Abstract
Summary
Changes in bed management and access policy aimed to shorten Canadian hip fracture hospital stay. Secular trends in hip fracture total, preoperative, and postoperative stay are unknown. Hip fracture stay shortened from 2004 to 2012, mostly from shortening postoperative stay. This may reflect changes in bed management rather than access policy.
Purpose
To compare the probability of discharge by time after patient admission to hospital with first-time hip fracture over a period of nine calendar years.
Methods
We retrieved acute hospitalization records for 169,595 patients 65 years and older, who were admitted to an acute care hospital with hip fracture between 2004 and 2012 in Canada (outside of Quebec). The main outcome measure was cumulative incidence of discharge by inpatient day, accounting for competing events that end hospital stay.
Results
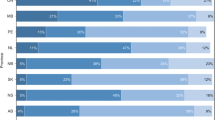
The probability of surgical discharge within 30 days of admission increased from 57.2 % in 2004 to 67.3 % in 2012. The probability of undergoing surgery on day of admission or day after fluctuated around 58.5 % over the study period. For postoperative stay, the discharge probability increased from 6.8 to 12.2 % at day 4 after surgery and from 57.2 to 66.6 % at day 21 after surgery, between 2004 and 2012. The differences across years persisted after adjustment for characteristics of patients, fracture, comorbidity, treatment, type and timing of surgery, and access to care.
Conclusions
Hospital stay following hip fracture shortened substantially between 2004 and 2012 in Canada, mostly due to shortening of postoperative stays. Shorter hospital stays may reflect changes in bed management protocols rather than in access policy.




Similar content being viewed by others
References
Sutherland JM, Crump RT (2013) Alternative level of care: Canada’s hospital beds, the evidence and options. Healthc Policy 9:26–34
Barrett B, Way C, McDonald J, Parfrey P (2005) Hospital utilization, efficiency and access to care during and shortly after restructuring acute care in Newfoundland and Labrador. J Health Serv Res Policy 10(Suppl 2):S2–S7
Evans B, Potvin C, Johnson G, Henderson N, Yuen I, Smith T, Metham S, Taylor S, Sniekers D (2011) Enhancing patient flow in an acute care hospital: successful strategies at the Juravinski Hospital. Healthc Q 14:66–74
Barrett J, Doyle W, Higgins D (2008) Corporate patient flow: “changing a culture through strategic planning and Accreditation Canada”. http://www.healthcarecan.ca/wp-content/uploads/2014/07/Changing-a-culture-though-strategic-planning-and-Accreditation-Canad.pdf Accessed 24 July 2015
Waddell J, McMullan J, Lo N, OConnor M, Sheppard L, Mensour M, Palda V, McGlasson R (2010) Improving time to surgery—emergency room, preoperative and immediate postoperative clinical practice guidelines for the management of hip fracture patients. Bone & Joint Health Network. http://boneandjointcanada.com/wp-content/uploads/2014/05/ER-Pre-op-Clinical-Practice-Guidelines-20101101_Final.pdf Accessed 24 July 2015
Ontario Ministry of Health and Long-Term Care (2005) First ever common benchmarks will allow canadians to measure progress in reducing wait times. www.health.gov.on.ca/english/media/news_releases/archives/nr_05/nr_121205.html Accessed 24 July 2015
Orosz GM, Magaziner J, Hannan EL, Morrison RS, Koval K, Gilbert M, McLaughlin M, Halm EA, Wang JJ, Litke A, Silberzweig SB, Siu AL (2004) Association of timing of surgery for hip fracture and patient outcomes. JAMA 291:1738–1743
Mariconda M, Costa GG, Cerbasi S, Recano P, Aitanti E, Gambacorta M, Misasi M (2015) The determinants of mortality and morbidity during the year following fracture of the hip: a prospective study. Bone Joint J 97-B:383–390
Simunovic N, Devereaux PJ, Sprague S, Guyatt GH, Schemitsch E, DeBeer J, Bhandari M (2010) Effect of early surgery after hip fracture on mortality and complications: systematic review and meta-analysis. CMAJ 182:1609–1616
Ho V, Hamilton BH, Roos LL (2000) Multiple approaches to assessing the effects of delays for hip fracture patients in the United States and Canada. Health Serv Res 34:1499–1518
Lefaivre KA, Macadam SA, Davidson DJ, Gandhi R, Chan H, Broekhuyse HM (2009) Length of stay, mortality, morbidity and delay to surgery in hip fractures. J Bone Joint Surg (Br) 91:922–927
Canadian Institute for Health Information (2007) Health Indicators 2007. CIHI, Ottawa
