Abstract
Introduction
This study investigated the intraocular pressure (IOP)-lowering effects and safety of tafluprost ophthalmic solution 0.0015% in actual clinical practice.
Methods
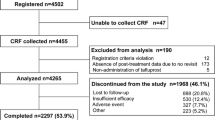
We started a mandatory prospective 2-year observational study, which collected IOP, conjunctival hyperemia score, corneal staining score, and adverse event data from glaucoma and ocular hypertension (OH) patients not previously treated with tafluprost at 2, 12, and 24 months. This report analyzes the 2-month findings.
Results
Of the 4,180 patients from 553 medical institutions in Japan, most patients had primary open-angle glaucoma (POAG, 38.1%) or normal-tension glaucoma (NTG, 44.2%). After 2 months of tafluprost administration, IOP was significantly reduced by 4.3 ± 5.2 mmHg in POAG, 2.4 ± 2.5 mmHg in NTG, 3.6 ± 5.3 mmHg in primary angle-closure glaucoma, 5.6 ± 7.1 mmHg in other types of glaucoma, and 5.3 ± 4.8 mmHg in OH. IOP was significantly reduced by 4.3 ± 4.0 mmHg in the naïve monotherapy group, 1.9 ± 3.5 mmHg in switching from prior treatment, and 3.7 ± 4.1 mmHg in the add-on therapy group. Among patients switched, the prostaglandin analog (PGA) latanoprost was the previous predominant drug (57.4%), followed by travoprost (13.8%). Significant IOP reductions were observed by 1.5 ± 3.4 mmHg in switching from latanoprost and 1.3 ± 3.7 mmHg in switching from travoprost. The conjunctival hyperemia score peaked at 1 month in the naïve monotherapy and add-on therapy groups, whereas it was significantly decreased in patients switched from another PGA. The corneal staining score showed no particular changes. Incidence of adverse drug reaction (ADR) was 7.70 % (322/4,180 patients), and all major ADRs involved the eyes or skin around the eyes.
Conclusion
Tafluprost showed significant IOP-lowering effects without any safety concerns in patients with various types of glaucoma and OH in daily clinical practice and tafluprost is highly effective in any therapeutic patterns.







Similar content being viewed by others
References
Heijl A, Leske MC, Bengtsson B, et al. Reduction of intraocular pressure and glaucoma progression: results from the early manifest glaucoma trial. Arch Ophthalmol. 2002;120:1268–79.
The AGIS investigators. The advanced glaucoma intervention study (AGIS): 7. The relationship between control of intraocular pressure and visual field deterioration. Am J Ophthalmol. 2000;130:429–40.
Collaborative Normal-Tension Glaucoma Study Group. Comparison of glaucomatous progression between untreated patients with normal-tension glaucoma and patients with therapeutically reduced intraocular pressures. Am J Ophthalmol. 1998;126:487–97.
Leske MC, Heijl A, Hussein M, et al. Factors for glaucoma progression and the effect of treatment: the early manifest glaucoma treatment trial. Arch Ophthalmol. 2003;121:48–56.
Marquis RE, Whitson JT. Management of glaucoma: focus on pharmacological therapy. Drugs Aging. 2005;22:1–21.
Takagi Y, Nakajima T, Shimazaki A, et al. Pharmacological characteristics of AFP-168 (tafluprost), a new prostanoid FP receptor agonist, as an ocular hypotensive drug. Exp Eye Res. 2004;78:767–76.
Aihara M. Clinical appraisal of tafluprost in the reduction of elevated intraocular pressure (IOP) in open-angle glaucoma and ocular hypertension. Clin Ophthalmol. 2010;4:163–70.
Iwase A, Suzuki Y, Araie M, et al. The prevalence of primary open-angle glaucoma in Japanese: the Tajimi Study. Ophthalmology. 2004;111:1641–8.
Yamamoto T, Iwase A, Araie M, et al. The Tajimi Study report 2: prevalence of primary angle closure and secondary glaucoma in a Japanese population. Ophthalmology. 2005;112:1661–9.
