ABSTRACT
BACKGROUND
The Accreditation Council for Graduate Medical Education (ACGME) implemented duty hour regulations for residents in 2003 and again in 2011. While previous studies showed no systematic impacts in the first 2 years post-reform, the impact on mortality in subsequent years has not been examined.
OBJECTIVE
To determine whether duty hour regulations were associated with changes in mortality among Medicare patients in hospitals of different teaching intensity after the first 2 years post-reform.
DESIGN
Observational study using interrupted time series analysis with data from July 1, 2000 to June 30, 2008. Logistic regression was used to examine the change in mortality for patients in more versus less teaching-intensive hospitals before (2000–2003) and after (2003–2008) duty hour reform, adjusting for patient comorbidities, time trends, and hospital site.
PATIENTS
Medicare patients (n = 13,678,956) admitted to short-term acute care non-federal hospitals with principal diagnoses of acute myocardial infarction (AMI), gastrointestinal bleeding, or congestive heart failure (CHF); or a diagnosis-related group (DRG) classification of general, orthopedic, or vascular surgery.
MAIN MEASURE
All-location mortality within 30 days of hospital admission.
KEY RESULTS
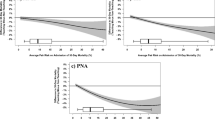
In medical and surgical patients, there were no consistent changes in the odds of mortality at more vs. less teaching intensive hospitals in post-reform years 1–3. However, there were significant relative improvements in mortality for medical patients in the fourth and fifth years post-reform: Post4 (OR 0.88, 95 % CI [0.93–0.94]); Post5 (OR 0.87, [0.82–0.92]) and for surgical patients in the fifth year post-reform: Post5 (OR 0.91, [0.85–0.96]).
CONCLUSIONS
Duty hour reform was associated with no significant change in mortality in the early years after implementation, and with a trend toward improved mortality among medical patients in the fourth and fifth years. It is unclear whether improvements in outcomes long after implementation can be attributed to the reform, but concerns about worsening outcomes seem unfounded.

Similar content being viewed by others
REFERENCES
Kohn LT, Corrigan JM, Donaldson MS. To Err is Human: Building a Safer Health System. Washington: National Academy Press; 2000.
Accreditation Council for Graduate Medical Education. Resident duty hours language: Final requirements. 2003; http://www.acgme.org. Accessed February 18, 2013.
Accreditation Council for Graduate Medical Education. Report of the work group on resident duty hours and the learning environment. June 11, 2002. In: The ACGME’s approach to limit resident duty hours 12 months after implementation: a summary of achievements, 2004. 2006; http://www.acgme.org/acgmeweb/Portals/0/PFAssets/PublicationsPapers/dh_dutyhoursummary2003–04.pdf. Accessed February 18, 2013.
Volpp KG, Rosen AK, Rosenbaum PR, et al. Mortality among hospitalized Medicare beneficiaries in the first 2 years following ACGME resident duty hour reform. JAMA. 2007;298(9):975–83.
Volpp KG, Rosen AK, Rosenbaum PR, et al. Mortality among patients in VA hospitals in the first 2 years following ACGME resident duty hour reform. JAMA. 2007;298(9):984–92.
Shetty KD, Bhattacharya J. Changes in hospital mortality associated with residency work-hour regulations. Ann Intern Med. 2007;147(2):73–80.
Volpp KG, Rosen AK, Rosenbaum PR, et al. Did duty hour reform lead to better outcomes among the highest risk patients? J Gen Intern Med. 2009;24(10):1149–55.
Rosen AK, Loveland SA, Romano PS, et al. Effects of resident duty hour reform on surgical and procedural patient safety indicators among hospitalized Veterans Health Administration and Medicare patients. Med Care. 2009;47(7):723–31.
Press MJ, Silber JH, Rosen AK, et al. The impact of resident duty hour reform on hospital readmission rates among Medicare beneficiaries. J Gen Intern Med. 2011;26(4):405–11.
Silber JH, Rosenbaum PR, Rosen AK, et al. Prolonged hospital stay and the resident duty hour rules of 2003. Med Care. 2009;47(12):1191–200.
Nasca TJ, Day SH, Amis ES, Jr. The new recommendations on duty hours from the ACGME Task Force. N Engl J Med. 2010.
Croasdale M. Johns Hopkins Penalized for Resident Hour Violations. 2003; http://www.ama-assn.org/amednews/2003/09/15/prsc0915.htm. Accessed February 18, 2013.
Killelea BK, Chao L, Scarpinato V, Wallack MK. The 80-hour workweek. Surg Clin N Am. 2004;84(6):1557–72, x.
Fletcher KE, Reed DA, Arora VM. Patient safety, resident education and resident well-being following implementation of the 2003 ACGME duty hour rules. J Gen Intern Med. 2011;26(8):907–19.
Moonesinghe SR, Lowery J, Shahi N, Millen A, Beard JD. Impact of reduction in working hours for doctors in training on postgraduate medical education and patients’ outcomes: systematic review. BMJ (Clin Res Ed). 2011;342:d1580.
