Abstract
BACKGROUND
The contribution of masculinity to men’s healthcare use has gained increased public health interest; however, few studies have examined this association among African-American men, who delay healthcare more often, define masculinity differently, and report higher levels of medical mistrust than non-Hispanic White men.
OBJECTIVE
To examine associations between traditional masculinity norms, medical mistrust, and preventive health services delays.
DESIGN AND PARTICIPANTS
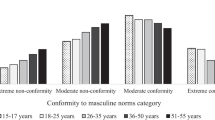
A cross-sectional analysis using data from 610 African-American men age 20 and older recruited primarily from barbershops in the North, South, Midwest, and West regions of the U.S. (2003-2009).
MEASUREMENTS
Independent variables were endorsement of traditional masculinity norms around self-reliance, salience of traditional masculinity norms, and medical mistrust. Dependent variables were self-reported delays in three preventive health services: routine check-ups, blood pressure screenings, and cholesterol screenings. We controlled for socio-demography, healthcare access, and health status.
RESULTS
After final adjustment, men with a greater endorsement of traditional masculinity norms around self-reliance (OR: 0.77; 95% CI: 0.60–0.98) were significantly less likely to delay blood pressure screening. This relationship became non-significant when a longer BP screening delay interval was used. Higher levels of traditional masculinity identity salience were associated with a decreased likelihood of delaying cholesterol screening (OR: 0.62; 95% CI: 0.45–0.86). African-American men with higher medical mistrust were significantly more likely to delay routine check-ups (OR: 2.64; 95% CI: 1.34–5.20), blood pressure (OR: 3.03; 95% CI: 1.45–6.32), and cholesterol screenings (OR: 2.09; 95% CI: 1.03–4.23).
CONCLUSIONS
Contrary to previous research, higher traditional masculinity is associated with decreased delays in African-American men’s blood pressure and cholesterol screening. Routine check-up delays are more attributable to medical mistrust. Building on African-American men’s potential to frame preventive services utilization as a demonstration, as opposed to, denial of masculinity and implementing policies to reduce biases in healthcare delivery that increase mistrust, may be viable strategies to eliminate disparities in African-American male healthcare utilization.
Similar content being viewed by others
References
Cherry DK, Woodwell DA, Rechtsteiner EA. National Ambulatory Medical Care Survey: 2005 summary. Advance Data. 2007;2007:1–39.
Sandman D, Simantov E, An C, Fund C, Harris L. Out of touch: American men and the health care system. Commonwealth Fund New York, 2000.
Viera A, Thorpe J, Garrett J. Effects of sex, age, and visits on receipt of preventive healthcare services: a secondary analysis of national data. BMC Health Serv Res. 2006;6:15.
Neighbors HW, Howard CS. Sex differences in professional help seeking among adult Black Americans. Am J Community Psychol. 1987;15:403–17.
Green CA, Pope CR. Gender, psychosocial factors and the use of medical services: a longitudinal analysis. Soc Sci Med. 1999;48:1363–72.
United States. Agency for Healthcare R, Quality. National healthcare disparities report. In: Agency for Healthcare Research and Quality, 2006. Rockville: U.S. Dept. of Health and Human Service; 2006.
Arias E. United states life tables, 2004. Natl Vital Stat Rep. 2007;56:1–39.
Thom T, Haase N, Rosamond W, et al. Heart disease and stroke statistics–2006 Update: A report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2006;113:e85–151.
Wong MD, Chung AK, Boscardin JW, et al. The contribution of specific causes of death to sex differences in mortality. Public Health Rep. 2006;121:746–54.
Hertz RP, Unger AN, Cornell JA, Saunders E. Racial disparities in hypertension prevalence, awareness, and management. Arch Intern Med. 2005;165:2098–104.
Nelson K, Norris K, Mangione CM. Disparities in the diagnosis and pharmacologic treatment of high serum cholesterol by race and ethnicity: data from the Third National Health and Nutrition Examination Survey. Arch Intern Med. 2002;162:929–35.