Ikeda Y, Mori K, Ishibashi T, Naruse S, Nakajima N, Kinoshita S. Latanoprost nonresponders with open-angle glaucoma in the Japanese population. Jpn J Ophthalmol. 2006;50:153–7.
Camras CB, Hedman K, US Latanoprost Study Group. Rate of response to latanoprost or timolol in patients with ocular hypertension or glaucoma. J Glaucoma. 2003;12:466–9.
Mizoguchi T, Ozaki M, Unoki K, Dake Y, Eto T, Arai M. A randomized crossover study comparing tafluprost 0.005% with travoprost 0.004% in patients with normal-tension glaucoma. Clin Ophthalmol. 2012;6:1579–84.
Kawaguchi I, Higashide T, Ohkubo S, Kawaguchi C, Sugiyama K. Comparison of efficacy of four prostaglandin analogues by bilateral treatment in healthy subjects. Jpn J Ophthalmol. 2012;56:346–53.
Kurashima H, Asai Y, Aihara M, Ishida N, Nakamura M, Araie M. Ocular hypotensive effect of tafluprost in latanoprost low-responder cynomolgus monkeys. J Glaucoma. 2012;21:123–8.
Nakano T, Yoshikawa K, Kimura T, Suzumura H, Nanno M, Noro T. Efficacy and safety of tafluprost in normal-tension glaucoma with intraocular pressure of 16 mmHg or less. Jpn J Ophthalmol. 2011;55:605–13.
Uusitalo H, Pillunat LE, Ropo A. Efficacy and safety of tafluprost 0.0015% versus latanoprost 0.005% eye drops in open-angle glaucoma and ocular hypertension: 24-month results of a randomized, double-masked Phase III study. Acta Ophthalmol. 2010;88:12–9.
Schnober D, Hofmann G, Maier H, Scherzer ML, Ogundele AB, Jasek MC. Diurnal IOP-lowering efficacy and safety of travoprost 0.004% compared with tafluprost 0.0015% in patients with primary open-angle glaucoma or ocular hypertension. Clin Ophthalmol. 2010;8:1459–63.
Acknowledgments
All named authors meet the ICMJE criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval for the version to be published. We wish to express our gratitude to the physicians at the medical institutions who cooperated in the study. Sponsorship and article processing charges for this study were funded by Santen Pharmaceutical Co., Ltd., Osaka, Japan. English language editing and manuscript preparation for submission for this study were provided by James Eudeikis, Forte Science Communications (Tokyo, Japan) and Hiromi Okubo, Springer Japan (Tokyo, Japan). This support was funded by Santen Pharmaceutical Co. Ltd. (Osaka, Japan).
Conflict of interest
Yasuaki Kuwayama is affiliated with Fukushima Eye Clinic, and has received consulting fees from Bausch & Lomb Japan, Kowa Pharmaceutical, Pfizer Japan, Santen Pharmaceutical and Senju Pharmaceutical, and honoraria from Alcon Japan, MSD and Otsuka Pharmaceutical. Akio Nomura is an employee of Santen Pharmaceutical Co., Ltd.
Compliance with ethics guidelines
This current on-going post-marketing, multicenter, prospective, non-interventional, observational study is being conducted in accordance with the requirements of the regulatory authority in Japan, the Good Post-Marketing Study Practice (MHLW Ordinance No. 171; December 20, 2004). The study began in December 2008 and is scheduled to run through December 2014. Since the research protocol was reviewed and approved by the regulatory authority in Japan prior to beginning the study, approval by the ethics review committees at each participating medical institution is not required. The Japanese regulatory authority does not require informed consent for post-marketing observational studies; this study did not obtain informed consent from the patients.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kuwayama, Y., Nomura, A. Prospective Observational Post-Marketing Study of Tafluprost for Glaucoma and Ocular Hypertension: Short-Term Efficacy and Safety. Adv Ther 31, 461–471 (2014). https://doi.org/10.1007/s12325-014-0109-9
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-014-0109-9