Abstract
BACKGROUND
Urine drug tests (UDTs) are recommended for patients on chronic opioid therapy (COT). Knowledge of the risk factors for aberrant UDT results could help optimize their use.
OBJECTIVE
To identify primary care COT patient and opioid regimen characteristics associated with aberrant UDT results.
DESIGN
Population-based observational.
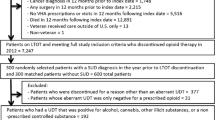
SAMPLE
5,420 UDTs for Group Health integrated group practice COT patients.
MEASURES
Group Health database measures of patient demographics, medical history, COT characteristics, and UDT results.
RESULTS
Thirty percent of UDTs had aberrant results, including prescribed opioid non-detection (12.3 %), tetrahydrocannabinol (THC; 11.2 %), non-prescribed opioid (5.3 %), illicit drug (excluding THC; 0.6 %), non-prescribed benzodiazepine (1.7 %), and dilute (4.8 %). Adjusted odds ratios (95 % CI) of any aberrant result were higher for males than females (1.24 [1.07, 1.43]), patients with versus without prior substance use disorder diagnoses (1.42 [1.17, 1.72]), and current smokers versus non-smokers (1.50 [1.30, 1.73]). Odds ratios were lower for patients aged 45–64 (0.77 [0.65, 0.92]) and 65+ (0.40 [0.32, 0.50]) versus patients aged 20–44 and for patients on long-acting opioids only (0.72 [0.55, 0.95]) or long-acting plus short-acting (0.67 [0.54, 0.83]) versus short-acting only. Adjusted odds of prescribed opioid non-detection were lower for patients aged 45–64 (0.79 [0.63, 0.998]) and 65+ (0.44 [0.32, 0.59]) versus patients aged 20–44, for those on 40–<120 mg daily morphine-equivalent dose (0.52 [0.39, 0.70]) or 120+ mg (0.22 [0.11, 0.43]) versus <40 mg, and for patients on long-acting (0.35 [0.21, 0.57]) or long-acting plus short-acting (0.35 [0.24, 0.50]) opioids (versus short-acting only); and odds ratios were higher for patients with versus without prior diagnoses of substance use disorder (1.70 [1.31, 2.20]).
CONCLUSIONS
In this primary care setting, results were aberrant for 30 % of UDTs of COT patients, largely because of prescribed opioid non-detection and THC. Aberrant results of almost all types were more likely among patients under the age of 45. Other risk factors varied across aberrancies, but commonly included current smoking and prior substance use disorder diagnosis.
Similar content being viewed by others
REFERENCES
Kirschner N, Ginsburg J, Sulmasy LS. Prescription drug abuse: a policy position paper from the American College of Physicians. Ann Intern Med. 2014;160:198–200.
Starrels JL, Becker WC, Alford DP, Kapoor A, Williams A, Turner BJ. Systematic review: treatment agreements and urine drug testing to reduce opioid misuse in patients with chronic pain. Ann Intern Med. 2010;152:712–20.
Warner M, Chen LH, Makuc DM, Anderson RN, Minino AM. Drug poisoning deaths in the United States, 1980–2008. NCHS data brief, no. 81. National Center for Health Statistics. 2011 [Accessed August 13, 2014]. Available at: http://www.cdc.gov/nchs/data/databriefs/db81.htm.
Starrels J, Becker W, Weiner M, Li X, Heo M, Turner B. Low use of opioid risk reduction strategies in primary care even for high risk patients with chronic pain. J Gen Intern Med. 2011;26:958–64.
Bohnert ASB, Valenstein M, Bair MJ, et al. Association between opioid prescribing patterns and opioid overdose-related deaths. JAMA. 2011;305(13):1315–21.
Volkow ND, McLellan TA. Curtailing diversion and abuse of opioid analgesics without jeopardizing pain treatment. JAMA. 2011;305(13):1346–7.
Rolfs RT, Johnson E, Williams NJ, Sundwall DN. Utah Clinical Guidelines on Prescribing Opioids for Treatment of Pain. J Pain Palliat Care Pharmacother. 2010;24(3):219–35.
Chou R, Fanciullo GJ, Fine PG, et al. Clinical guidelines for the use of chronic opioid therapy in chronic noncancer pain. J Pain. 2009;10(2):113–30.
Manchikanti L, Abdi S, Atluri S, et al. American Society of Interventional Pain Physicians (ASIPP) Guidelines for Responsible Opioid Prescribing in Chronic Non-Cancer Pain: Part 2-Guidance. Pain Physician. 2012;15:S67-S116.
Department of Veterans Affairs, Department of Defense. VA/DoD Clinical practice guideline for management of opioid therapy for chronic pain. Department of Veterans Affairs, Department of Defense. 2010 [Accessed August 13, 2014]. Available at: http://www.healthquality.va.gov/guidelines/Pain/cot/.
Nuckols TK, Anderson L, Popescu I, et al. Opioid prescribing: a systematic review and critical appraisal of guidelines for chronic pain. Ann Intern Med. 2014;160:38–47.