Canadian Institute for Health Information (2011) Data quality documentation for external users: Discharge Abstract Database, 2010–2011. CIHI, Ottawa
Ahmed I, Khan MA, Nayak V, Mohsen A (2014) An evidence-based warfarin management protocol reduces surgical delay in hip fracture patients. J Orthop Traumatol 15:21–27
Lee DJ, Elfar JC (2014) Timing of hip fracture surgery in the elderly. Geriatr Orthop Surg Rehabil 5:138–140
Fransoo R, Yogendran M, Olafson K, Ramsey C, McGowan KL, Garland A (2012) Constructing episodes of inpatient care: data infrastructure for population-based research. BMC Med Res Methodol 12:133
Kaboli PJ, Go JT, Hockenberry J, Glasgow JM, Johnson SR, Rosenthal GE, Jones MP, Vaughan-Sarrazin M (2012) Associations between reduced hospital length of stay and 30-day readmission rate and mortality: 14-year experience in 129 Veterans Affairs hospitals. Ann Intern Med 157:837–845
Vidan MT, Sanchez E, Gracia Y, Maranon E, Vaquero J, Serra JA (2011) Causes and effects of surgical delay in patients with hip fracture: a cohort study. Ann Intern Med 155:226–233
Pintilie M (2006) Competing risks, a practical perspective. John Wiley & Sons
Klein JP, Andersen PK (2005) Regression modeling of competing risks data based on pseudovalues of the cumulative incidence function. Biometrics 61:223–229
Bland JM, Altman DG (1998) Survival probabilities (the Kaplan-Meier method). BMJ 317:572
Gray B (2014) cmprsk: Subdistribution analysis of competing risks. http://CRAN.R-project.org/package=cmprsk Accessed 24 July 2015
Gerds T (2014) prodlim: Product-limit estimation for censored event history analysis. http://CRAN.R-project.org/package=prodlim Accessed 24 July 2015
Hojsgaard S, Halekoh U, Yan J (2006) The R package geepack for generalized estimating equations. J Stat Softw 15:1–11
R core team (2015) R: a language and environment for statistical computing
Nikkel LE, Fox EJ, Black KP, Davis C, Andersen L, Hollenbeak CS (2012) Impact of comorbidities on hospitalization costs following hip fracture. J Bone Joint Surg Am 94:9–17
Auais M, Morin S, Nadeau L, Finch L, Mayo N (2013) Changes in frailty-related characteristics of the hip fracture population and their implications for healthcare services: evidence from Quebec, Canada. Osteoporos Int 24(10):2713–2724
Ban I, Palm H, Birkelund L, Eschen J, Kring S, Brix M, Troelsen A (2014) Implementing, adapting, and validating an evidence-based algorithm for hip fracture surgery. J Orthop Trauma 28:e21–e26
Moran CG, Wenn RT, Sikand M, Taylor AM (2005) Early mortality after hip fracture: is delay before surgery important? J Bone Joint Surg Am 87:483–489
Ricci WM, Brandt A, McAndrew C, Gardner MJ (2015) Factors affecting delay to surgery and length of stay for patients with hip fracture. J Orthop Trauma 29:e109–e114
Orosz GM, Hannan EL, Magaziner J, Koval K, Gilbert M, Aufses A, Straus E, Vespe E, Siu AL (2002) Hip fracture in the older patient: reasons for delay in hospitalization and timing of surgical repair. J Am Geriatr Soc 50:1336–1340
Tracey J, Forte T, Fagbemi J, Chaudhary Z (2007) Wait time for hip fracture surgery in Canada. Healthc Q 10:24–27
Motohashi T, Hamada H, Lee J, Sekimoto M, Imanaka Y (2013) Factors associated with prolonged length of hospital stay of elderly patients in acute care hospitals in Japan: a multilevel analysis of patients with femoral neck fracture. Health Policy 111:60–67
Canadian Institute for Health Information (2005) Inpatient hospitalizations and average length od stay trends in Canada, 2003–2004 and 2004–2005. CIHI, Ottawa
Canadian Institute for Health Information (2005) Hospital trends in Canada—results of a project to create a historical series of statistical and financial data for Canadian hospitals over twenty-seven years. CIHI, Ottawa
Kralj B, Kantarevic J (2012) Primary care model enrolment and hospital length of stay in Ontario: patient rostering associated with reduced length of stay, significant health system savings. Ontario Medical Review. 16–19
OECD (2011) Average length of stay in hospitals. In: Health at a Glance 2011: OECD Indicators. OECD Publishing
Neuburger J, Harding KA, Bradley RJ, Cromwell DA, Gregson CL (2014) Variation in access to community rehabilitation services and length of stay in hospital following a hip fracture: a cross-sectional study. BMJ Open 4:e005469
