (HCl) controlled release (CR; 20–50 mg). In the 1-year safety study, patients were randomized (4:1) to tapentadol ER (100–250 mg bid) or oxycodone HCl CR (20–50 mg bid). Adverse events (AEs) and discontinuations were recorded in each study; pooled results were analyzed by treatment group.
Results
In the placebo (n = 993), tapentadol ER (n = 1,874), and oxycodone CR (n = 1,224) groups, respectively, 40.7%, 48.4%, and 62.3% of patients discontinued treatment prematurely and 58.7%, 79.0%, and 86.6% of patients experienced ≥1 treatment-emergent AE (TEAE). Incidences of gastrointestinal TEAEs in the placebo, tapentadol ER, and oxycodone CR groups, respectively, were 26.6%, 47.3%, and 65.4%; incidences of nervous system TEAEs were 22.5%, 42.6%, and 45.1%, respectively. Moderate or severe gastrointestinal TEAEs were reported for 10.9% of patients who received placebo, 25.3% of patients who received tapentadol ER, and 42.3% of patients who received oxycodone CR, and moderate or severe nervous system TEAEs were reported for 10.6%, 22.1%, and 25.2% of patients, respectively. In the placebo, tapentadol ER, and oxycodone CR groups, respectively, incidences of gastrointestinal TEAEs leading to study discontinuation were 2.1%, 8.3%, and 24.1%; incidences of nervous system TEAEs leading to discontinuation were 1.4%, 7.9%, and 16.3%, respectively.
Conclusion
Results from this large patient population showed that tapentadol ER (100–250 mg bid) had improved gastrointestinal tolerability compared with oxycodone CR, based on the overall incidence of gastrointestinal TEAEs, the incidence of moderate or severe gastrointestinal TEAEs, and the incidence of gastrointestinal TEAEs leading to discontinuation.





Similar content being viewed by others
References
Johannes CB, Le TK, Zhou X, Johnston JA, Dworkin RH. The prevalence of chronic pain in United States adults: results of an internet-based survey. J Pain. 2010;11:1230–9.
Reid KJ, Harker J, Bala MM, et al. Epidemiology of chronic non-cancer pain in Europe: narrative review of prevalence, pain treatments and pain impact. Curr Med Res Opin. 2011;27:449–62.
Katz WA, Barkin RL. Dilemmas in chronic/persistent pain management. Am J Ther. 2008;15:256–64.
Breivik H, Collett B, Ventafridda V, Cohen R, Gallacher D. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain. 2006;10:287–333.
Avouac J, Gossec L, Dougados M. Efficacy and safety of opioids for osteoarthritis: a meta-analysis of randomized controlled trials. Osteoarthr Cartil. 2007;15:957–65.
Furlan AD, Sandoval JA, Mailis-Gagnon A, Tunks E. Opioids for chronic noncancer pain: a meta-analysis of effectiveness and side effects. CMAJ. 2006;174:1589–94.
Kalso E, Edwards JE, Moore RA, McQuay HJ. Opioids in chronic non-cancer pain: systematic review of efficacy and safety. Pain. 2004;112:372–80.
Chou R, Ballantyne JC, Fanciullo GJ, Fine PG, Miaskowski C. Research gaps on use of opioids for chronic noncancer pain: findings from a review of the evidence for an American Pain Society and American Academy of Pain Medicine clinical practice guideline. J Pain. 2009;10:147–59.
Martell BA, O’Connor PG, Kerns RD, et al. Systematic review: opioid treatment for chronic back pain: prevalence, efficacy, and association with addiction. Ann Intern Med. 2007;146:116–27.
Trescot AM, Helm S, Hansen H, et al. Opioids in the management of chronic non-cancer pain: an update of American Society of the Interventional Pain Physicians’ (ASIPP) Guidelines. Pain Physician. 2008;11:S5–62.
McNicol E, Horowicz-Mehler N, Fisk RA, et al. Management of opioid side effects in cancer-related and chronic noncancer pain: a systematic review. J Pain. 2003;4:231–56.
Christo PJ. Opioid effectiveness and side effects in chronic pain. Anesthesiol Clin N Am. 2003;21:699–713.
Moore RA, McQuay HJ. Prevalence of opioid adverse events in chronic non-malignant pain: systematic review of randomised trials of oral opioids. Arthritis Res Ther. 2005;7:R1046–51.
Trescot AM, Glaser SE, Hansen H, Benyamin R, Patel S, Manchikanti L. Effectiveness of opioids in the treatment of chronic non-cancer pain. Pain Physician. 2008;11:S181–200.
Benyamin R, Trescot AM, Datta S, et al. Opioid complications and side effects. Pain Physician. 2008;11:S105–20.
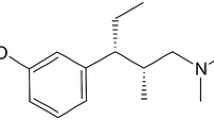
Tzschentke TM, Christoph T, Kögel B, et al. (-)-(1R,2R)-3-(3-Dimethylamino-1-ethyl-2-methyl-propyl)-phenol hydrochloride (tapentadol HCl): a novel m-opioid receptor agonist/norepinephrine reuptake inhibitor with broad-spectrum analgesic properties. J Pharmacol Exp Ther. 2007;323:265–76.
Tzschentke TM, De Vry J, Terlinden R, et al. Tapentadol hydrochloride. Analgesic, mu-opioid receptor agonist, noradrenaline reuptake inhibitor. Drugs Future. 2006;31:1053–61.
Lange B, Kuperwasser B, Okamoto A, et al. Efficacy and safety of tapentadol prolonged release for chronic osteoarthritis pain and low back pain. Adv Ther. 2010;27:381–99.
