Abstract
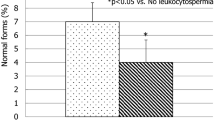
This study aims to perform global gonadal and sexual function assessments in systemic lupus erythematosus-related antiphospholipid syndrome (SLE-APS) patients. A cross-sectional study was conducted in ten SLE-APS male patients and 20 healthy controls. They were assessed by demographic data, clinical features, urological examination, sexual function, testicular ultrasound, seminal parameters, sperm antibodies, and hormone profile. The median of current age was similar in SLE-APS patients and controls with a higher frequency of erectile dysfunction in the former group (30 vs. 0 %, p = 0.029). The median penis circumference was significantly reduced in SLE-APS patients with erectile dysfunction compared to patients without this complication (8.17 vs. 9.14 cm, p = 0.0397). SLE-APS patients with previous arterial thrombosis had a significantly reduced median penis circumference compared to those without this complication (7.5 vs. 9.18 cm, p = 0.039). Comparing SLE-APS patients and controls, the former had a significant lower median of sperm concentration (41.1 vs. 120.06 × 106/mL, p = 0.003), percentages of sperm motility (47.25 vs. 65.42 %, p = 0.047), normal sperm forms by WHO guidelines (11 vs. 23.95 %, p = 0.002), and Kruger criteria (2.65 vs. 7.65 %, p = 0.02). Regarding seminal analysis, the medians of sperm concentration and total sperm count were significantly lower in SLE-APS patients treated with intravenous cyclophosphamide vs. those untreated with this drug (p < 0.05). Therefore, we have observed a novel association of reduced penile size with erectile dysfunction and previous arterial thrombosis in SLE-APS patients. Penis assessment should be routinely done in SLE-APS patients with fertility problems. We also identified that intravenous cyclophosphamide underlies severe sperm alterations in these patients.
Similar content being viewed by others
References
Rabelo-Júnior CN, Carvalho JF, Gallinaro AL, Bonfa E, Cocuzza M, Saito O et al (2012) Primary antiphospholipid syndrome: morphofunctional penile abnormalities with normal sperm analysis. Lupus 21(3):251–256
Wilson WA, Gharavi AE, Koike T, Lockshin MD, Branch DW, Piette JC et al (1999) International consensus statement on preliminary classification criteria for definite antiphospholipid syndrome: report of an international workshop. Arthritis Rheum 42:1309–1311
Hochberg MC (1997) Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 40:1725
Abdo CH (2007) The male sexual quotient: a brief, self-administered questionnaire to assess male sexual satisfaction. J Sex Med 4:382–389
World Health Organization (WHO) (1999) Laboratory manual for the examination of human semen and sperm-cervical mucus interaction, 4th edn. Cambridge University Press, New York, pp 1–128
Kruger TF, Acosta AA, Simmons KF, Swanson RJ, Matta JF, Oehninger S (1988) Predictive value of abnormal sperm morphology in vitro fertilization. Fertil Steril 49:112–117
Bombardier C, Gladman DD, Urowitz MB, Karon D, Chang CH, and The Committee on Prognosis Studies in SLE (1992) Derivation of the SLEDAI: a disease activity index for lupus patients. Arthritis Rheum 35:630–640
Gladman D, Ginzler E, Goldsmith C, Fortin P, Liang M, Urowitz M et al (1996) The development and initial validation of the Systemic Lupus International Collaborating Clinics/American College of Rheumatology Damage Index for systemic lupus erythematosus. Arthritis Rheum 39:363–369
Haris EN, Pierangeli S, Birch D (1994) Cardiolipin Wet Workshop report. Am J Clin Path 101:616–624
Wisloff F, Jacobsen EM, Liestol S (2002) Laboratory diagnosis of the antiphospholipid syndrome. Thromb Res 108:263–271
Silva CA, Bonfa E, Ostensen M (2010) Maintenance of fertility in patients with rheumatic diseases needing anti-inflammatory and immunosuppressive drugs. Arthritis Care Res (Hoboken) 62:1682–1690
Nukumizu LA, Saad GC, Ostensen M, Almeida BP, Cocuzza M, Gonçalves C, et al. (2012) Gonadal function in male patients with ankylosing spondylitis. Scand J Rheumatol (in press)
Vecchi A, Borba E, Bonfá E, Cocuzza M, Pieri P, Kim CA et al (2011) Penile anthropometry in systemic lupus erythematosus patients. Lupus 20:512–518
El-Sakka AI, Yassin AA (2010) Amelioration of penile fibrosis: myth or reality. J Androl 31:324–335
Soares PM, Borba EF, Bonfa E, Hallak J, Al C, Silva CA (2007) Gonad evaluation in male systemic lupus erythematosus. Arthritis Rheum 56:2352–2361
Suehiro RM, Borba EF, Bonfa E, Okay TS, Cocuzza M, Soares PM et al (2008) Testicular Sertoli cell function in male systemic lupus erythematosus. Rheumatology (Oxford) 47:1692–1697
Moraes AJ, Pereira RM, Cocuzza M, Casemiro R, Saito O, Silva CA (2008) Minor sperm abnormalities in young male post-pubertal patients with juvenile dermatomyositis. Braz J Med Biol Res 41:1142–1147
Moraes AJ, Pereira RM, Cocuzza M, Casemiro R, Saito O, Silva CA (2010) Gonad evaluation in male dermatomyositis. A pilot study. Clin Exp Rheumatol 28:441–442
Silva CA, Leal MM, Leone C, Simone VP, Takiuti AD, Saito MI et al (2002) Gonadal function in adolescents and young female with systemic lupus erythematosus. Lupus 11:419–425
Febronio MV, Pereira RM, Bonfa E, Takiuti AD, Pereyra EA, Silva CA (2007) Inflammatory cervicovaginal cytology is associated with disease activity in juvenile systemic lupus erythematosus. Lupus 16:430–543
Silva CA, Deen ME, Febronio MV, Oliveira SK, Terreri MT, Sacchetti SB et al (2011) Hormone profile in juvenile systemic lupus erythematosus with previous or current amenorrhea. Rheumatol Int 31:1037–1043
Aikawa NE, Sallum AM, Pereira RM, Suzuki S, Viana VS, Bonfá EETAL (2012) Subclinical impairment of ovarian reserve in juvenile systemic lupus erythematosus after cyclophosphamide therapy. Clin Exp Rheumatol 30(3):445–449
Aikawa NE, Sallum AM, Leal MM, Bonfá E, Pereira RM, Silva CA (2010) Menstrual and hormonal alterations in juvenile dermatomyositis. Clin Exp Rheumatol 28:571–575
Acknowledgments
This study was supported by the Fundação de Amparo à Pesquisa do Estado de São Paulo (grants 2004/07832-2 and 2005/56482-7 to CAS) and the Conselho Nacional de Desenvolvimento Científico e Tecnológico–CNPQ (grants 301411/2009-3 to EB, 3300665/2009-1 to JFC, and 302724/2011-7 to CAS), the Federico Foundation Grants (grants to JFC, EB, and CAS), and by the Núcleo de Apoio à Pesquisa Saúde da Criança e do Adolescente da USP. Our gratitude to Maribê Salan Marcos and Rosa Casemiro for technical support and Francisco Erivelton Aragão for the statistical analysis.
Disclosures
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rabelo-Júnior, C.N., Bonfá, E., Carvalho, J.F. et al. Penile alterations with severe sperm abnormalities in antiphospholipid syndrome associated with systemic lupus erythematosus. Clin Rheumatol 32, 109–113 (2013). https://doi.org/10.1007/s10067-012-2083-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-012-2083-4