Abstract
Methicillin-resistant Staphylococcus aureus (MRSA) is an important cause of pneumonia in ventilated patients. Our objective was to evaluate the GeneXpert MRSA/SA SSTI Assay (Xpert MRSA/SA) (Cepheid, Sunnyvale, CA) for use in lower respiratory tract (LRT) specimens for rapid MRSA detection and to determine the potentially saved antibiotic-days if a culture-based identification method was replaced by this assay. Remnant LRT samples from ventilated patients submitted to the microbiology laboratory for routine culture were tested using conventional culture and Xpert MRSA/SA. One hundred of 310 LRT specimens met the inclusion criteria. Ten samples were positive for MRSA by Xpert MRSA/SA, while six were positive by routine culture methods. Xpert MRSA/SA correctly identified 5/6 positive and 89/94 negative MRSA specimens, for a sensitivity of 83.3%, specificity of 94.7%, positive predictive value of 45.6%, and negative predictive value of 98.9%. The assay also correctly detected 3/3 positive and 90/97 negative methicillin-susceptible S. aureus (MSSA) specimens, for a sensitivity of 100%, specificity of 92.8%, positive predictive value of 30%, and negative predictive value of 100%. A total of 748 vancomycin and 305 linezolid antibiotic-days were associated with the enrolled specimens. Vancomycin and linezolid utilization could decrease by 68.4% and 83%, respectively, if discontinued 1 day after negative polymerase chain reaction (PCR) results. The Xpert MRSA/SA SSTI rapid MRSA PCR assay performed well in respiratory samples from ventilated patients with suspected pneumonia and has the potential to facilitate stewardship efforts such as reducing empiric vancomycin and linezolid therapy.
Similar content being viewed by others
Introduction
Methicillin-resistant Staphylococcus aureus (MRSA) is an important cause of ventilator-associated pneumonia (VAP) in the USA. For patients with suspected VAP, treatment guidelines suggest empirical therapy to cover MRSA in addition to other potential pathogens [1]. Using conventional microbiologic methods, however, 48 h or more may elapse before MRSA can be reliably excluded from a lower respiratory tract (LRT) specimen, with tracheal aspirate (TA), bronchial washing (BW), or bronchoalveolar lavage (BAL) being the most frequently obtained specimen types. Thus, clinicians are faced with a long interval of diagnostic uncertainty, obligating prolonged use of broad-spectrum empiric antibiotic therapy.
The Xpert MRSA/SA SSTI (Cepheid, Sunnyvale, CA) assay is a polymerase chain reaction (PCR)-based assay which is FDA cleared for the detection of MRSA and methicillin-susceptible S. aureus (MSSA) in specimens collected from skin and soft tissue infections. The assay provides a result in approximately 1 h. To detect S. aureus, the assay relies on the detection of spa, the gene for staphylococcal protein A. To infer resistance to methicillin and identify the organism as MRSA, it must also detect the methicillin resistance gene (mecA) and the junction between the staphylococcal cassette chromosome that harbors mecA (SCCmec) and the S. aureus chromosome. The assay has been adapted for off-label use to detect MRSA in suspected VAP [2, 3] and osteoarticular infections [4].
Preliminary data in our institution demonstrate that approximately 20% of patients with cultures from LRT secretions obtained from medical and surgical intensive care units (ICUs) were positive for S. aureus, with 9% determined to be methicillin-resistant. The Xpert MRSA/SA SSTI assay could be beneficial to reduce the interval of diagnostic uncertainty by identifying or ruling out MRSA in patients with suspected VAP and guiding antimicrobial therapy in a more timely fashion compared to conventional culture. The objectives of this study were two-fold: (1) to evaluate the analytical performance characteristics of the MRSA/SA SSTI assay for the rapid detection of MRSA in LRT specimens and (2) to evaluate its potential role in antimicrobial stewardship efforts for managing suspected VAP, specifically concerning anti-MRSA agents.
Materials and methods
Setting
Frozen and fresh LRT specimens collected at Barnes-Jewish Hospital, a 1250-bed, tertiary care academic medical center, between 2012 and 2014 were included. The study was approved by the Washington University School of Medicine Institutional Review Board. All specimens included in the study were de-identified by an individual not otherwise associated with the study (i.e., the Honest Broker).
