Abstract
Background
Hospital care on weekends has been associated with delays in care, reduced quality, and poor clinical outcomes.
Objective
The purpose of this study was to evaluate the impact of a weekend hospital intervention on processes of care and clinical outcomes. The multifaceted intervention included expanded weekend diagnostic services, improved weekend discharge processes, and increased physician and care management services on weekends.
Design and Patients
This was an interrupted time series observational study of adult non-obstetric patients hospitalized at a single academic medical center between January 2011 and January 2014. The study included 18 months prior to and 19 months following the implementation of the intervention. Data were analyzed using segmented regression analysis with adjustment for confounders.
Main Measures
The primary outcome was average length of stay. Secondary outcomes included percent of patients discharged on weekends, 30-day readmission rate, and in-hospital mortality rate.
Key Results
The study included 57,163 hospitalizations. Following implementation of the intervention, average length of stay decreased by 13 % (95 % CI 10–15 %) and continued to decrease by 1 % (95 % CI 1–2 %) per month as compared to the underlying time trend. The proportion of weekend discharges increased by 12 % (95 % CI 2–22 %) at the time of the intervention and continued to increase by 2 % (95 % CI 1–3 %) per month thereafter. The intervention had no impact on readmissions or mortality. During the post-implementation period, the hospital was evacuated and closed for 2 months due to damage from Hurricane Sandy, and a new hospital-wide electronic health record was introduced. The contributions of these events to our findings are not known. We observed a lower inpatient census and found differences in patient characteristics, including higher rates of Medicaid insurance and comorbidities, in the post-Hurricane Sandy period as compared to the pre-Sandy period.
Conclusions
The intervention was associated with a reduction in length of stay and an increase in weekend discharges. Our longitudinal study also illuminated the challenges of evaluating the effectiveness of a large-scale intervention in a real-world hospital setting.
Similar content being viewed by others
INTRODUCTION
Multiple studies have demonstrated that there are differences in the quality of care delivered in hospitals, depending on the day of the week. Compared to care on weekdays, care on weekends has been associated with delays,1,2 decreased intensity,3,4 and poorer performance on quality-of-care metrics such as time to reperfusion for acute myocardial infarction and completion of discharge instructions.5–11 This variability in care may have important clinical implications, as weekends in the hospital have been associated with increased mortality.8–15
At our medical center, we observed that the number of discharges was substantially lower on weekends than on weekdays. The number of discharges was highest on Mondays, and hospitalizations that ended on Monday were associated with a long length of stay. These observations suggested that there were delays in care over the weekend leading to increased length of stay. Furthermore, we observed that while some services, such as imaging or operating rooms, were at or even above capacity during the week, they were being underutilized on weekends. To address concerns related to differences in care throughout the week, our medical center instituted an intervention to increase weekend services and staffing called the 7-Day Hospital Initiative.16 This was a major initiative that was championed by hospital executive leadership and was guided by a steering committee that included both clinical (e.g. chief medical officer, chief nursing officer) and operational (e.g. chief of hospital operations, chief information officer) leadership. The purpose of the current study was to evaluate the effectiveness of this intervention on length of stay and other process and outcome measures.
METHODS
Design and Setting
We performed an interrupted time series observational study of patients hospitalized at Tisch Hospital, a 705-bed teaching hospital that is the flagship acute care hospital of NYU Langone Medical Center. In this quasi-experimental design, changes in an outcome are associated with the introduction of an intervention while accounting for temporal trends in the outcome.17 Patients eligible for inclusion in the study were those who were 18 years of age and older and who were admitted to the hospital after January 1, 2011 and discharged before January 31, 2014. We excluded patients on the obstetrical service and patients who were discharged on October 30, 2012, the day on which the hospital was evacuated due to the effects of Hurricane Sandy.
This study was approved by the NYU School of Medicine Institutional Review Board (IRB).
Intervention
The 7-Day Hospital Initiative was a multifaceted intervention consisting of five major components: 1) expanded access to diagnostic procedures on weekends; 2) expanded hospitalist coverage on the medicine service on weekends, with improved structure for patient handoffs; 3) increased care management services on weekends; 4) improved discharge processes; and 5) increased elective surgeries on weekends (Table 1). In addition, providers and staff were encouraged to provide ongoing feedback regarding weekend quality of care in order to foster ongoing improvement.