Nordstrom P, Gustafson Y, Michaelsson K, Nordstrom A (2015) Length of hospital stay after hip fracture and short term risk of death after discharge: a total cohort study in Sweden. BMJ 350:h696
Williams N, Hardy BM, Tarrant S, Enninghorst N, Attia J, Oldmeadow C, Balogh ZJ (2013) Changes in hip fracture incidence, mortality and length of stay over the last decade in an Australian major trauma centre. Arch Osteoporos 8(1–2):150
Holvik K, Ranhoff AH, Martinsen MI, Solheim LF (2010) Predictors of mortality in older hip fracture inpatients admitted to an orthogeriatric unit in Oslo, Norway. J Aging Health 22:1114–1131
Miani C, Ball S, Pitchforth E, Exley J, King S, Roland M, Fuld J, Nolte E (2014) Organisational interventions to reduce length of stay in hospital: a rapid evidence assessment. health services and delivery research
Neuburger J, Currie C, Wakeman R, Tsang C, Plant F, De SB, Cromwell DA, van der Meulen J (2015) The impact of a national clinician-led audit initiative on care and mortality after hip fracture in England: an external evaluation using time trends in non-audit data. Med Care 53:686–691
Boddaert J, Cohen-Bittan J, Khiami F, Le MY, Raux M, Beinis JY, Verny M, Riou B (2014) Postoperative admission to a dedicated geriatric unit decreases mortality in elderly patients with hip fracture. PLoS One 9(1):e83795
Suhm N, Kaelin R, Studer P, Wang Q, Kressig RW, Rikli D, Jakob M, Pretto M (2014) Orthogeriatric care pathway: a prospective survey of impact on length of stay, mortality and institutionalisation. Arch Orthop Trauma Surg 134:1261–1269
Leslie WD, O’Donnell S, Jean S, Lagace C, Walsh P, Bancej C, Morin S, Hanley DA, Papaioannou A (2009) Trends in hip fracture rates in Canada. JAMA 302:883–889
Ko FC, Morrison RS (2014) Hip fracture: a trigger for palliative care in vulnerable older adults. JAMA Intern Med 174:1281–1282
Meier DE (2011) Increased access to palliative care and hospice services: opportunities to improve value in health care. Milbank Q 89:343–380
Acknowledgments
We gratefully acknowledge the guidance from the CIHI experts in understanding the discharge abstracts.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Funding source
This research was funded by the Canadian Institute for Health Research. This funder had no role in the design of this study, execution, analyses, data interpretation, or decision to submit results for publication.
Conflicts of interest
The following competing interests are declared: (1) PG has received grants from the Canadian Institutes of Health Research related to this work. PG also receives funding from the Natural Sciences and Engineering Research Council of Canada, the Canadian Foundation for Innovation, and the British Columbia Specialists Services Committee for work around hip fracture care not related to this manuscript. He has also received fees from the BC Specialists Services Committee (for a provincial quality improvement project on redesign of hip fracture care) and from Stryker Orthopedics (as a product development consultant). He is a board member and shareholder in Traumis Surgical Systems Inc. and a board member for the Canadian Orthopedic Foundation. He also serves on the speakers’ bureaus of AO Trauma North America and Stryker Canada. (2) SNM reports grants from Amgen Canada, grants from Merck, personal fees from Amgen Canada, and personal fees from Eli Lilly outside the submitted work. (3) KS is a postdoctoral fellow whose salary is paid by Canadian Institutes of Health Research funding related to this work. (4) BS, LK, EB, LB, JMS, MD, DG, EH declare that they have no conflicts of interest.
Additional information
The following are members of the Canadian Collaborative Study on Hip Fractures: Eric Bohm, Lauren Beaupre, Michael Dunbar, Donald Griesdale, Pierre Guy, Edward Harvey, Erik Hellsten, Susan Jaglal, Hans Kreder, Lisa Kuramoto, Adrian Levy, Suzanne N. Morin, Katie Jane Sheehan, Boris Sobolev, Jason M. Sutherland, and James Waddell.
Boris Sobolev and Pierre Guy contributed equally to this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Additional File 1
(DOC 30 kb)
Additional File 2
(DOC 189 kb)
Rights and permissions
About this article
Cite this article
Sobolev, B., Guy, P., Sheehan, K.J. et al. Time trends in hospital stay after hip fracture in Canada, 2004–2012: database study. Arch Osteoporos 11, 13 (2016). https://doi.org/10.1007/s11657-016-0264-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-016-0264-5