Standard-of-care LRT culture
BAL, BW, and TA cultures were plated to 5% sheep’s blood, chocolate, and MacConkey agar (Remel, Lenexa, KS), using a 1-μL calibrated loop, and incubated at 35 °C in an environment with 5% CO2. Thresholds for work-up of BAL, BW, and TA specimens were ≥103 colony-forming units (CFU)/mL, ≥5 × 103 CFU/mL, and ≥105 CFU/mL, respectively. Cultures were discarded if no growth was observed following 48 h of incubation. In S. aureus, methicillin resistance was confirmed using Kirby–Bauer disk diffusion in accordance with Clinical and Laboratory Standards Institute (CLSI) guidelines [5, 6]. This standard-of-care LRT culture was used as the gold standard for comparison when calculating the analytical performance characteristics of the Xpert MRSA/SA.
Limit of detection and reproducibility studies
Limit of detection (LOD) studies were performed using cultured isolates of Staphylococcus epidermidis (clinical isolate), S. aureus ATCC 29213 (MSSA), MRSA SCCmec type II, and MRSA SCCmec type IV (clinical isolates). Isolates were resuspended in 0.9% saline to a 0.5 McFarland standard and subsequently diluted to final concentrations of 105, 104, 103, and 102 CFU/mL. In addition, a negative saline control was analyzed. Subsequently, LOD studies were repeated in the matrix of pooled, S. aureus-negative, BAL fluid. Replicate testing, using 104 CFU/mL of the same group of organisms in BAL fluid, was performed over three consecutive days.
Retrospective samples
Study procedures were approved by the Washington University School of Medicine Institutional Review Board. Thirty frozen banked LRT specimens (including 13 TAs and 17 BALs), obtained during routine diagnostic work-up prior to this study, were tested using the Xpert MRSA/SA SSTI assay, and the results were compared to the standard-of-care LRT culture result performed in the clinical microbiology laboratory. A flocked swab (Copan, Murrieta, CA) was placed into the specimen and subsequently inserted into the Xpert elution buffer vial. Next, the swab was broken, and the vial was closed and vortexed for 10 s. A sterile pipette was used to transfer the contents of the elution vial to the “S” chamber of the Xpert MRSA/SA cartridge, and the cartridge was loaded onto the GeneXpert Dx instrument. Testing was otherwise performed and results interpreted according to the manufacturer’s protocol.
Prospective samples
Specimens submitted to the microbiology laboratory for routine bacterial culture during the study period (November 2013 to March 2014) were screened by the Honest Broker for study eligibility in the prospective part of the study. The following six items were the inclusion criteria: (1) subject ≥18 years of age; (2) patient admitted to the ICU; (3) patient on a ventilator at the time of sample collection; (4) ≥1 mL of remnant TA, BAL, or BW specimen available; (5) specimen tested by GeneXpert within 6 h of collection; and 6) presence of at least one of the following clinical criteria: (a) active or recently discontinued use of broad-spectrum antibiotics (vancomycin, linezolid, cefepime, or meropenem); (b) temperature >38.3 °C (within previous 72 h); (c) white blood cell or leukocyte count ≥10,000/μL or ≤4000/μL (within 72 h of specimen collection); (d) purulent specimen (>25 polymorphonuclear cells/high-power field); or (e) recent intubation (within 72 h of specimen collection). Patients with a previous positive result from the Xpert MRSA/SA assay were excluded.
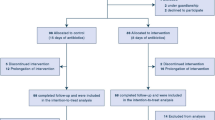
Specimens were screened for eligibility three times per day on weekdays by the Honest Broker. Three hundred and ten LRT specimens were screened and 100 specimens met the study inclusion criteria and were tested using the Xpert MRSA/SA.
In addition to the standard-of-care culture, if a specimen was positive for MSSA or MRSA by the Xpert MRSA/SA, 100-μL and 500-μL aliquots were inoculated to blood agar (BD Diagnostics, Franklin Lakes, NJ), in addition to the standard-of-care culture, to attempt to isolate the organism. Isolates recovered using the larger aliquots were not included in the sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) calculations.