Initial discussions related to targeting weekend versus weekday variations in care began in late 2010,16 based on evaluation by hospital operations as well as feedback from physicians, nurses, and other clinicians regarding the causes of weekend hospital inefficiencies. Implementation of the intervention largely occurred in calendar year 2012. For analytic purposes, we considered the 7-Day Hospital Initiative implementation to have started on July 1, 2012, the date on which the hospitalist service component of the initiative began.
Hurricane Sandy
On October 29, 2012, Hurricane Sandy descended upon New York City, resulting in widespread flooding and loss of power. NYU Langone Medical Center sustained extensive damage from the storm, requiring emergency evacuation of more than 300 inpatients and closure of the hospital to repair infrastructure.18 Surgical and intensive care unit inpatient services were reopened on December 27, and nearly all other inpatient services were restored by January 14, 2013.19,20 The emergency department remained under construction for the duration of the current study and reopened April 2014, with an urgent care center established in the interim to provide immediate patient care.20
Change in Electronic Health Record (EHR)
A new EHR, Epic (Epic Systems, Verona, WI, USA), was implemented in December 2012, and replaced the previous EHR for inpatient services, Sunrise Clinical Manager (Allscripts, Chicago, IL, USA). The change in EHR coincided with hospital reopening following Hurricane Sandy.
Study Measures
The primary study outcome was average length of stay. Secondary outcomes included percent of weekend (versus weekday) discharges, in-hospital mortality, and 30-day hospital readmission. For evaluation of 30-day readmission, we captured readmissions only to our medical center and excluded patients who died during the index hospitalization. Patients discharged in October 2012 were also excluded from this analysis due to incomplete 30-day follow-up as a result of hospital closure.
We also examined a secondary outcome of electronic health record (EHR) interactions, a measure of hospital care intensity which is defined as the number of times any provider accesses an individual patient chart. This measure has demonstrated substantial temporal fluctuations throughout the week and has been correlated with length of stay.3,4 EHR interactions were presented as rates by dividing the number of patient chart accessions by the inpatient census for each hour. EHR interaction rates were assigned to one of three time periods: day (9:00 a.m. to 4:59 p.m.), morning/evening (7:00 a.m. to 8:59 a.m. and 5:00 p.m. to 7:59 p.m.), or night (8:00 p.m. to 6:59 a.m.).3,4 We determined the rate ratio of weekday to weekend EHR interactions per patient for each month by calculating the quotient of the mean number of EHR interactions per patient per hour for each time group.
Covariates included age, gender, race, insurance, admission source, clinical service, Charlson comorbidity score,21 admission day of the week, and service intensity weight (SIW). SIW is a relative measure of resources needed for a given All Patient Refined Diagnosis Related Group (APR-DRG) in the state of New York.22
Statistical Analysis
Baseline characteristics were presented as percentages or means with standard deviations, as appropriate. We used chi-squared tests and t tests to compare characteristics of patients across time.
The interrupted time series study was performed with each calendar month as the unit of time. We examined trends for 18 months prior to and 19 months following implementation of the intervention. The two months (November and December 2012) of storm-related hospital closure were considered to not have contributed to time in the model; i.e. January 2013 was treated analytically as the month following October 2012. Associations between the intervention and outcomes were analyzed using segmented regression analysis23–25 For the outcome of length of stay, a negative binomial model was fit, while for the outcomes of percent weekend discharges, 30-day readmission, and in-hospital mortality, logistic regression models were fit. In each model, we included three variables to measure the relationship of time and the outcome of interest: 1) a continuous time variable to represent the underlying temporal trends; 2) a dummy variable for the post-intervention period to determine the change in outcome related to the intervention; and 3) a continuous time variable, which began at the start of the intervention, to represent the change in slope.23–25 The coefficients of the latter two variables were of primary interest and indicated whether the intervention had an immediate or ongoing effect on the outcome of interest, respectively. Results for the relationships between time and outcomes were presented graphically using post-estimation adjustment for covariates.
