Abstract
Background
Regular aftercare attendance following laparoscopic adjustable gastric banding (LAGB) is associated with greater weight loss and fewer post-surgical complications. Despite high reported rates of attrition from LAGB aftercare, the reasons for non-attendance have not been previously explored. The present study aimed to explore patient-reported barriers to LAGB aftercare attendance, and the perceived helpfulness of potential attrition-reducing strategies, in both regular attendees and non-attendees of aftercare.
Methods
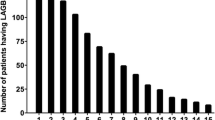
One hundred and seventy-nine participants (107 regular attendees and 72 non-attendees) completed a semi-structured questionnaire, assessing barriers to attrition (101 items) and usefulness of attrition prevention strategies (14 items).
Results
Findings indicate that both regular attendees and non-attendees experience multiple barriers to aftercare attendance. Non-attendees generally reported that barriers had a greater impact on their aftercare attendance. There was evidence for some level of acceptability for attrition-reducing strategies suggesting that LAGB patients may be receptive to such strategies.
Conclusions
Current findings highlight the importance of assessing barriers to treatment in both attendees and non-attendees. It is proposed that addressing barriers that differentiate non-attendees from attendees may be most effective in reducing attrition from aftercare.


Similar content being viewed by others
References
O’Brien P, McDonald L, Anderson M, et al. Long term outcomes after bariatric surgery: fifteen-year follow up after gastric banding and a systematic review of the literature. Ann Surg. 2013;257(1):87–94.
Dixon JB, Laurie CP, Anderson ML, et al. Motivation, readiness to change, and weight loss following adjustable gastric band surgery. Obesity. 2009;17(4):698–705.
Shen R, Dugay G, Rajaram K, et al. Impact of patient follow-up on weight loss after bariatric surgery. Obes Surg. 2004;14(4):514–9.
Odom J, Zalesin KC, Washington TL, et al. Behavioral predictors of weight regain after bariatric surgery. Obes Surg. 2010;20(3):349–56.
Poole N. Compliance with surgical after-care following bariatric surgery for morbid obesity: a retrospective study. Obes Surg. 2005;15(2):261–5.
te Riele WW. Long-term results of laparoscopic adjustable gastric banding in patients lost to follow-up. Br J Surg. 2010;97(10):1535–40.
Wheeler E, Prettyman A, Lenhard MJ, et al. Adherence to outpatient program postoperative appointments after bariatric surgery. Surg Obes Relat Dis. 2008;4(4):515–20.
Sivagnanam P, Rhodes M. The importance of follow-up and distance from centre in weight loss after laparoscopic adjustable gastric banding. Surg Endosc. 2010;24(10):2432–8.
Pontiroli AE, Fossati A, Vedani P, et al. Post-surgery adherence to scheduled visits and compliance, more than personality disorders, predict outcome of bariatric restrictive surgery in morbidly obese patients. Obes Surg. 2007;17(11):1492–7.
Moroshko I, O’Brien P, Brennan L. Patients’ perspectives on laparoscopic adjustable gastric banding (LAGB) aftercare attendance: qualitative assessment. Obes Surg. 2014;24(2):266–75.
DeNino WF, Osler T, Evans EG, et al. Travel distance as factor in follow-up visit compliance in postlaparoscopic adjustable gastric banding population. Surg Obes Relat Dis. 2010;6(6):597–600.
Brennan L, Walkley J, Wilks R. Parent-and adolescent-reported barriers to participation in an adolescent overweight and obesity intervention. Obesity. 2012;20(6):1319–24.
Greenberg I, Stampfer MJ, Schwarzfuchs D, et al. Adherence and success in long-term weight loss diets: the dietary intervention randomized controlled trial. J Am Coll Nutr. 2009;28(2):159–68.
Lara MD, Baker MT, Larson CJ, et al. Travel distance, age, and sex as factors in follow-up visit compliance in the post-gastric bypass population. Surg Obes Relat Dis. 2005;1(1):17–21.
Huisman S, Maes S, De Gucht VJ, et al. Low goal ownership predicts drop-out from a weight intervention study in overweight patients with type 2 diabetes. Int J Behav Med. 2010;17(3):176–81.