Molecular typing
SCCmec characterization was performed on S. aureus isolates using a previously described multiplex PCR assay that detects and differentiates SCCmec types I–V [7]. Strain typing of S. aureus isolates was performed by repetitive sequence-based PCR (rep-PCR), using the DiversiLab Bacterial Barcodes system (bioMérieux, Durham, NC), as previously described [8]. Isolates with a similarity index of ≥95% were considered to represent the same strain.
Detection of high-level mupirocin resistance and chlorhexidine resistance
Phenotypic high-level mupirocin resistance was detected using a 200-μg mupirocin disk (Oxoid, Hampshire, United Kingdom), in accordance with CLSI guidelines [5]. In addition to phenotypic mupirocin resistance testing, a multiplex PCR for the detection of mupA (mupirocin resistance) and qacA/B (chlorhexidine tolerance) was performed as previously described [8, 9].
Antimicrobial stewardship applicability
Clinical data on subjects whose specimens met the eligibility criteria were obtained from Washington University’s medical informatics clinical data repository, including microbiological culture results (for the LRT specimen tested in the study, in addition to any other positive culture results) as well as antimicrobials utilized. “Total antibiotic-days” (all consecutive days that antibiotics were administered starting 48 h prior to the study specimen collection date, until discontinued) were calculated for vancomycin and linezolid. Other antibiotics with activity against MRSA were not included. The number of antibiotic-days that could have potentially been avoided was calculated using the “earliest date when antibiotics could be discontinued”. This was calculated as the calendar day after a negative MRSA PCR, given that no other clinical cultures were positive for MRSA. The potential reduction of antibiotic use (i.e., the number of antibiotic-days saved) was calculated by subtracting this number from the total antibiotic-days.
Results
Limit of detection studies
The LOD in saline was 103 CFU/mL for MSSA and MRSA SCCmec type IV. For MRSA SCCmec type II, the LOD was 104 CFU/mL. In BAL fluid, the LOD was 103 CFU/mL for MSSA and MRSA SCCmec type II, while it was 104 CFU/mL for MRSA SCCmec type IV.
Retrospective validation samples
The Xpert MRSA/SA SSTI assay correctly detected MRSA in 9 of 9 specimens positive by routine culture and did not detect MRSA in 21 of 21 specimens negative by routine culture, resulting in a sensitivity of 100% [95% confidence interval (CI): 62.9–100%], specificity of 100% (95% CI: 80.8–100%), PPV of 100% (95% CI: 62.9–100%), and NPV of 100% (95% CI: 80.8–100%). In addition, MSSA was correctly detected in 4 of 6 specimens positive by routine culture and was not detected in 24 of 24 specimens negative by routine culture, resulting in a sensitivity of 66.7% (95% CI: 24.1–94.0%), specificity of 100% (95% CI: 82.8–100%), PPV of 100% (95% CI: 39.6–100%), and NPV of 92.3% (95% CI: 73.4–98.7%). Four isolates of MSSA and seven isolates of MRSA were recovered from the subset of frozen specimens saved for molecular analysis.
Prospective samples
Of the 100 prospective specimens, which included BALs, TAs, and BWs, Xpert MRSA/SA detected MRSA in 5 of 6 specimens positive by standard-of-care culture, resulting in a sensitivity of 83.3% (95% CI: 36.5–99.1%). The false-negative was a BAL specimen. Xpert MRSA/SA detected MRSA in an additional five specimens, four BALs and one BW, where MRSA was not recovered by routine culture, resulting in a specificity of 94.7% (95% CI: 87.5–98.0%), PPV of 50% (95% CI: 20.1–79.9%), and NPV of 98.9% (95% CI: 93.1–99.9%) (Table 1). Of note, in higher volume cultures (500 μL, inoculated to 5% sheep’s blood agar), MRSA was recovered in 3 of the 5 specimens that were negative by routine culture but positive by PCR. The mean cycle threshold (Ct) values were as follows: spa 26.41 (range 16.5–35.5), mecA 26.58 (range 17.6–32.5), and scc 27.94 (range 19.2–34.6) (Table 2).