We performed subgroup analyses for patients on the medicine and surgical services. Within the medicine service, we performed subgroup analyses of patients who were cared for by hospitalist physicians, who worked exclusively with inpatients and were employed by the hospital, or non-hospitalist physicians. Differences between the services were determined based on the coefficient for the interaction term.
Trends in the rate ratio of weekday to weekend EHR interactions were presented graphically to demonstrate changes across time. To help assess the validity of comparing this metric across two different EHRs, we presented the mean number of EHR interactions before and after the implementation of the new EHR at our hospital, which coincided with hospital reopening following Hurricane Sandy. Differences between the pre- and post-EHR implementation periods were compared using t tests.
RESULTS
Implementation of the components of the 7-Day Hospital Initiative occurred at various time points (Table 1). The increase in weekend staffing of hospitalists occurred on July 1, 2012, when the number of weekend hospitalists on staff increased from 6.5 to 12.5 full-time equivalents. Concurrently with this new staffing model, handoffs were redesigned such that the weekend hospitalist was included in rounds with the weekday hospitalist and resident team each Friday to review the plan for each patient at the bedside. The majority of new weekend social workers and care managers were hired around this time, but due to delays following hospital closure after Hurricane Sandy, the increase in care management staffing was not fully completed until early 2013 (Table 1). With the increased weekend staffing, physicians and care managers began to review the disposition of all patients on weekend mornings; previously, communication between these staff was infrequent and only occurred if a significant issue arose. Formal interdisciplinary rounds were introduced only at the end of the study period (Table 1).
The study included 57,163 hospitalizations, representing a total of 38,703 unique patients. Of these hospitalizations, 48.5 % were on the medicine service, 37.3 % were on surgical services, and 14.2 % were on other services (Table 2). The mean age of hospitalized adult patients was 61.4 years, 50.2 % of patients were female, and 9.9 % of patients were black. Although weekends represent 28.6 % of the week, only 13.1 % of all hospitalizations began with admission on a weekend day (Table 2).
Of the three full calendar years included in the study, 2011 contributed the greatest number of hospitalizations, which at least partly reflects hospital closure and the aftereffects of Hurricane Sandy during 2012 and 2013. The average (SD) census of included patients was 374.3 (47.5) before hospital closure and 301.4 (45.1) after hospital reopening; the census did not reach that of the pre-Sandy period until August 2013. Some differences were noted in patient characteristics across time. For instance, patients hospitalized during the post-Sandy period were more likely to be Medicaid beneficiaries and to have a higher Charlson comorbidity index, but lower service intensity weight, as compared to patients hospitalized during the pre-Sandy period. Hospitalizations during the post-Sandy period were also more likely to be on the surgical service and less likely to have begun on a weekend day (Table 2).
Prior to the intervention, there was an underlying trend of an increase in average length of stay of 1 % (95 % CI 1–2 %) per month (Table 3). Immediately following introduction of the intervention, overall hospital length of stay decreased by 13 % (95 % CI 10–15 %). This was followed by a continued decrease of 1 % per month as compared to the underlying time trend, or no change as compared to the new baseline following the introduction of the intervention (Fig. 1). Similar trends were observed on the medicine service, while reduced length of stay was not observed for surgery patients (Fig. 1). Results in trends of length of stay were similar between medicine patients on the hospitalist service versus non-hospitalist service, although the hospitalist service was associated with a smaller decrease in length of stay immediately following introduction of the intervention (0.91 [95 % CI 0.85–0.98] versus 0.82 [95 % CI 0.78–0.86], p = 0.02).
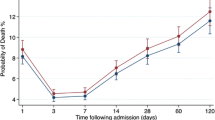
The percent of weekend discharges was 19.1 % in the pre-intervention period and 22.0 % in the post-intervention period. The proportion of weekend discharges increased by 12 % (95 % CI 2–22 %) at the time of the intervention and continued to increase by 2 % (95 % CI 1–3 %) per month thereafter (Table 3; Fig. 2). In 30-day readmissions, there was a nonsignificant decrease of 10 % (95 % CI −1 % to 19 %) at the time of the intervention, and no subsequent change. There were no significant changes in mortality during the study period (Table 3; Fig. 2). Trends in these secondary outcomes were generally similar between medicine and surgery services (p > 0.05 for differences between these services).
