ABSTRACT
BACKGROUND
Increasingly, medical school policies limit pharmaceutical representatives’ access to students and gifts from drugmakers, but little is known about how these policies affect student attitudes toward industry.
OBJECTIVE
To assess interactions between trainees and the pharmaceutical industry, and to determine whether learning environment characteristics influence students’ practices and attitudes.
DESIGN, PARTICIPANTS
We conducted a cross-sectional survey with a nationally-representative sample of first- and fourth-year medical students and third-year residents, stratified by medical school, including ≥ 14 randomly selected trainees at each level per school.
MAIN MEASURES
We measured frequency of industry interactions and attitudes regarding how such interactions affect medical training and the profession. Chi-squared tests assessed bivariate linear trend, and hierarchical logistic regression models were fitted to assess associations between trainees’ attitudes and their schools’ National Institutes of Health (NIH) funding levels and American Medical Student Association (AMSA) PharmFree Scorecard grades reflecting industry-related conflict of interest policies.
KEY RESULTS
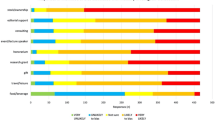
Among 1,610 student (49.3 % response rate) and 739 resident (43.1 %) respondents, industry-sponsored gifts were common, rising from 33.0 % (first-year students) to 56.8 % (fourth-year students) and 54 % (residents) (p < 0.001). These gifts included meals outside the hospital (reported by 5 % first-year students, 13.4 % fourth-year students, 27.5 % residents (p < 0.001)) and free drug samples (reported by 7.4 % first-year students, 14.1 % fourth-year students, 14.3 % residents (p < 0.001)). The perception that industry interactions lead to bias was prevalent, but the belief that physicians receive valuable education through these interactions increased (64.1 % to 67.5 % to 79.8 %, p < 0.001). Students in schools receiving more NIH funding reported industry gifts less often (OR = 0.51, 95 % CI: 0.38–0.68, p < 0.001), but the strength of institutional conflict of interest policies was not associated with this variable.
CONCLUSIONS
Despite recent policy changes, a substantial number of trainees continue to receive gifts from pharmaceutical representatives. We found no relation between these outcomes and a school’s policies concerning interactions with industry.

Similar content being viewed by others
REFERENCES
Brody H. Pharmaceutical industry financial support for medical education: benefit, or undue influence? J Law Med Ethics. 2009;37(3):451–460.
Campbell EG, Regan S, Gruen RL, Ferris TG, Rao SR, Cleary PD, Blumenthal D. Professionalism in medicine: results of a national survey of physicians. Ann Intern Med. 2007;147(11):795–802.
Steinbrook R. Future directions in industry funding of continuing medical education. Arch Intern Med. 2011;171(3):257–258.
Avorn J, Choudhry NK. Funding for medical education: maintaining a healthy separation from industry. Circulation. 2010;121(20):2228–2234.
Campbell EG, Weissman JS, Ehringhaus S, Rao SR, Moy B, Feibelmann S, Goold SD. Institutional academic industry relationships. JAMA. 2007;298(15):1779–1786.
Zipkin DA, Steinman MA. Interactions between pharmaceutical representatives and doctors in training. A thematic review. J Gen Intern Med. 2005;20(8):777–786.
Fitz M, Homna D, Reddy S, Griffith C, Baker E, et al. The hidden curriculum: medical students’ changing opinions toward the pharmaceutical industry. Acad Med. 2007;82:S1–S3.
Bellin M, McCarthy S, Drevlow L, Pierach C. Medical students’ exposure to pharmaceutical industry marketing: a survey at one U.S. medical school. Acad Med. 2004;79:1041–1045.
Hyman P, Hochman M, Shaw J, Steinman M. Attitudes of preclinical and clinical medical students toward interactions with the pharmaceutical industry. Acad Med. 2007;82:94–99.
Fein E, Vermillion M, Uijtdehaag S. Pre-clinical medical students’ exposure to and attitudes toward pharmaceutical industry marketing. Med Educ. Online 2007;12. Available at: http://www.med-ed-online.net/index.php/meo/article/viewArticle/4465.
Sierles FS, Brodkey AC, Cleary LM, McCurdy FA, Mintz M, Frank J, Lynn DJ, Chao J, Morgenstern BZ, Shore W, Woodard JL. Medical students’ exposure to and attitudes about drug company interactions: a national survey. JAMA. 2005;294(9):1034–1042.
Soyk C, Pfefferkorn B, McBride P, Rieselbach R. Medical student exposure to and attitudes about pharmaceutical companies. WMJ. 2010;109(3):142–148.
Austad KE, Avorn J, Kesselheim AS. Medical students’ exposure to and attitudes about the pharmaceutical industry: a systematic review. PLoS Med. 2011;8(5):e1001037.
Wazana A. Physicians and the pharmaceutical industry: is a gift ever just a gift? JAMA. 2000;283(3):373–380.
Bowman MA, Pearle DL. Changes in drug prescribing patterns related to commercial company funding of continuing medical education. J Contin Educ Health Prof. 1988;8:13–20.
Sondergaard J, Vach K, Kragstrup J, Andersen M. Impact of pharmaceutical representative visits on GPs’ drug preferences. Fam Pract. 2009;26:204–209.