Barnett E, Casper MC, Halveron TA, et al. Men and heart disease an atlas of racial and ethnic disparities in mortality. Morgantown: Office for Social Environment and Health Research, West Virginia University; 2000.
American Cancer Society. Colorectal Cancer Facts & Figures 2008-2010. In: Society AC, ed. Atlanta, 2008.
American Cancer Society. Cancer Facts & Figures for African Americans 2009-2010. In: Society AC, ed. Atlanta, 2009.
Agrawal S, Bhupinderjit A, Bhutani MS, et al. Colorectal cancer in African Americans. Am J Gastroenterol. 2005;100:515–23.
Ndubuisi SC, Kofie VY, Andoh JY, Schwartz EM. Black-White differences in the stage at presentation of prostate cancer in the District of Columbia. Urology. 1995;46:71–7.
Harper S, Lynch J, Burris S, Davey Smith G. Trends in the black-white life expectancy gap in the United States, 1983-2003. J Am Med Assoc. 2007;297:1224–32.
Kung HC, Hoyert DL, Xu J, Murphy SL. Deaths: final data for 2005. Natl Vital Stat Rep. 2008;56:1–120.
Ravenell JE, Whitaker EE, Johnson WE Jr. According to him: barriers to healthcare among African-American men. J Natl Med Assoc. 2008;100:1153–60.
Whitley EM, Samuels BA, Wright RA, Everhart RM. Identification of barriers to healthcare access for underserved men in Denver. J Mens Health Gend. 2005;2:421–8.
Cheatham CT, Barksdale DJ, Rodgers SG. Barriers to health care and health-seeking behaviors faced by Black men. J Am Acad Nurse Pract. 2008;20:555–62.
Hammond WP, Matthews D, Corbie-Smith G. Psychosocial factors associated with routine health examination scheduling and receipt among African-American men. J Natl Med Assoc. 2010;102:276–289.
Wade JC. Masculinity ideology, male reference group identity dependence, and African American men's health-related attitudes and behaviors. Psychol Men Masc. 2008;9:5–16.
Andersen RM. Revisiting the behavioral model and access to medical care: Does it matter? J Health Soc Behav. 1995;36:1–10.
Bradley EH, McGraw SA, Curry L, et al. Expanding the Andersen model: the role of psychosocial factors in long-term care use. Health Serv Res. 2002;37:1221–42.
Mahalik JR, Burns SM, Syzdek M. Masculinity and perceived normative health behaviors as predictors of men's health behaviors. Soc Sci Med. 2007;64:2201–9.
Courtenay WH. Constructions of masculinity and their influence on men's well-being: A theory of gender and health. Soc Sci Med. 2000;50:1385–401.
Månsdotter A, Lundin A, Falkstedt D, Hemmingsson T. The association between masculinity rank and mortality patterns: a prospective study based on the Swedish 1969 conscript cohort. J Epidemiol Community Health. 2009;63:408–13.
Marcell AV, Ford CA, Pleck JH, Sonenstein FL. Masculine beliefs, parental communication, and male adolescents' health care use. Pediatrics. 2007;119:e966–75.
Musa D, Schulz R, Harris R, Silverman M, Thomas SB. Trust in the health care system and the use of preventive health services by older Black and White adults. Am J Public Health. 2009;99:1293–9.
O'Malley AS, Sheppard VB, Schwartz M, Mandelblatt J. The role of trust in use of preventive services among low-income African-American women. Prev Med. 2004;38:777–85.
Addis ME, Mahalik JR. Men, masculinity, and the contexts of help seeking. Am Psychol. 2003;58:5–14.
Helgeson VS. Relation of agency and communion to well-being: Evidence and potential explanations. Psychol Bull. 1994;116:412–28.
Mahalik JR, Lagan HD, Morrison JA. Health behaviors and masculinity in Kenyan and U.S. male college students. Psychol Men Masc. 2006;7:191–202.
Helgeson VS. The role of masculinity in a prognostic predictor of heart attack severity. Sex Roles. 1990;22:755–74.
Helgeson V, Fritz H. Unmitigated agency and unmitigated communion: Distinctions from agency and communion. J Res Pers. 1999;33:131–58.