The Xpert MRSA/SA assay detected MSSA in 3 of 3 specimens positive by routine culture, resulting in a sensitivity of 100% (95% CI: 31.0–100%). In addition, MSSA was detected in an additional seven specimens, five BALs and two TAs, which were negative by routine culture, for a specificity of 92.8% (95% CI: 85.2–96.8%). The PPV and NPV for MRSA were 30.0% (95% CI: 8.1–64.6%) and 100% (95% CI: 94.9–100%), respectively. In higher volume cultures (500 μL, inoculated to 5% sheep’s blood agar), MSSA was recovered in two additional specimens. The average spa Ct was 29.32 (range 16.5–35.5) (Table 2). The spa Ct for the two specimens in which MSSA was only recovered when plating 500 μL were 26.2 and 29.9.
Of the 100 prospective specimens, 36 were visibly bloody and 13 specimens contained visible mucus; these specimens produced an Xpert MRSA/SA result on the first attempt with the exception of one viscous specimen, which resulted in a pressure error. The assay was repeated on the same specimen, and a valid result was obtained. Of the 51 non-bloody, non-viscous specimens, three specimens did not give a result on the first attempt. Two of the specimens gave an error message on the first run, while a third specimen gave an invalid result. The invalid specimen and one of specimens with an error message yielded a valid result upon repeating the assay. One specimen, which gave an error message on the first attempt, gave an invalid result on the second attempt. The specimen had to be diluted 1:10 with sterile saline before a valid result was obtained. Overall, the assay had to be repeated 4% of the time.
Characterization of isolates
A total of 15 MRSA and nine MSSA isolates recovered from retrospective and prospective specimens were further characterized by SCCmec typing, high-level mupirocin resistance, chlorhexidine resistance, and molecular typing. Of the 15 MRSA isolates recovered, 12 isolates were SCCmec type II and three isolates were SCCmec type IV. All nine MSSA isolates were negative by SCCmec typing. Analysis of the 24 isolates by rep-PCR demonstrated heterogeneity of the strains recovered. In total, eight unique strain types were identified. The largest cluster contained 14 isolates, with the next two clusters containing four and two isolates, respectively. The second and third clusters were unrelated to the first cluster and to each other. Four unique isolates, unrelated to any other isolates in the study, were also identified.
Two isolates, both prospective MRSA isolates, were mupirocin resistant, by both phenotypic and genotypic (mupA) methods. None of the isolates tested contained the chlorhexidine tolerance gene, qacA/B.
Retrospective evaluation of the potential impact of Xpert MRSA/SA on antimicrobial stewardship
For 27 subjects in the study, MRSA was recovered in culture from a clinical specimen that was not evaluated as part of the study: TA (24 from 15 subjects), BAL (8 from 7 subjects), blood (8 from 5 subjects), BW (6 from 6 subjects), sputum (1), joint fluid (1), abscess (1), and wound (1), with a subset of patients (n = 6) having more than one positive culture. Nares screening swabs for MRSA active surveillance were positive for nine subjects.
Of the 100 subjects associated with the prospective specimen set, 96 received vancomycin and/or linezolid. The four subjects who did not receive these agents were negative for MRSA based on both Xpert MRSA/SA and culture.
Vancomycin was administered to 88 patients for a total of 748 total antibiotic-days and a mean duration of 8.5 days. Linezolid was administered to 28 patients for a total of 305 total antibiotic-days and a mean duration of 10.9 days. If the anti-MRSA agent had been discontinued one calendar day after a negative MRSA PCR result in patients without any additional culture or PCR results positive for MRSA (including surveillance swabs), the total antibiotic-days and mean duration would have decreased. The vancomycin total antibiotic-days would have decreased by 68.4% (512 days) to a mean duration of 2.7 days, and linezolid would have decreased by 83% (253 days) to a mean duration of 1.9 days.
Cost analysis
An approximate cost estimate for a single Xpert MRSA/SA assay is $60; thus, for 100 patients, the test costs would have been $6000. This is an underestimate of the true cost, as it does not account for quality control testing, repeat testing, equipment acquisition, or labor. Based on the John’s Hopkins Antibiotic Guide, average wholesale prices for the evaluated antimicrobials are estimated to be approximately $15.56 per day (based on a dose of 1 g b.i.d.) for vancomycin and $240.22 per day (based on a dose of 600 mg b.i.d.) for linezolid [10]. This is also an underestimate as it does not take into account drug administration costs or expenses for therapeutic drug monitoring and other laboratory testing, such as laboratory testing to monitor renal function in patients receiving vancomycin therapy. It also does not take into account the costs associated with complications due to these antibiotics, particularly vancomycin and renal injury. If vancomycin usage was reduced by 512 days, it would result in savings of $7966.72 in drug cost, and if linezolid usage was decreased by 253 days, it would result in savings of $60,775.66 in drug cost. Based on these estimates, the total potential antibiotic savings were $62,742.38. Thus, an estimate of potential cost savings would be $627.42 per patient.