Institute of Medicine. Conflict of interest in medical research, education, and practice. Washington, D.C.: National Academies Press; 2009.
Association of American Medical Colleges. Industry funding of medical education: report of an AAMC task force. June 2008. Available at: https://members.aamc.org/eweb/upload/Industry%20Funding%20of%20Medical%20Education.pdf. Accessed 14 Jan 2013.
Stanford School of Medicine. New policy on continuing medical education. 19 Aug 2008. Available at: http://med.stanford.edu/coi/documents/deanpizzo_cmeletter.pdf. Accessed 14 Jan 2013.
Pharmaceutical Research and Manufacturers of America. PhRMA code on interactions with healthcare professionals. July 2008. Available at: http://www.phrma.org/sites/default/files/369/phrma_marketing_code_2008-1.pdf . Accessed 14 Jan 2013.
University of Iowa health care conflict of interests and conflict of commitment policy regarding interactions with industry. 20 January 2009. Available at: http://www.healthcare.uiowa.edu/cme/planning/documents/FinalCOIPolicy.pdf. Accessed 14 Jan 2013.
Fugh-Berman A, Brown SR, Trippett R, Bell AM, Clark P, Fleg A, Siwek J. Closing the door on pharma? A national survey of family medicine residencies regarding industry interactions. Acad Med. 2011;86(5):649–654.
Kao AC, Braddock C 3rd, Clay M, Elliott D, Epstein SK, Filstead W, Hotze T, May W, Reenan J. Effect of educational interventions and medical school policies on medical students’ attitudes toward pharmaceutical marketing practices: a multi-institutional study. Acad Med. 2011;86(11):1454–1462.
Weissman JS, Betancourt J, Campbell EG, Park ER, Kim M, Clarridge B, Blumenthal D, Lee KC, Maina AW. Resident physicians' preparedness to provide cross-cultural care. JAMA. 2005;294(9):1058–1067.
US News. Best medical schools: research. 2011. Available at: http://grad-schools.usnews.rankingsandreviews.com/best-graduate-schools/top-medical-schools/research-rankings. Accessed 14 Jan 2013.
American Association for Public Opinion Research. Standard definitions: final dispositions of case codes and outcome rates for surveys. 2009. Available at: http://www.aapor.org/AM/Template.cfm?Section=Standard_Definitions1&Template=/CM/ContentDisplay.cfm&ContentID=1814. Accessed 14 Jan 2013.
Johnson TP, Wislar JS. Response rates and nonresponse errors in surveys. JAMA. 2012;307(17):1805–1806.
Kesselheim AS, Mello MM, Studdert DM. Strategies and practices in off-label marketing of pharmaceuticals: a retrospective analysis of whistleblower complaints. PLoS Med. 2011;8(4):e1000431.
Mullan F, Chen C, Petterson S, Kolsky G, Spagnola M. The social mission of medical education: ranking the schools. Ann Intern Med. 2010;152(12):804–811.
Chimonas S, Brennan TA, Rothman DJ. Physicians and drug representatives: exploring the dynamics of the relationship. J Gen Intern Med. 2007;22(2):184–190.
Chren M-M, Landefeld CS. Physicians’ behavior and their interactions with drug companies: a controlled study of physicians who requested additions to a hospital drug formulary. JAMA. 1994;271:684–689.
Manchanda P, Honka E. The effects and role of direct-to-physician marketing in the pharmaceutical industry: an integrative review. Yale J Health Policy Law Ethics. 2005;5:785–812.
Avorn J, Chen M, Hartley R. Scientific versus commercial sources of influence on the prescribing behavior of physicians. Am J Med. 1982;73(1):4–8.
Agrawal S, Saluja I, Kaczorowski J. A prospective before-and-after trial of an educational intervention about pharmaceutical marketing. Acad Med. 2004;79:1046–1050.
Austad KE, Kesselheim AS. Conflict of interest disclosure in early medical education: should medical students stay in the dark? JAMA. 2011;306:991–992.
Asch DA, Jedrziewski MK, Christakis NA. Response rates to mail surveys published in medical journals. J Clin Epidemiol. 1997;50(10):1129–1136.
Acknowledgements
The authors would like to thank Prof. Lawrence Lessig of Harvard Law School for his helpful comments on the study, and to acknowledge useful input from members of the Research Ethics Program of the Harvard Clinical and Translational Science Center. Study funded by a grant from the Edmond J. Safra Center for Ethics at Harvard University. Dr. Kesselheim is supported by a career development award from the Agency for Healthcare Research & Quality (K08HS18465-01), and a Robert Wood Johnson Foundation Investigator Award in Health Policy Research. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Conflict of Interest
The authors declare that they do not have a conflict of interest. Ms. Austad reports being a member of the American Medical Student Association (AMSA) and has received funding to support travel and lodging to attend AMSA conferences.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(PDF 105 kb)
Rights and permissions
About this article
Cite this article
Austad, K.E., Avorn, J., Franklin, J.M. et al. Changing Interactions Between Physician Trainees and the Pharmaceutical Industry: A National Survey. J GEN INTERN MED 28, 1064–1071 (2013). https://doi.org/10.1007/s11606-013-2361-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-013-2361-0