Bound J, Freeman RB. What Went Wrong? The erosion of relative earnings and employment among young Black men in the 1980s. Q J Econ. 1992;107:201–32.
Holzer HJ, Offner P. Trends in employment outcomes of young black men, 1979-2000. Madison: Institute for Research on Poverty, University of Wisconsin--Madison; 2002.
Hammond WP, Mattis JS. Being a man about It: Manhood meaning among African American men. Psychol Men Masc. 2005;6:114–26.
Wallace M. Black Macho and the Myth of the Superwoman. Verso, 1999.
Staples R. Black masculinity: The Black male's role in American society. Feminism and Masculinities. 2004:121.
Abreu J, Goodyear R, Campos A, Newcomb M. Ethnic belonging and traditional masculinity ideology among African Americans, European Americans, and Latinos. Psychology of Men and Masculinity. 2000;1:75–86.
Gordon E. Cultural politics of black masculinity. Transforming Anthropology. 1997;6:36–53.
Aronson RE, Whitehead TL, Baber WL. Challenges to masculine transformation among urban low-income African American males. Am J Public Health. 2003;93:732–41.
Wade JC, Brittan-Powell C. Men's attitudes toward race and gender equity: The importance of masculinity ideology, gender-related traits, and reference group identity dependence. Psychol Men Masc. 2001;2:42–50.
Sheldon S, Serpe RT. Identity salience and psychological centrality: equivalent, overlapping, or complementary concepts? Social Psychology Quarterly. 1994;57:16–35.
Hogg MA, Terry DJ, White KM. A tale of two theories: A critical comparison of identity theory with social identity theory. Soc Psychol Q. 1995;58:255–69.
LaVeist T, Nickerson K, Bowie J. Attitudes about racism, medical mistrust, and satisfaction with care among African American and white cardiac patients. Med Care Res Rev. 2000;57:146–61.
Gamble VN. Under the shadow of Tuskegee: African Americans and health care. Am J Public Health. 1997;87:1773–8.
Hammond WP. Psychosocial correlates of medical mistrust among African American men. Am J Community Psychol. 2010;45:86–107.
US Preventive Services Task Force. Guide to Clinical Preventive Services. Rockville: Agency for Healthcare Research and Quality; 2008.
Vasan RS, Kannel WB. Strategies for cardiovascular risk assessment and prevention over the life course: Progress amid imperfections. Circulation. 2009;120:360–3.
Lynch J, Smith GD. A life course approach to chronic disease epidemiology. Annu Rev Pub Health. 2005;26:1–35.
Fields LE, Burt VL, Cutler JA, Hughes J, Roccella EJ, Sorlie P. The burden of adult hypertension in the United States 1999 to 2000: A rising tide. Hypertension. 2004;44:398–404.
Hess PL, Reingold JS, Jones J, et al. Barbershops as hypertension detection, referral, and follow-up centers for Black men. Hypertension. 2007;49:1040–6.
Hart A, Bowen DJ. The feasibility of partnering with African-American barbershops to provide prostate cancer education. Ethn Dis. 2004;14:269–73.
Corbie-Smith G, Flagg E, Doyle J, O’Brien M. Influence of usual source of care on differences by race/ethnicity in receipt of preventive services. J Gen Intern Med. 2002;17:458–64.
Witt W, Kahn R, Fortuna L, et al. Psychological Distress as a Barrier to Preventive Healthcare Among U.S. Women. J Prim Prev. 2009;30:531–47.
Tessler R, Mechanic D, Dimond M. The effect of psychological distress on physician utilization: A prospective study. J Health Soc Behav. 1976;17:353–64.
Bellon JA, Delgado A, Luna JD, Lardelli P. Psychosocial and health belief variables associated with frequent attendance in primary care. Psychol Med. 1999;29:1347–57.
Manning WG Jr, Wells KB. The effects of psychological distress and psychological well-being on use of medical services. Med Care. 1992;30:541–53.
Shuval JT. Social functions of medical practice. San Francisco: Jossey-Bass; 1970.
Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401.
Levant RF, Hirsch LS, Celentano E, Cozza TM. The male role: An investigation of contemporary norms. Journal of Mental Health Counseling. 1992;14:325–37.
Sheldon S, Serpe RT. Identity salience and psychological centrality: equivalent, overlapping, or complementary concepts? Soc Psychol Q. 1994;57:16–35.
Hair JF. Multivariate Data Analysis. Upper Saddle River, N.J.; Harlow: Pearson Education, 2009.
Allison PD. Multiple imputation for missing data: A cautionary tale. Sociol Methods Res. 2000;28:301–9.
SPSS 17 for Windows. Chicago, Ill.: SPSS Inc., 2008.
Boulware LE, Marinopoulos S, Phillips KA, et al. Systematic Review: Systematic review: The value of the periodic health evaluation. Ann Intern Med. 2007;146:289–300.
Fiscella K, Franks P, Clancy CM. Skepticism toward medical care and health care utilization. Med Care. 1998;36:180–9.
Elster AB, Levenberg P. Integrating comprehensive adolescent preventive services into routine medicine care. Rationale and approaches. Pediatr Clin North Am. 1997;44:1365–77.
Marcell AV. The adolescent male. In: Heidelbaugh JJ, Jauniaux E, Landon MB, eds. Clinical men's health: evidence in practice. Philadelphia: Saunders/Elsevier; 2007:75–94.
Rich JA. Primary care for young African American men. J Am Coll Health. 2001;49:183.
Park MJ, Paul Mulye T, Adams SH, Brindis CD, Irwin JCE. The health status of young adults in the United States J Adolesc Health. 2006;39:305–17.
Stamler J, Daviglus ML, Garside DB, Dyer AR, Greenland P, Neaton JD. Relationship of baseline serum cholesterol levels in 3 large cohorts of younger men to long-term coronary, cardiovascular, and all-cause mortality and to longevity. J Am Med Assoc. 2000;284:311–8.
Wallston K, Wallston B. Who is responsible for your health? The construct of health locus of control. In: Sanders GS, Suls JM, eds. Social psychology of health and illness. Hillsdale: L. Erlbaum Associates; 1982:65–95.
United States Census Bureau. United States - Data Sets - American Fact Finder. 2009.
United States Bureau of Labor Statistics. The employment situation: December 2004-2007. Washington: U.S. Dept. of Labor, Bureau of Labor Statistics; 2008.
Reynolds WM. Development of reliable and valid short forms of the Marlowe-Crowne social desirability scale. J Clin Psychol. 1982;38:119–25.
Acknowledgments
Funding
This research was supported by a Student Award Program award to the first author from the Blue Cross and Blue Shield of Michigan Foundation (Grant # 657.SAP), The Robert Wood Johnson Foundation Health & Society Scholars Program, and The University of North Carolina Cancer Research Fund. Additional research and salary support during the preparation of this manuscript was provided to the first author from the National Center for Minority Health and Health Disparities (Award # 1L60MD002605-01), and National Cancer Institute (Grant # 3U01CA114629-04 S2).
Additional Contributions
The first author wishes to thank faculty, student, and community members of the UNC Men’s Health Research Lab: Yasmin Cole-Lewis, Travis Melvin, Justin Smith, Allison Mathews, Dr. Keon Gilbert, Melvin R. Muhammad, and Donald Parker for their assistance with data collection for the African-American Men’s Health & Social Life Study. The first author also thanks Dr. Amani Nuru-Jeter, Keith Hermanstyne, Adebiyi Adesina, and Michael Hammond for their assistance with data collection. The authors thank Dr. Nestor Lopez-Duran for his feedback about the statistical analyses.
Conflict of Interest
None disclosed.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hammond, W.P., Matthews, D., Mohottige, D. et al. Masculinity, Medical Mistrust, and Preventive Health Services Delays Among Community-Dwelling African-American Men. J GEN INTERN MED 25, 1300–1308 (2010). https://doi.org/10.1007/s11606-010-1481-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-010-1481-z