Afilalo M, Etropolski MS, Kuperwasser B, et al. Efficacy and safety of tapentadol extended release compared with oxycodone controlled release for the management of moderate to severe chronic pain related to osteoarthritis of the knee: a randomized, double-blind, placebo- and active-controlled phase III study. Clin Drug Investig. 2010;30:489–505.
Buynak R, Shapiro DY, Okamoto A, et al. Efficacy and safety of tapentadol extended release for the management of chronic low back pain: results of a prospective, randomized, double-blind, placebo- and active-controlled phase III study. Expert Opin Pharmacother. 2010;11:1787–804.
Wild JE, Grond S, Kuperwasser B, et al. Long-term safety and tolerability of tapentadol extended release for the management of chronic low back pain or osteoarthritis pain. Pain Pract. 2010;10:416–27.
Buynak R, Shapiro DY, Okamoto A, et al. Erratum: efficacy and safety of tapentadol extended release for the management of chronic low back pain: results of a prospective, randomized, double-blind, placebo- and active-controlled phase III study. Expert Opin Pharmacother. 2010;11:2773.
Slappendel R, Simpson K, Dubois D, Keininger DL. Validation of the PAC-SYM questionnaire for opioid-induced constipation in patients with chronic low back pain. Eur J Pain. 2006;10:209–17.
Wesson DR, Ling W. The Clinical Opiate Withdrawal Scale (COWS). J Psychoactive Drugs. 2003;35:253–9.
Handelsman L, Cochrane KJ, Aronson MJ, Ness R, Rubinstein KJ, Kanof PD. Two new rating scales for opiate withdrawal. Am J Drug Alcohol Abuse. 1987;13:293–308.
Caldwell JR, Hale ME, Boyd RE, et al. Treatment of osteoarthritis pain with controlled release oxycodone or fixed combination oxycodone plus acetaminophen added to nonsteroidal antiinflammatory drugs: a double blind, randomized, multicenter, placebo controlled trial. J Rheumatol. 1999;26:862–9.
Hale ME, Fleischmann R, Salzman R, et al. Efficacy and safety of controlled-release versus immediate-release oxycodone: randomized, double-blind evaluation in patients with chronic back pain. Clin J Pain. 1999;15:179–83.
Roth SH, Fleischmann RM, Burch FX, et al. Around-the-clock, controlled-release oxycodone therapy for osteoarthritis-related pain: placebo-controlled trial and long-term evaluation. Arch Intern Med. 2000;160:853–60.
Friedmann N, Klutzaritz V, Webster L. Long-term safety of Remoxy® (extended-release oxycodone) in patients with moderate to severe chronic osteoarthritis or low back pain. Pain Med. 2011;12:755–60.
Swegle JM, Logemann C. Management of common opioid-induced adverse effects. Am Fam Physician. 2006;74:1347–54.
Bell TJ, Panchal SJ, Miaskowski C, Bolge SC, Milanova T, Williamson R. The prevalence, severity, and impact of opioid-induced bowel dysfunction: results of a US and European Patient Survey (PROBE 1). Pain Med. 2009;10:35–42.
Panchal SJ, Muller-Schwefe P, Wurzelmann JI. Opioid-induced bowel dysfunction: prevalence, pathophysiology and burden. Int J Clin Pract. 2007;61:1181–7.
Acknowledgments
Sponsorship and article processing charges for this study were funded by Janssen Scientific Affairs, LLC, (New Jersey, USA) and Grünenthal GmbH (Aachen, Germany). Medical writing assistance for this study was provided by Megan Knagge, PhD, of MedErgy (Pennsylvania, USA), and funded by Janssen Research & Development, LLC (New Jersey, USA). The authors would like to acknowledge the contributions of Akiko Okamoto of Janssen Research & Development, LLC. All named authors meet the ICMJE criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval for the version to be published.
Conflict of interest
Mila Etropolski is an employee of Janssen Research & Development, LLC, and is a Johnson & Johnson stockholder. Christine Rauschkolb is an employee of Janssen Research & Development, LLC, and is a Johnson & Johnson stockholder. Brigitte Kuperwasser was an employee of Janssen Research & Development, LLC, at the time the work was performed and is a Johnson & Johnson stockholder. Thomas Häufel is an employee of Grünenthal GmbH. Bernd Lange is an employee of Grünenthal GmbH. Frank Laschewski is an employee of Grünenthal GmbH. Maren Flügel was an employee of Grünenthal GmbH at the time the work was performed.
Compliance with ethics guidelines
The analysis in this article is based on previously conducted studies, and does not involve any new studies of human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
Trial Registration: NCT00421928, NCT00486811, NCT00449176, and NCT00361504.
Data in this manuscript were presented in part at the International Association for the Study of Pain’s 13th World Congress on Pain, August 29 to September 2, 2010, Montreal, Canada; at the British Pain Society’s 2010 Annual Scientific Meeting, April 13–16, 2010, Manchester, England; at the 14th World Society of Pain Clinicians Congress, October 28–31, 2010, Beijing, China; and at the 2010 National Conference on Pain for Frontline Practitioners (PAIN Week), September 8–11, 2010, Las Vegas, Nevada.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Etropolski, M., Kuperwasser, B., Flügel, M. et al. Safety and Tolerability of Tapentadol Extended Release in Moderate to Severe Chronic Osteoarthritis or Low Back Pain Management: Pooled Analysis of Randomized Controlled Trials. Adv Ther 31, 604–620 (2014). https://doi.org/10.1007/s12325-014-0128-6
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-014-0128-6