Kolotkin RL, Moore JM. Attrition in a behavioral weight-control program: a comparison of dropouts and completers. Int J Eat Disord. 1983;2(3):93–100.
Pekarik G, Blodgett C, Evans RG, et al. Variables related to continuance in a behavioral weight loss program. Addict Behav. 1984;9(4):413–6.
Teixeira PJ, Going SB, Houtkooper LB, et al. Pretreatment predictors of attrition and successful weight management in women. Int J Obes. 2004;28(9):1124–33.
Clark MM, Niaura R, King TK, et al. Depression, smoking, activity level, and health status: pretreatment predictors of attrition in obesity treatment. Addict Behav. 1996;21(4):509–13.
Graffagnino CL, Falko JM, La Londe M, et al. Effect of a community-based weight management program on weight loss and cardiovascular disease risk factors. Obesity. 2006;14(2):280–8.
Packianathan I, Sheikh M, Boniface D, et al. Predictors of programme adherence and weight loss in women in an obesity programme using meal replacements. Diabetes Obes Metab. 2005;7(4):439–47.
Moroshko I, Brennan L, O’Brien P. Predictors of dropout in weight loss interventions: a systematic review of the literature. Obes Rev. 2011;12(11):912–34.
Barlow SE, Ohlemeyer CL. Parent reasons for nonreturn to a pediatric weight management program. Clin Pediatr. 2006;45:355–60.
Grossi E, Grave R, Mannucci E, et al. Complexity of attrition in the treatment of obesity: clues from a structured telephone interview. Int J Obes. 2006;30(7):1132–7.
Gross D, Julion W, Fogg L. What motivates participation and dropout among low-income urban families of color in a prevention intervention? Fam Relat. 2001;50(3):246–54.
Kirk E, Jacobsen D, Gibson C, et al. Time course for changes in aerobic capacity and body composition in overweight men and women in response to long-term exercise: the Midwest Exercise Trial (MET). Int J Obes. 2003;27(8):912–9.
McManus K, Antinoro L, Sacks F. A randomized controlled trial of a moderate-fat, low-energy diet compared with a low fat, low-energy diet for weight loss in overweight adults. Int J Obes. 2001;25(10):1503–11.
Read A, Ramwell H, Strorer H, et al. A primary care intervention programme for obesity and coronary heart disease risk factor reduction. Br J Gen Pract. 2004;54(501):272–8.
Stahre L, Hallstrom T. A short-term cognitive group treatment program gives substantial weight reduction up to 18 months from the end of treatment. A randomized controlled trial. Eat Weight Disord. 2005;10(1):51–8.
Harvey-Berino J, Pintauro S, Buzzell P, et al. Effect of internet support on the long-term maintenance of weight loss. Obes Res. 2004;12(2):320–9.
Lantz H, Peltonen M, Agren L, et al. A dietary and behavioural programme for the treatment of obesity: a 4-year clinical trial and a long-term posttreatment follow-up. J Intern Med. 2003;254(3):272–9.
Melin I, Karlstrom B, Lappalainen R, et al. A programme of behaviour modification and nutrition counselling in the treatment of obesity: a randomised 2-y clinical trial. Int J Obes. 2003;27(9):1127–35.
Garvey WT, Ryan DH, Look M, et al. Two-year sustained weight loss and metabolic benefits with controlled-release phentermine/topiramate in obese and overweight adults (SEQUEL): A randomized, placebo-controlled, phase 3 extension study. Am J Clin Nutr. 2012;95(2):297–308.
Goulis D, Giaglis G, Boren S, et al. Effectiveness of home-centered care through telemedicine applications for overweight and obese patients: a randomized controlled trial. Int J Obes. 2004;28(11):1391.
McElroy SL, Frye MA, Altshuler LL, et al. A 24-week, randomized, controlled trial of adjunctive sibutramine versus topiramate in the treatment of weight gain in overweight or obese patients with bipolar disorders. Bipolar Disor. 2007;9(4):426–34.
Elder C, Ritenbaugh C, Mist S, et al. Randomized trial of two mind-body interventions for weight-loss maintenance. J Altern Complement Med. 2007;13(1):67–78.
Jacobsen DJ, Donnelly JE, Snyder-Heelan K, et al. Adherence and attrition with intermittent and continuous exercise in overweight women. Int J Sport Med. 2003;26(4):459–64.