Monthly trends in secondary outcomes for all hospitalized patients: percent of discharges occurring on weekends, 30-day hospital readmission, and in-hospital mortality. July 2012 represents the beginning of the 7-Day Initiative. Data from November and December 2012 are missing due to hospital closure related to Hurricane Sandy.
The rate ratios of weekday to weekend EHR interactions decreased substantially after January 2013 (Fig. 3), the month in which a new EHR was implemented in our medical center. Furthermore, the overall number of EHR interactions significantly increased following implementation of the new EHR, from 2.8 (SD 1.4) to 4.4 (SD 1.7) per patient per hour (p < 0.001 for difference).
Trends in weekday to weekend electronic health record (EHR) interactions, a measure of hospital intensity of care, by month. Weekday to weekend EHR interaction comparisons were based on the following three work-hour periods: day (9:00 a.m. to 4:59 p.m.), morning/evening (7:00 a.m. to 8:59 a.m. and 5:00 p.m. to 7:59 p.m.), and night (8:00 p.m. to 6:59 a.m.).
DISCUSSION
The 7-Day Hospital Initiative, a multi-component initiative to increase hospital services on weekends, was associated with a sustained reduction in length of stay. However, this association must be interpreted in the context of concurrent hospital changes during the study period. Specifically, we were unable to determine the contribution of hospital closure due to Hurricane Sandy and the implementation of a new EHR to our findings. The 7-Day Hospital Initiative was also associated with an increase in the proportion of patients discharged on weekends, which likely contributed to the observed decrease in hospital length of stay. We did not detect an impact on clinical measures of 30-day readmission or in-hospital mortality.
Retrospective studies have noted differences in care and outcomes between weekends and weekdays.1–15 A number of prior analyses have suggested that the introduction of care components similar to elements in our intervention may lead to reductions in hospital length of stay. For instance, improved night and weekend physician coverage has been associated with reduced length of stay.26,27
In a real-world setting, the evaluation of the clinical impact of a hospital initiative can be challenging. Any findings regarding the effect of an intervention on care and clinical outcomes may be limited by various factors, including temporal changes in patient case mix, trends in care patterns and outcomes, and concurrent hospital initiatives, such as a new EHR, which may also affect outcomes. To help mitigate such concerns, we performed a time trend study, which accounts for secular trends, and adjusted for patient case mix.17
In addition to these relatively routine threats to validity, our hospital delivery system experienced two changes during the study period: a natural disaster and a new EHR. The biggest challenge to the validity of our analytic framework in this real-world study was the evacuation, shutdown, and phased reopening of the entire hospital in the wake of Hurricane Sandy. Our administration worked intently to be able to reopen only two months after the storm. However, the early “post-reopening” period differed from the “pre-closing” period in a number of respects. For instance, due to substantial damage, the emergency department was replaced by an urgent care center, which is not serviced by emergency medical services ambulances. The lack of a full-service emergency department contributed to the reduction in hospital volume and changes in case mix observed in the months after reopening. The decreased census in the post-Sandy period may have led to an improvement in patient flow through the hospital, with a resulting decreased length of stay that may have been independent of the intervention. Patients with extended hospital stays needed to be discharged when the hospital closed, and it took time to replenish this cohort after the hospital reopened. Our findings must be interpreted in the context of these differences in case mix, patient census, and hospital flow between pre-closing and post-closing periods.
We considered several analytic approaches to account for the closure. As an interrupted time series study considers that part of the effect of the intervention may be related to increased uptake over time, we decided on an approach to consider closure time as a time gap. In other words, we did not believe that the time of hospital closure would lead to further implementation or uptake of the initiative, although we were unable to measure the aggregate effect of closure on the effectiveness of the initiative.