Peppin JF, Passik SD, Couto JE, et al. Recommendations for urine drug monitoring as a component of opioid therapy in the treatment of chronic pain. Pain Med. 2012;13:886–96.
Colorado Division of Workers’ Compensation. Chronic Pain Disorder Medical Treatment Guidelines 2011 [Accessed August 13, 2014]. Available at: http://www.colorado.gov/cs/Satellite?blobcol=urldata&blobheader=application%2Fpdf&blobkey=id&blobtable=MungoBlobs&blobwhere=1251894637011&ssbinary=true.
Kahan M, Mailis-Gagnon A, Wilson L, Srivastava A. Canadian guideline for safe and effective use of opioids for chronic noncancer pain: clinical summary for family physicians. Part 1: general population. Can Fam Physician. 2011;57:1269–76.
Turner JA, Saunders K, Shortreed SM, et al. Chronic opioid therapy risk reduction initiative: impact on urine drug testing rates and results. J Gen Intern Med. 2014;29:305–11.
Couto JE, Romney MC, Leider HL, Sharma S, Goldfarb NI. High rates of inappropriate drug use in the chronic pain population. Popul Health Manag. 2009;12(4):185–90.
Manchikanti L, Manchukonda R, Pampati V, et al. Does random urine drug testing reduce illicit drug use in chronic pain patients receiving opioids? Pain Physician. 2009;9(2):123–9.
Michna E, Jamison RN, Pham L-D, et al. Urine toxicology screening among chronic pain patients on opioid therapy: frequency and predictability of abnormal findings. Clin J Pain. 2007;23:173–9.
Morasco BJ, Duckart JP, Dobscha SK. Adherence to clinical guidelines for opioid therapy for chronic pain in patients with substance use disorder. J Gen Intern Med. 2011;26(9):965–71.
Morasco BJ, Duckart JP, Carr TP, Deyo RA, Dobscha SK. Clinical characteristics of veterans prescribed high doses of opioid medications for chronic non-cancer pain. Pain. 2010;151:625–32.
Trescott CE, Beck RM, Seelig MD, Von Korff M. Group Health’s initiative to avert opioid misuse and overdose among patients with chronic noncancer pain. Health Aff. 2011;30:1420–4.
Turk DC, Swanson KS, Gatchel RJ. Predicting opioid misuse by chronic pain patients: a systematic review and literature synthesis. Clin J Pain. 2008;24:497–508.
Ives T, Chelminski P, Hammett-Stabler C, et al. Predictors of opioid misuse in patients with chronic pain: a prospective cohort study. BMC Health Services Research. 2006;6(1):46.
Katz NP, Sherburne S, Beach M, et al. Behavioral monitoring and urine toxicology testing in patients receiving long-term opioid therapy. Anesthesia & Analgesia. 2003;97:1097–102.
Edlund MJ, Steffick D, Hudson T, Harris KM, Sullivan M. Risk factors for clinically recognized opioid abuse and dependence among veterans using opioids for chronic non-cancer pain. Pain. 2007;129(3):355–62.
Reid MC, Engles-Horton LL, Weber MB, Kerns RD, Rogers EL, O’Connor PG. Use of opioid medications for chronic noncancer pain syndromes in primary care. J Gen Intern Med. 2002;17:173–9.
White AG, Birnbaum HG, Schiller M, Tang J, Katz NP. Analytic models to identify patients at risk for prescription opioid abuse. Am J Manag Care. 2009;15:897–906.
Sullivan MD, Edlund MJ, Fan M-Y, DeVries A, Brennan Braden J, Martin BC. Risks for possible and probable opioid misuse among recipients of chronic opioid therapy in commercial and Medicaid insurance plans: The TROUP Study. Pain. 2010;150(2):332–9.
Edlund MJ, Martin BC, Fan M-Y, Devries A, Braden JB, Sullivan MD. Risks for opioid abuse and dependence among recipients of chronic opioid therapy: Results from the TROUP Study. Drug Alcohol Depend. 2010;112(1–2):90–8.
Michna E, Ross EL, Hynes WL, et al. Predicting aberrant drug behavior in patients treated for chronic pain: importance of abuse history. J Pain Symptom Manage. 2004;28(3):250–8.
Wasan AD, Butler SF, Budman SH, Benoit C, Fernandez K, Jamison RN. Psychiatric history and psychologic adjustment as risk factors for aberrant drug-related behavior among patients with chronic pain. Clin J Pain. 2007;23:307–15.
Liebschutz JM, Saitz R, Weiss RD, et al. Clinical factors associated with Prescription Drug Use Disorder in urban primary care patients with chronic pain. J Pain. 2010;11(11):1047–55.
Akbik H, Butler SF, Budman SH, Fernandez K, Katz NP, Jamison RN. Validation and clinical application of the Screener and Opioid Assessment for Patients with Pain (SOAPP). J Pain Symptom Manage. 2006;32(3):287–93.
Public Health Service and Health Care Financing Administration. International classification of diseases, 9th revision, clinical modification. Washington, D. C.: Public Health Service; 1980.