Kushner RF, Blatner DJ, Jewell DE, et al. The PPET Study: people and pets exercising together. Obesity. 2006;14(10):1762–70.
Goldberg JH, Kiernan M. Innovative techniques to address retention in a behavioral weight-loss trial. Health Educ Res. 2005;20(4):439–47. doi:10.1093/her/cyg139.
Macleod M, Craigie AM, Barton KL, et al. Recruiting and retaining postpartum women from areas of social disadvantage in a weight-loss trial: an assessment of strategies employed in the WeighWell feasibility study. Matern Child Nutr. 2012;9(3):322–31.
Perri MG, Martin A, Leermakers EA, et al. Effects of group- versus home-based exercise in the treatment of obesity. J Consult Clin Psychol. 1997;65(2):278–85.
Smith CH. The effects of telephone prompting and programmed homework in behavioral treatment of the obese. Diss Abstr Int. 1978;39(6):3007–8.
Brownell KD, Stunkard AJ, McKeon PE. Weight reduction at the work site: a promise partially fulfilled. Am J Psychiatr. 1985;142(1):47–52.
Pekarik G. The effects of program duration on continuance in a behavioral weight loss program. Addict Behav. 1987;12(4):381–4.
Ard JD, Kumanyika S, Stevens VJ, et al. Effect of group racial composition on weight loss in African Americans. Obesity. 2008;16(2):306–10.
Karanja N, Stevens VJ, Hollis JF, et al. Steps to soulful living (steps): a weight loss program for African-American women. Ethn Dis. 2002;12(3):363–71.
Jeffery RW, Sherwood NE, Brelje K, et al. GOOD EMail and phone interventions for weight loss in a managed-care setting: Weigh-To-Be one-year outcomes. Int J Obes. 2003;27(12):1584–92.
Shapiro JR, Bauer S, Hamer RM, et al. Use of text messaging for monitoring sugar-sweetened beverages, physical activity, and screen time in children: a pilot study. J Nut Educ Behav. 2008;40(6):385–91.
Keller CS, Gonzales A, Fleuriet K. Retention of minority participants in clinical research studies. West J Nurs Res. 2005;27(3):292–306.
Richardson CR, Buis LR, Janney AW, et al. An online community improves adherence in an internet-mediated walking program. Part 1: results of a randomized controlled trial. J Med Internet Res. 2010;12(4):e71.
Wing RR, Jeffery RW. Benefits of recruiting participants with friends and increasing social support for weight loss and maintenance. J Consult Clin Psychol. 1999;67(1):132–8.
Minniti A, Bissoli L, Di Francesco V, et al. Individual versus group therapy for obesity: comparison of dropout rate and treatment outcome. Eat Weight Disord. 2007;12(4):161–7.
Jeffery RW, Forster JL, Snell MK. Promoting weight control at the worksite: a pilot program of self-motivation using payroll-based incentives. Prev Med. 1985;14(2):187–94.
Lasco RA, Curry RH, Dickson VJ, et al. Participation rates, weight loss, and blood pressure changes among obese women in a nutrition-exercise program. Pubic Health Rep. 1989;104(6):640–6.
Parra-Medina D, D’Antonio A, Smith SM, et al. Successful recruitment and retention strategies for a randomized weight management trial for people with diabetes living in rural, medically underserved counties of South Carolina: the POWER study. J Am Diet Assoc. 2004;104(1):70–5.
Schelling S, Munsch S, Meyer AH, et al. Increasing the motivation for physical activity in obese patients. Int J Eat Disord. 2009;42(2):130–8. doi:10.1002/eat.20595.
DiMarco ID, Klein DA, Clark VL, et al. The use of motivational interviewing techniques to enhance the efficacy of guided self-help behavioral weight loss treatment. Eat Behav. 2009;10(2):134–6.
Smith DE, Heckemeyer CM, Kratt PP, et al. Motivational interviewing to improve adherence to a behavioral weight-control program for older obese women with NIDDM: a pilot study. Diabetes Care. 1997;20(1):52–4.
VanWormer JJ, Boucher JL. Motivational interviewing and diet modification: a review of the evidence. Diabetes Educ. 2004;30(3):404–6.