Discussion
Antimicrobial resistance is an increasing threat in the USA and worldwide. The Centers for Disease Control and Prevention (CDC) has recently listed MRSA as one of the current antibiotic threats in the USA and has assigned it a threat level of “Serious” [11]. One core approach to address antimicrobial resistance is to reduce unnecessary antibiotic use, and in order to do so, it is imperative to reduce the window of diagnostic uncertainty, thus shortening the duration of empiric antibiotics.
The Infectious Diseases Society of America (IDSA) recently published a public policy document declaring that, in order for tests to have a positive impact on patient care, new tests need to provide information about the causative organism, including antimicrobial susceptibility/resistance information, if possible, and must have rapid results, ideally within 1 h [12, 13]. Even with the development of rapid assays, however, the positive impact on patient care can only be achieved if physicians act quickly upon the results and start adequate or stop inadequate antibiotics. Such tests have been scrutinized for the detection of bloodborne pathogens, in a number of studies, often with a positive impact in antimicrobial stewardship efforts [14–16]. There are currently no commercial pathogen-specific assays available for evaluating respiratory specimens for hospital-acquired pneumonia (HAP) or VAP, although the MRSA/SA SSTI assay has been evaluated off-label in this and two prior studies.
One specimen that was positive for MRSA by routine culture was negative by the MRSA/SA SSTI assay. A limitation of the Xpert assay compared to culture is that the assay may not detect emerging SCCmec variants, and it is possible that the isolate may have been an SCCmec variant [17]. Laboratories considering implementing the assay should consider local epidemiology before relying on PCR to exclude the presence of S. aureus in respiratory tract specimens.
Seven specimens (two MRSA, five MSSA) were positive by the MRSA/SA SSTI assay but negative by culture. All seven specimens had spa PCR Cts greater than 30 when tested by the MRSA/SA SSTI assay, suggesting that the organism burden in these specimens was low. Alternatively, the PCR assay may have been detecting remnant DNA from dead organisms. Three additional MRSA PCR-positive specimens also had spa Cts greater than 30, but those three were recovered in culture. However, in those three cases, MRSA was not recovered in routine culture and was only recovered when a larger volume (500 μL) was evaluated. The organism burden in these specimens may, thus, represent colonization rather than infection, or it may represent non-viable organisms after exposure to antimicrobials, such as linezolid or vancomycin. Laboratories considering such testing may wish to modify the Ct cutoff value for reporting positive PCR results from respiratory specimens.
Two previous studies have examined the performance of the MRSA/SA SSTI assay on LRT specimens. In a validation study, the sensitivity, specificity, PPV and NPV were 99%, 72.2%, 90.7%, and 96.3%, respectively, when compared with quantitative cultures for detecting MRSA in LRT samples [3]. Leone et al. [2] utilized the assay to evaluate the presence of MSSA or MRSA in LRT samples of patients with suspected VAP, and reported NPVs of 99.7% and 99.8%, respectively. In contrast to the evaluation described herein (where MRSA prevalence was 8%), a limitation of Leone et al.’s study is that the reported MRSA prevalence was <2%. Neither study estimated the impact of the assay on antimicrobial stewardship efforts or antimicrobial cost avoidance. Other studies have evaluated automated microscopy of mini-BAL specimens [18], nares MRSA screening [19], and the Gram stain of a respiratory specimen [20] for the likelihood and diagnosis of VAP.
The strengths of this study include that it was conducted in a high-prevalence, high-acuity setting, and that it included a calculation of total antibiotic-days, potential antibiotic-days saved, and an estimated cost savings analysis. In addition, the strain typing and characterization data demonstrate that multiple S. aureus strain types were recovered from the patients in this study. The variety of strain types detected verifies that off-label use of the assay is capable of detecting multiple S. aureus strain types, and it also proves that the study, although conducted at a single center, did not simply repeatedly test the same clone.