The second change, while not a regular occurrence, is an example of a substantial alteration that may occur in any large hospital system. A new EHR was introduced during the study period, a system-level change which is increasingly common in hospital systems given the rapid expansion of EHRs nationally.28 At our hospital, this change may have had implications in care delivery through changes to workflow and the introduction of clinical decision support.29 As a result, our findings may have been influenced by the change in EHR. The possibility that the new EHR affected workflow is supported by findings that EHR interactions increased substantially after the introduction of the new EHR. In this study, we observed a substantial decrease in weekend to weekday variability in EHR interactions, a measure associated with intensity of care,3,4 following implementation of the initiative. However, because of the mid-study transition in our hospital-wide EHR platform, we were unable to determine the relative contribution of the 7-Day Hospital Initiative to these observed changes in EHR interactions.
Additional limitations of our study design deserve consideration in the interpretation of our findings. First, the initiative was implemented and evaluated at a single institution, and results may not be generalizable to other hospitals. Second, readmissions were counted only if they occurred at our hospital, which may have led to misclassification as a result of patients going to other hospitals. Third, we were unable to determine the effect of the intervention on important patient-reported outcomes such as quality of life and patient satisfaction. Fourth, we did not evaluate a number of intervention-related process measures, such as timing between ordering and the performance of diagnostic tests or evaluation of weekend discharge collaboration and communication. Fifth, we were unable to discern the relative effect of each component of the intervention on observed outcomes.
Our findings suggest that a multifaceted intervention designed to improve care on weekends may improve hospital throughput, though we did not detect an impact on clinical outcomes such as readmissions or mortality. This study also affords a look at the impact of a large-scale perturbation on an evaluation of the effectiveness of a system-level care improvement intervention in a real-world hospital setting. As Hurricane Sandy and the new EHR had effects on the implementation and possibly the outcomes of the intervention, studies evaluating similar interventions in other hospital systems are warranted.
References
Carey MR, Sheth H, Braithwaite RS. A prospective study of reasons for prolonged hospitalizations on a general medicine teaching service. J Gen Intern Med. 2005;20(2):108–15.
Selker HP, Beshansky JR, Pauker SG, Kassirer JP. The epidemiology of delays in a teaching hospital. The development and use of a tool that detects unnecessary hospital days. Med Care. 1989;27(2):112–29.
Blecker S, Austrian JS, Shine D, Braithwaite RS, Radford MJ, Gourevitch MN. Monitoring the pulse of hospital activity: Electronic health record utilization as a measure of care intensity. J Hosp Med. 2013;8(9):513–8.
Blecker S, Goldfeld K, Park N, et al. Electronic health record use, intensity of hospital care, and patient outcomes. Am J Med. 2014;127(3):216–21.
Bejanyan N, Fu AZ, Lazaryan A, et al. Impact of weekend admissions on quality of care and outcomes in patients with acute myeloid leukemia. Cancer. 2010;116(15):3614–20.
Jneid H, Fonarow GC, Cannon CP, et al. Impact of time of presentation on the care and outcomes of acute myocardial infarction. Circulation. 2008;117(19):2502–9.
Horwich TB, Hernandez AF, Liang L, et al. Weekend hospital admission and discharge for heart failure: association with quality of care and clinical outcomes. Am Heart J. 2009;158(3):451–8.
Kazley AS, Hillman DG, Johnston KC, Simpson KN. Hospital care for patients experiencing weekend vs weekday stroke: a comparison of quality and aggressiveness of care. Arch Neurol. 2010;67(1):39–44.
Kostis WJ, Demissie K, Marcella SW, Shao YH, Wilson AC, Moreyra AE. Weekend versus weekday admission and mortality from myocardial infarction. N Engl J Med. 2007;356(11):1099–109.
Becker DJ. Do hospitals provide lower quality care on weekends? Health Serv Res. 2007;42(4):1589–612.
Magid DJ, Wang Y, Herrin J, et al. Relationship between time of day, day of week, timeliness of reperfusion, and in-hospital mortality for patients with acute ST-segment elevation myocardial infarction. JAMA : J Am Med Assoc. 2005;294(7):803–12.
Aujesky D, Jimenez D, Mor MK, Geng M, Fine MJ, Ibrahim SA. Weekend versus weekday admission and mortality after acute pulmonary embolism. Circulation. 2009;119(7):962–8.