Cowan RJ, Sheridan SM. Investigating the acceptability of behavioral interventions in applied conjoint behavioral consultations: moving from analog conditions to naturalistic settings. Sch Psychol Q. 2003;18(1):1–21.
Kazdin AE. Acceptability of alternative treatments for deviant child behavior. J Appl Behav Anal. 1980;13:259–73.
Kazdin AE. Acceptability of child treatment techniques: the influence of treatment efficacy and adverse side effects. Behav Ther. 1981;12:439–506.
Kazdin AE. Perceived barriers to treatment participation and treatment acceptability among antisocial children and their families. J Child Fam Stud. 2000;9(2):157–74.
Nelson TD, Steele RG. Beyond efficacy and effectiveness: a multifaceted approach to treatment evaluation. Prof Psychol Res Prac. 2006;37:389–97.
Sidani S, Miranda J, Epstein DR, et al. Relationships between personal beliefs and treatment acceptability, and preferences for behavioral treatments. Behave Res Ther. 2009;47(10):823–9.
DeVellis RF. Scale development: theory and applications. 2nd ed. Newbury Park: Sage Publications; 2003.
Frazer L, Lawley M. Questionnaire design & administration: a practical guide. Milton: John Wiley & Sons Ltd; 2000.
Melin I, Reynisdottir S, Berglund L, et al. Conservative treatment of obesity in an academic obesity unit. Long-term outcome and drop-out. Eat Weight Disord. 2006;11(1):22–30.
Caltabiano ML, Sarafino EP. Health psychology: biopsychosocial interactions. An Australian Perspective. Milton: John Wiley & Sons; 2002.
Livhits M, Mercado C, Yermilov I, et al. Preoperative predictors of weight loss following bariatric surgery: systematic review. Obes Surg. 2012;22(1):70–89.
Moroshko I, Brennan L, O’Brien P. Predictors of attrition in bariatric aftercare: a systematic review of the literature. Obes Surg. 2012;22(10):1640–7.
Weingarten SR, Henning JM, Badamgarav E, et al. Interventions used in disease management programmes for patients with chronic illness—which ones work? Meta-analysis of published reports. BMJ. 2002;325(7370):925.
Wagner E, Austin B, Von Korff M. Organising care for patients with chronic illness. Millbank Q. 1996;74(4):511–44.
World Health Organization. Innovative care for chronic conditions: building blocks for action: global report. Geneva: World Health Organization; 2002.
Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness. JAMA. 2002;288(14):1775–9.
Battersby MW, Kit JA, Prideaux C, et al. Implementing the flinders model of self-management support with aboriginal people who have diabetes: findings from a pilot study. Aust J Prim Health. 2008;14(1):66–74.
Lorig KR, Ritter P, Stewart AL, et al. Chronic disease self-management program: 2-year health status and health care utilization outcomes. Med Care. 2001;39(11):1217–23.
Zwar NA, Harris M, Griffiths R, et al. A systematic review of chronic disease management. APHCRI: Canberra; 2006.
Lorig KR, Sobel DS, Stewart AL, et al. Evidence suggesting that a chronic disease self-management program can improve health status while reducing hospitalization: a randomized trial. Med Care. 1999;37(1):5–14.
Funnell MM. Empowerment and self-management after weight loss surgery. Obes Surg. 2005;15:417–22.
Conflict of Interest
The Centre for Obesity Research and Education (CORE) receives a grant from Allergan for research support. The grant is not tied to any specified research projects, and Allergan has no control of the protocol, analysis and reporting of any studies. CORE also receives a grant from Applied Medical towards the educational programmes. Dr Paul O’Brien reported having written a patient information book entitled The LAP-BAND Solution: A Partnership for Weight Loss which was published by Melbourne University Publishing in 2007. Most copies are given to patients without charge, but he reports that he derives a financial benefit from the copies that are sold. He also reports receiving compensation as the national medical director of the American Institute of Gastric Banding, a multicentre facility, based in Dallas, Texas, that treats obesity predominantly by gastric banding. No other authors reported disclosures.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hochberg, L.S., Murphy, K.D., O’Brien, P.E. et al. Laparoscopic Adjustable Gastric Banding (LAGB) Aftercare Attendance and Attrition. OBES SURG 25, 1693–1702 (2015). https://doi.org/10.1007/s11695-015-1597-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-015-1597-7