The limitations of this study include the fact that the assay results were not reported for use into routine clinical care, and all the clinical data were obtained retrospectively from the medical records. Thus, the cost analysis presented is an estimate based on the assumption that the assay results would have impacted antimicrobial therapy. In addition, the cost analysis does not take into consideration patients without clinical improvement after 48–72 h, where discontinuation of vancomycin or linezolid would be unlikely to occur. However, these data suggest that incorporation of this test into the management of ICU patients suspected to have VAP has the potential to provide cost savings to hospitals.
There are currently no commercially available assays for the rapid detection of MRSA/MSSA in LRT specimens, and, thus, off-label use of the Xpert MRSA/SA SSTI assay is a promising alternative for the microbiological diagnosis of VAP. Herein, we demonstrate the sensitivity and specificity of this approach, and suggest that rapid detection of MRSA in LRT specimens using this assay could be a tool to support antimicrobial stewardship efforts in patients with suspected VAP. Prospective studies incorporating this approach into routine clinical use are needed to confirm these findings.
References
American Thoracic Society; Infectious Diseases Society of America (2005) Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med 171(4):388–416. doi:10.1164/rccm.200405-644ST
Leone M, Malavieille F, Papazian L, Meyssignac B, Cassir N, Textoris J, Antonini F, La Scola B, Martin C, Allaouchiche B, Hraiech S; AzuRea Network (2013) Routine use of Staphylococcus aureus rapid diagnostic test in patients with suspected ventilator-associated pneumonia. Crit Care 17(4):R170. doi:10.1186/cc12849
Cercenado E, Marín M, Burillo A, Martín-Rabadán P, Rivera M, Bouza E (2012) Rapid detection of Staphylococcus aureus in lower respiratory tract secretions from patients with suspected ventilator-associated pneumonia: evaluation of the Cepheid Xpert MRSA/SA SSTI assay. J Clin Microbiol 50(12):4095–4097. doi:10.1128/jcm.02409-12
Dubouix-Bourandy A, de Ladoucette A, Pietri V, Mehdi N, Benzaquen D, Guinand R, Gandois JM (2011) Direct detection of Staphylococcus osteoarticular infections by use of Xpert MRSA/SA SSTI real-time PCR. J Clin Microbiol 49(12):4225–4230. doi:10.1128/jcm.00334-11
Clinical and Laboratory Standards Institute (CLSI) (2014) Performance standards for antimicrobial susceptibility testing; Twenty-fourth informational supplement. CLSI document M100-S24. , Wayne
Clinical and Laboratory Standards Institute (CLSI) (2012) Performance standards for antimicrobial disk susceptibility tests; Approved standard—Eleventh edition. CLSI document M02-A11. CLSI, Wayne
Boye K, Bartels MD, Andersen IS, Møller JA, Westh H (2007) A new multiplex PCR for easy screening of methicillin-resistant Staphylococcus aureus SCCmec types I–V. Clin Microbiol Infect 13(7):725–727. doi:10.1111/j.1469-0691.2007.01720.x
Fritz SA, Hogan PG, Camins BC, Ainsworth AJ, Patrick C, Martin MS, Krauss MJ, Rodriguez M, Burnham CA (2013) Mupirocin and chlorhexidine resistance in Staphylococcus aureus in patients with community-onset skin and soft tissue infections. Antimicrob Agents Chemother 57(1):559–568. doi:10.1128/aac.01633-12
Hogue JS, Buttke P, Braun LE, Fairchok MP (2010) Mupirocin resistance related to increasing mupirocin use in clinical isolates of methicillin-resistant Staphylococcus aureus in a pediatric population. J Clin Microbiol 48(7):2599–2600. doi:10.1128/jcm.02118-09
Bartlett JG (ed) (2016) The Johns Hopkins POC-IT ABX Guide. Available online at: http://www.hopkinsguides.com/hopkins/view/Johns_Hopkins_ABX_Guide/540602/all/**About**. Accessed 20 Mar 2016
