Abstract
Background
Obesity is successfully treated by bariatric operations, but some patients need reoperations. No large national studies are available to evaluate the safety and efficacy after reoperative bariatric surgery.
Methods
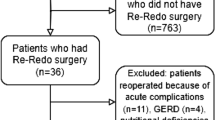
Data from June 2007 through March 2012 from the Bariatric Outcomes Longitudinal Database were queried for safety and efficacy of reoperations and compared to those who had initial bariatric operations but did not undergo reoperations. Reoperations were subdivided into corrective operations and conversions.
Results
Out of 449,753 bariatric operations, 28,720 (6.3 %) underwent reoperations of which 19,970 (69.5 %) were corrective and 8,750 (30.5 %) were conversions. The conversion group compared to primary operations was older (47.63 ± 10.8 vs. 45.5 ± 11.8 years), had less males (13.5 vs. 21.3 %), and had more African Americans (14.6 vs. 12 %). Comparing primary operations to corrective and conversions operations, respectively, the following were observed: length of stay (1.78 ± 4.95 vs. 2.04 ± 6.44 and 2.86 ± 4.58 days), severe adverse events at 30 days (1.6 vs. 1.7 and 3.3 %), severe adverse events at 1 year (2.15 vs. 1.9 and 3.61 %), percent excess weight loss at 1 year (43.2 vs. 35.9 ± 92.4 and 39.3 ± 39.9 %), 30-day mortality rate (0.1 vs. 0.12 and 0.21 %), and 1-year mortality rate (0.17 vs. 0.24 and 0.31 %). Comorbidities were resolved after both primary operations and reoperations.
Conclusions
Most bariatric surgery patients do not need reoperations. Among those who do, the complication rate is low and outcomes are clinically comparable to primary procedures.


Similar content being viewed by others
References
Buchwald H, Avidor Y, Braunwald E, Jensen MD, Pories W, Fahrbach K, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA: the Journal of the American Medical Association. 2004 Oct 13;292(14):1724-37.
Prachand VN, Davee RT, Alverdy JC. Duodenal switch provides superior weight loss in the super-obese (BMI > or =50 kg/m2) compared with gastric bypass. Ann Surg. 2006 Oct;244(4):611-9.
Courcoulas AP, Christian NJ, Belle SH, Berk PD, Flum DR, Garcia L, et al. Weight change and health outcomes at 3 years after bariatric surgery among individuals with severe obesity. JAMA: the journal of the American Medical Association. 2013 Dec 11;310(22):2416-25. PubMed PMID: 24189773.
Buchwald H, Estok R, Fahrbach K, Banel D, Sledge I. Trends in mortality in bariatric surgery: a systematic review and meta-analysis. Surgery. 2007 Oct;142(4):621-32; discussion 32-5.
Himpens J, Coromina L, Verbrugghe A, Cadiere GB. Outcomes of revisional procedures for insufficient weight loss or weight regain after Roux-en-Y gastric bypass. Obesity surgery. 2012 Nov;22(11):1746-54.
Greenbaum DF, Wasser SH, Riley T, Juengert T, Hubler J, Angel K. Duodenal switch with omentopexy and feeding jejunostomy—a safe and effective revisional operation for failed previous weight loss surgery. Surgery for obesity and related diseases: official Journal of the American Society for Bariatric Surgery. 2011 Mar-Apr;7(2):213-8.
Brethauer SA, Kothari S, Sudan R, Williams B, English WJ, Brengman M, et al. Systematic review on reoperative bariatric surgery: American Society for Metabolic and Bariatric Surgery Revision Task Force. Surg for Obes Relat Dis. 2014 Feb 22. doi: 10.1016/j.soard.2014.02.014.
DeMaria EJ, Pate V, Warthen M, Winegar DA. Baseline data from American Society for Metabolic and Bariatric Surgery-designated Bariatric Surgery Centers of Excellence using the Bariatric Outcomes Longitudinal Database. Surgery for obesity and related diseases: official Journal of the American Society for Bariatric Surgery. 2010 Jul-Aug;6(4):347-55.
Inabnet WB, 3rd, Belle SH, Bessler M, Courcoulas A, Dellinger P, Garcia L, et al. Comparison of 30-day outcomes after non-LapBand primary and revisional bariatric surgical procedures from the Longitudinal Assessment of Bariatric Surgery study. Surgery for obesity and related diseases: official Journal of the American Society for Bariatric Surgery. 2010 Jan-Feb;6(1):22-30.
Sudan R, Winegar D, Thomas S, Morton J. Influence of ethnicity on the efficacy and utilization of bariatric surgery in the USA. Journal of gastrointestinal surgery: official Journal of the Society for Surgery of the Alimentary Tract. 2014 Jan;18(1):130-6.
Mor A, Sharp L, Portenier D, Sudan R, Torquati A. Weight loss at first postoperative visit predicts long-term outcome of Roux-en-Y gastric bypass using Duke weight loss surgery chart. Surgery for obesity and related diseases: official Journal of the American Society for Bariatric Surgery. 2012 Sep-Oct;8(5):556-60.
Stroh C, Weiner R, Wolff S, Knoll C, Manger T, Obesity Surgery Working G, et al. Influences of Gender on Complication Rate and Outcome after Roux-en-Y Gastric Bypass: Data Analysis of More Than 10,000 Operations from the German Bariatric Surgery Registry. Obesity surgery. 2014 Apr 21.