Iezzoni LI. Risk Adjustment for Measuring Health-care Outcomes. 3rd ed. Chicago: Health Administration Press; 2003.
Rockall TA, Logan RF, Devlin HB, Northfield TC. Variation in outcome after acute upper gastrointestinal haemorrhage. The National Audit of Acute Upper Gastrointestinal Haemorrhage. Lancet. 1995;346(8971):346–50.
Agency for Healthcare Research and Quality. Inpatient Quality Indicators Download. AHRQ Quality Indicators. 2007; http://www.qualityindicators.ahrq.gov/downloads/software/sas/v21r4/iqi_guide_rev4.pdf Accessed February 18, 2013.
Second Report of the California Hospitals Outcomes Project. Acute Myocardial Infarction 1996; http://repositories.cdlib.org/chsrpc/coshpd/index.html#1996. Accessed February 18, 2013.
Iezzoni LI, Burnside S, Sickles L, Moskowitz MA, Sawitz E. Coding of acute myocardial infarction: clinical policy and implications. Ann Intern Med. 1988;109:745–51.
Kiyota Y, Schneeweiss S, Glynn RJ, Cannuscio CC, Avorn J, Solomon DH. Accuracy of Medicare claims-based diagnosis of acute myocardial infarction: estimating positive predictive value on the basis of review of hospital records. Am Hear J. 2004;148(1):99–104.
Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27.
Lawthers AG, McCarthy EP, Davis RB, Petersen LE, Palmer RH, Iezzoni LI. Identification of in-hospital complications from claims data: is it valid? Med Care. 2000;38(8):785–95.
Keeler EB, Rubenstein LV, Kahn KL, et al. Hospital characteristics and quality of care. JAMA. 1992;268(13):1709–14.
Allison JJ, Kiefe CI, Weissman NW, et al. Relationship of hospital teaching status with quality of care and mortality for Medicare patients with acute MI. JAMA. 2000;284(10):1256–62.
Taylor DH, Whellan DJ, Sloan FA. Effects of admission to a teaching hospital on the cost and quality of care for Medicare beneficiaries. N Engl J Med. 1999;340(4):293–9.
Campbell DT, Stanley JC. Experimental and Quasi-Experimental Designs for Research. Dallas: Houghton Mifflin Company; 1963.
Shadish WR, Cook TD, Campbell DT. Experimental and Quasi-Experimental Designs for Generalized Causal Inference. Boston: Houghton-Mifflin; 2002.
Rosenbaum PR. Stability in the absence of treatment. J Am Stat Assoc. 2001;96:210–9.
Field C, Welsh A. Bootstrapping clustered data. J R Stat Soc Ser B Methodol. 2007;69:369–90.
CMS. Fiscal year 2009 quality measure reporting for 2010 payment update 2009; https://www.cms.gov/HospitalQualityInits/downloads/HospitalRHQDAPU200808.pdf. Accessed February 18, 2013.
CMS. Premier Hospital Quality Incentive Demonstration. 2011; https://www.cms.gov/HospitalQualityInits/35_HospitalPremier.asp. Accessed February 18, 2013.
RAC. Critical access hospital (CAH) frequently asked questions. Health and human services information for rural America 2011; http://www.raconline.org/topics/hospitals/cahfaq.php. Accessed February 18, 2013.
Landrigan CP, Barger LK, Cade BE, Ayas NT, Czeisler CA. Interns’ compliance with accreditation council for graduate medical education work-hour limits. JAMA. 2006;296(9):1063–70.
Accreditation Council for Graduate Medical Education. The ACGME’s approach to limit resident duty hours 12 months after implementation: A summary of achievements, 2004. 2006; http://www.acgme.org/acgmeweb/Portals/0/PFAssets/PublicationsPapers/dh_dutyhoursummary2003-04.pdf. Accessed February 18, 2013.
Pellegrini VD Jr, Peabody T, Dinges DF, Moody J, Fabri PJ. Symposium resident work-hour guidelines. A sentence or an opportunity for orthopaedic education? J Bone Joint Surg Am. 2005;87(11):2576–86.
Acknowledgements
This work was funded by grant R01 HL094593-01 from the NHLBI.
Conflict of Interest
The sponsors/funders have had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript. There are no known financial conflicts of interest among any of the authors, including but not limited to employment/affiliation, grants or funding, honoraria, paid consultancies, expert testimony, stock ownership or options, and patents filed, received or pending. Both Dr. Volpp and Dr. Bellini served as unpaid members of the Committee on Innovations for the ACGME from 2005 to 2009.
Author information
Authors and Affiliations
Corresponding author
APPENDIX
APPENDIX
Rights and permissions
About this article
Cite this article
Volpp, K.G., Small, D.S., Romano, P.S. et al. Teaching Hospital Five-Year Mortality Trends in the Wake of Duty Hour Reforms. J GEN INTERN MED 28, 1048–1055 (2013). https://doi.org/10.1007/s11606-013-2401-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-013-2401-9