Bell CM, Redelmeier DA. Mortality among patients admitted to hospitals on weekends as compared with weekdays. N Engl J Med. 2001;345(9):663–8.
Gordon HS, Johnson ML, Wray NP, et al. Mortality after noncardiac surgery: prediction from administrative versus clinical data. Med Care. 2005;43(2):159–67.
James MT, Wald R, Bell CM, et al. Weekend hospital admission, acute kidney injury, and mortality. J Am Soc Nephrol : JASN. 2010;21(5):845–51.
Orszag P. Health care's lost weekend. The New York Times. 2010;Sect A:27.
Fan E, Laupacis A, Pronovost PJ, Guyatt GH, Needham DM. How to use an article about quality improvement. JAMA : J Am Med Assoc. 2010;304(20):2279–87.
Uppal A, Evans L, Chitkara N, et al. In search of the silver lining: the impact of Superstorm Sandy on Bellevue Hospital. Ann Am Thorac Soc. 2013;10(2):135–42.
Hartocollis A. NYU Langone Reopens for Surgery as Its Recovery Moves Ahead. New York Times; December 27, 2012: A22. Available at: http://www.nytimes.com/2012/12/28/nyregion/surgery-returns-to-nyu-langone-medical-center.html. Accessed March 25, 2015.
NYU Langone Medical Center Office of Communications and Marketing. NYU Langone Medical Center Today Resumes Additional Services, Opens New Urgent Care Center While Emergency Department Remains Temporarily Closed. Published January 14, 2013. Available at: http://nyulangone.org/press-releases/nyu-langone-medical-center-today-resumes-additional-services-opens-new-urgent-care-center-while-emergency-department-remains-temporarily-closed. Accessed March 25, 2015.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chron Dis. 1987;40(5):373–83.
New York State Department of Health. APR-DRG Weights. Available at: http://www.health.ny.gov/facilities/hospital/reimbursement/apr-drg/weights/ Accessed March 25, 2015.
Campbell SM, Reeves D, Kontopantelis E, Sibbald B, Roland M. Effects of pay for performance on the quality of primary care in England. N Engl J Med. 2009;361(4):368–78.
Morgan OW, Griffiths C, Majeed A. Interrupted time-series analysis of regulations to reduce paracetamol (acetaminophen) poisoning. PLoS Med. 2007;4(4):e105.
Wagner AK, Soumerai SB, Zhang F, Ross-Degnan D. Segmented regression analysis of interrupted time series studies in medication use research. J Clin Pharm Ther. 2002;27(4):299–309.
Nishisaki A, Pines JM, Lin R, et al. The impact of 24-hr, in-hospital pediatric critical care attending physician presence on process of care and patient outcomes*. Crit Care Med. 2012;40(7):2190–5.
St Noble VJ, Davies G, Bell D. Improving continuity of care in an acute medical unit: initial outcomes. QJM : Mon J Assoc Phys. 2008;101(7):529–33.
DesRoches CM, Charles D, Furukawa MF, et al. Adoption of electronic health records grows rapidly, but fewer than half of US hospitals had at least a basic system in 2012. Health Aff (Millwood). 2013;32(8):1478–85.
Bright TJ, Wong A, Dhurjati R, et al. Effect of clinical decision-support systems: a systematic review. Ann Intern Med. 2012;157(1):29–43.
Acknowledgments
Dr. Blecker was supported in part by the National Center for Advancing Translational Sciences (NCATS) grant KL2 TR000053.
Conflict of Interest
Dr. Braithwaite has acted as a paid consultant to evaluate the scientific rigor of Gilead’s internal mathematical modeling efforts. Dr. Braithwaite is currently a paid consultant to RTI for advising the Medical Device Innovation Consortium and to Engaged Public for advising health insurance plan design. All other authors declare no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Blecker, S., Goldfeld, K., Park, H. et al. Impact of an Intervention to Improve Weekend Hospital Care at an Academic Medical Center: An Observational Study. J GEN INTERN MED 30, 1657–1664 (2015). https://doi.org/10.1007/s11606-015-3330-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-015-3330-6