Bekheit M, Katri K, Ashour MH, Sgromo B, Abou-Elnagah G, Abdel-Salam WN, et al. Gender influence on long-term weight loss after three bariatric procedures: gastric banding is less effective in males in a retrospective analysis. Surgical endoscopy. 2014 Mar 20.
Livingston EH, Huerta S, Arthur D, Lee S, De Shields S, Heber D. Male gender is a predictor of morbidity and age a predictor of mortality for patients undergoing gastric bypass surgery. Ann Surg. 2002 Nov;236(5):576-82.
Flum DR, Dellinger EP. Impact of gastric bypass operation on survival: a population-based analysis. Journal of the American College of Surgeons. 2004 Oct;199(4):543-51.
Schauer P, Ikramuddin S, Hamad G, Gourash W. The learning curve for laparoscopic Roux-en-Y gastric bypass is 100 cases. Surgical endoscopy. 2003 Feb;17(2):212-5.
Shikora SA, Kim JJ, Tarnoff ME, Raskin E, Shore R. Laparoscopic Roux-en-Y gastric bypass: results and learning curve of a high-volume academic program. Archives of surgery. 2005 Apr;140(4):362-7.
Sudan R, Bennett KM, Jacobs DO, Sudan DL. Multifactorial analysis of the learning curve for robot-assisted laparoscopic biliopancreatic diversion with duodenal switch. Ann Surg. 2012 May;255(5):940-5.
Ali MR, Tichansky DS, Kothari SN, McBride CL, Fernandez AZ, Jr., Sugerman HJ, et al. Validation that a 1-year fellowship in minimally invasive and bariatric surgery can eliminate the learning curve for laparoscopic gastric bypass. Surgical endoscopy. 2010 Jan;24(1):138-44.
Carlin AM, Zeni TM, English WJ, Hawasli AA, Genaw JA, Krause KR, et al. The comparative effectiveness of sleeve gastrectomy, gastric bypass, and adjustable gastric banding procedures for the treatment of morbid obesity. Ann Surg. 2013 May;257(5):791-7.
Acknowledgments
Funding was provided by an unrestricted grant to the American Society for Metabolic and Bariatric surgery. The funding agency had no input on data collection, analysis, results, or preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Discussant
Dr. Alfons Pomp (New York, NY):
I would like to thank the authors for the opportunity to discuss this interesting paper. This is another of an ever expanding group of papers presented at recent national meetings which have mined huge nonadministrative databases with multiple variables and tried to draw meaningful conclusions that are statistically valid. I, and others, remain somewhat dubious that most of these papers will actually allow us to make decisions of clinical significance.
The bariatric surgery databases of outcomes both from BOLD (and ACS) were historically established prior to the CMS decision to link accreditation with surgical outcome follow-up. This paper illustrates how it is actually possible for surgeons in multiple centers to enter data about their patients’ outcomes, use it in a comparative fashion, and then improve quality of care. Incidentally, it also shows just how safe and competent bariatric surgeons are as a group. We operate on these surgically difficult and seriously ill patients, mostly laparoscopically, with fairly amazing results.
My questions are as follows: (1) On what basis did you choose the serious adverse events from the 134 variables in the BOLD database? (2) Do you think the fact that 70 % of your revisions involved band to bypass or bypass to band skewed your results (showing relatively low rates of complications compared to other published series)? And finally (3) there were several statistical differences noted in the reoperation group, other than an increased length of stay (LOS), did you find anything clinically relevant?
Closing Discussant
Dr. Sudan:
Thank you for your comments and questions Dr. Pomp. I agree with you that establishing and participating in the data registry has been a big achievement for bariatric surgeons, and this clinically rich database provides very valuable information that has impacted quality of care. It is also true that bariatric surgeons have established that as a group we are able to perform complex primary bariatric operations very safely. However, the word that we can perform complex reoperative bariatric surgery still needs to get out. Each database has limitations, and therefore, investigators need to be knowledgeable about its nuances and conduct a responsible and careful analysis and we have attempted to do so. In response to your first question, BOLD collected information on 134 adverse events. To define severe adverse events, two experts in bariatric surgery reviewed this list and identified 33 acute adverse events that were potentially life-threatening such as bleeding requiring transfusion, leaks, deep venous thrombosis, sepsis, etc. We hoped that such severe events would be captured more completely in BOLD and, thus, yield valid results. This decision was based on judgment, and it is important to note that this list does not represent the full spectrum of complications that these patients may have suffered. In response to your second question, the vast majority of reoperations were related to an adjustable gastric band, and this may have driven the overall reoperation rate higher but kept the severity of complications low. We did not investigate procedure-specific severe adverse event rates but plan to do so in the future. Finally, when working with large databases, even small differences are statistically significant. Therefore, the results should be placed in a clinical context. In this study, even though length of stay, morbidity, and mortality were statistically higher, but from a clinical perspective, conversions had a length of stay of 3 days. At 1 year, mortality was around 0.3 % and severe adverse events were around 3.5 %. Comorbidities were also resolved. Therefore, the clinicians and patients have to decide if these risks are worth taking not withstanding statistical significance. We certainly believe so and hope that these results will encourage payors, health-care providers, and patients so that more people may benefit from bariatric reoperations.
Rights and permissions
About this article
Cite this article
Sudan, R., Nguyen, N.T., Hutter, M.M. et al. Morbidity, Mortality, and Weight Loss Outcomes After Reoperative Bariatric Surgery in the USA. J Gastrointest Surg 19, 171–179 (2015). https://doi.org/10.1007/s11605-014-2639-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-014-2639-5