Centers for Disease Control and Prevention (CDC) (2013) Antibiotic resistance threats in the United States, 2013. Available online at: http://www.cdc.gov/drugresistance/pdf/ar-threats-2013-508.pdf. Accessed 20 Mar 2016
Caliendo AM, Gilbert DN, Ginocchio CC, Hanson KE, May L, Quinn TC, Tenover FC, Alland D, Blaschke AJ, Bonomo RA, Carroll KC, Ferraro MJ, Hirschhorn LR, Joseph WP, Karchmer T, MacIntyre AT, Reller LB, Jackson AF; Infectious Diseases Society of America (IDSA) (2013) Better tests, better care: improved diagnostics for infectious diseases. Clin Infect Dis 57(Suppl 3):S139–S170. doi:10.1093/cid/cit578
Bauer KA, Perez KK, Forrest GN, Goff DA (2014) Review of rapid diagnostic tests used by antimicrobial stewardship programs. Clin Infect Dis 59(Suppl 3):S134–S145. doi:10.1093/cid/ciu547
Banerjee R, Teng CB, Cunningham SA, Ihde SM, Steckelberg JM, Moriarty JP, Shah ND, Mandrekar JN, Patel R (2015) Randomized trial of rapid multiplex polymerase chain reaction-based blood culture identification and susceptibility testing. Clin Infect Dis 61(7):1071–1080. doi:10.1093/cid/civ447
Parta M, Goebel M, Matloobi M, Stager C, Musher DM (2009) Identification of methicillin-resistant or methicillin-susceptible Staphylococcus aureus in blood cultures and wound swabs by GeneXpert. J Clin Microbiol 47(5):1609–1610. doi:10.1128/JCM.00351-09
Spencer DH, Sellenriek P, Burnham CA (2011) Validation and implementation of the GeneXpert MRSA/SA blood culture assay in a pediatric setting. Am J Clin Pathol 136(5):690–694. doi:10.1309/AJCP07UGYOKBVVNC
Laurent C, Bogaerts P, Schoevaerdts D, Denis O, Deplano A, Swine C, Struelens MJ, Glupczynski Y (2010) Evaluation of the Xpert MRSA assay for rapid detection of methicillin-resistant Staphylococcus aureus from nares swabs of geriatric hospitalized patients and failure to detect a specific SCCmec type IV variant. Eur J Clin Microbiol Infect Dis 29(8):995–1002. doi:10.1007/s10096-010-0958-3
Douglas IS, Price CS, Overdier KH, Wolken RF, Metzger SW, Hance KR, Howson DC (2015) Rapid automated microscopy for microbiological surveillance of ventilator-associated pneumonia. Am J Respir Crit Care Med 191(5):566–573. doi:10.1164/rccm.201408-1468OC
Langsjoen J, Brady C, Obenauf E, Kellie S (2014) Nasal screening is useful in excluding methicillin-resistant Staphylococcus aureus in ventilator-associated pneumonia. Am J Infect Control 42(9):1014–1015. doi:10.1016/j.ajic.2014.05.026
O’Horo JC, Thompson D, Safdar N (2012) Is the gram stain useful in the microbiologic diagnosis of VAP? A meta-analysis. Clin Infect Dis 55(4):551–561. doi:10.1093/cid/cis512
Acknowledgments
The authors thank Meghan Wallace for her assistance as the Honest Broker.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was funded by a Barnes-Jewish Hospital Patient Safety and Quality Fellowship (to J.M.) and a BIRCWH grant (5K12HD001459-13; J.M.). The funders had no role in the study design, data collection and interpretation, or the decision to submit the work for publication.
Conflict of interest
C.-A.D.B. has received research support from Cepheid. J.M. has served on an advisory board for Astellas Switzerland.
Ethical approval
The study was approved by the Washington University Institutional Review Board.
Informed consent
Informed consent was not required for this study.
Additional information
S. E. Trevino and M. A. Pence contributed equally to this work.
Rights and permissions
About this article
Cite this article
Trevino, S.E., Pence, M.A., Marschall, J. et al. Rapid MRSA PCR on respiratory specimens from ventilated patients with suspected pneumonia: a tool to facilitate antimicrobial stewardship. Eur J Clin Microbiol Infect Dis 36, 879–885 (2017). https://doi.org/10.1007/s10096-016-2876-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-016-2876-5