Elixhauser A, Steiner C, Palmer L. Clinical Classifications Software (CCS), 2014. U.S. Agency for Healthcare Research and Quality. 2013 [Accessed August 13, 2014]. Available at: http://www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp.
Wiley LK, Shah A, Xu H, Bush WS. ICD-9 tobacco use codes are effective identifiers of smoking status. J Am Med Inform Assoc. 2013;20(4):652–8.
Raebel MA, Newcomer SR, Reifler LM, et al. Chronic use of opioid medications before and after bariatric surgery. JAMA. 2013;310(13):1369–76.
Von Korff M, Saunders K, Ray GT, et al. De facto long-term opioid therapy for noncancer pain. Clin J Pain. 2008;24:521–7.
Carson S, Thakurta S, Low A, Smith B, Chou R. Drug class review: long-acting opioid analgesics: Final Update 6 Report. Portland, OR: Oregon Health & Science University. 2011 [Accessed August 13, 2014]. Available at: http://www.ncbi.nlm.nih.gov/books/NBK62335/.
McCullagh P, Nelder JA. Generalized Linear Models. London: Chapman & Hall; 1989.
Liang JK-Y, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73:13–22.
Zeger SL, Liang JK-Y. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42:121–30.
Substance Abuse and Mental Health Services Administration. Results from the 2012 National Survey on Drug Use and Health: Summary of national findings. NSDUH Series H-46, HHS Publication No. (SMA) 13–4795. Rockville, MD: Substance Abuse and Mental Health Services Administration. 2013 [Accessed August 13, 2014]. Available at: http://www.samhsa.gov/data/NSDUH/2012SummNatFindDetTables/NationalFindings/NSDUHresults2012.htm.
Berg CJ, Wen H, Cummings JR, Ahluwalia JS, Druss BG. Depression and substance abuse and dependency in relation to current smoking status and frequency of smoking among nondaily and daily smokers. Am J Addict. 2013;22:581–9.
Fuster D, Cheng DM, Allensworth-Davies D, Palfai TP, Samet JH, Saitz R. No detectable association between frequency of marijuana use and health or healthcare utilization among primary care patients who screen positive for drug use. J Gen Intern Med. 2014;29:133–9.
Gudin JA, Mogali S, Jones JD, Comer SD. Risks, management, and monitoring of combination opioid, benzodiazepines, and/or alcohol use. Postgrad Med. 2013;125:115–30.
Chaturvedi AK, Sershon JL, Craft KJ, et al. Effects of fluid load on human urine characteristics related to workplace drug testing. J Anal Toxicol. 2013;37(1):5–10.
Saunders KW, Davis RL, Stergachis A. Group Health Cooperative. In: Strom B, editor. Pharmacoepidemiology. 4th ed. West Sussex, England: John Wiley and Sons; 2005. p. 223–39.
Chou R, Ballantyne JC, Fanciullo GJ, Fine PG, Miaskowski C. Research gaps on use of opioids for chronic noncancer pain: findings from a review of the evidence for an American Pain Society and American Academy of Pain Medicine Clinical Practice Guideline. J Pain. 2009;10(2):147–59.
Chou R, Fanciullo GJ, Fine PG, Miaskowski C, Passik SD, Portenoy RK. Opioids for chronic noncancer pain: prediction and identification of aberrant drug-related behaviors: a review of the evidence for an American Pain Society and American Academy of Pain Medicine Clinical Practice Guideline. J Pain. 2009;10(2):131–46.
Dupouy J, Mémier V, Catala H, Lavit M, Oustric S, Lapeyre-Mestre M. Does urine drug abuse screening help for managing patients? A systematic review. Drug Alcohol Depend. 2014;136:11–20.
Acknowledgments
Contributors
The authors thank Ryan N. Hansen, PharmD, PhD, RPh, and Stephen Thielke, MD, for helpful contributions to this work.
Funders
Funding for this research was provided by NIH grant 1R01 AG034181 from the National Institutes of Health National Institute on Aging. The findings and conclusions do not necessarily represent the views of Group Health.
Prior Presentation
Preliminary results of this study were presented in a poster at the annual meeting of the American Pain Society in Tampa, Florida, in May 2014 (Turner JA, Saunders K, Shortreed SM, LeResche L, Von Korff M.: Chronic opioid therapy urine drug testing in primary care: Rates and predictors of aberrant results.).
Conflict of Interest
Dr. Von Korff is the principal investigator of research grants awarded to the Group Health Research Institute from Pfizer. These grants also support Ms. Saunders. Dr. Shortreed served as a biostatistician on a grant to Group Health Research Institute from Bristol-Myers Squibb. Ms. Saunders owns stock in Merck. The other authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Turner, J.A., Saunders, K., Shortreed, S.M. et al. Chronic Opioid Therapy Urine Drug Testing in Primary Care: Prevalence and Predictors of Aberrant Results. J GEN INTERN MED 29, 1663–1671 (2014). https://doi.org/10.1007/s11606-014-3010-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-014-3010-y