Abstract
Extracorporeal membrane oxygenation (ECMO) is an established therapy for primary graft dysfunction (PGD) in adults after lung transplant, while venovenous (VV) ECMO is an evolving therapy that can bridge patients to lung transplantation. This report describes a case of relatively quick improvement of grade 3 PGD, based on the PaO2/FIO2 (P/F) ratio, in a 17-year-old patient with cystic fibrosis who was bridged to lung transplantation with ambulatory VV ECMO and then received support with VV ECMO as a protective strategy during the initial phases of PGD after lung transplantation.
Similar content being viewed by others
Introduction
Recent innovations in extracorporeal membrane oxygenation (ECMO) technology have allowed the application of this mode of respiratory support to be used as a bridge to lung transplantation. The ability to apply venovenous (VV) ECMO through a bicaval dual lumen catheter inserted through a single access site via the jugular system has quickly become a useful treatment option for patients with hypercapnic respiratory failure. A single jugular cannula has been used to permit ambulation and maximize physical therapy while supported with VV ECMO, avoiding the complications from mechanical ventilation [1–4].
Primary graft dysfunction (PGD) is observed after lung transplantation and is believed to represent ischemia reperfusion injury. ECMO has been used to support patients after lung transplant that develop severe PGD, but this is normally instituted after PGD has manifested and respiratory failure/high PaO2/FIO2 (P/F) is present. In these cases, recovery from PGD can be protracted. As a preventative strategy against PGD after a complicated lung transplant due to massive intraoperative hemoptysis and prolonged native lung explantation, VV ECMO was continued in a 17-year-old patient with cystic fibrosis (CF) who was bridged to transplant with ambulatory VV ECMO.
Case report
A 17-year-old female (weight 38.7 kg, height 153 cm) with advanced bronchiectasis due to CF (sweat chloride 103 mEq/l, genetic mutations ∆F508/S549N) and pulmonary arterial hypertension [mean pulmonary artery pressure (PAP) of 32 mmHg] had a complicated 2-month hospitalization course with Achromobacter xylosoxidans pneumonia and Clostridium difficile colitis. Despite optimal medical management, her condition continued to deteriorate with the need for mechanical ventilation due to refractory hypercapnia; maximum PCO2 was 180 mmHg. Hypercapnia improved with mechanical ventilation to 110 mmHg, so we elected to bridge her to lung transplant with extracorporeal support. Although the pumpless interventional lung assist device NovaLung® has been well described as an effective means to bridge to lung transplantation [5], we elected to use VV ECMO in order to optimize ambulation and active physical therapy. Therefore, jugular single-venous VV ECMO was implemented with the placement of a 23-Fr bicaval dual-lumen catheter (Avalon Laboratories, LLC, Los Angeles, CA, USA). The ECMO circuit was a centrifugal pump (Rotaflow; Maquet Cardiopulmonary-AG, Hirrlingen, Germany) with an integrated battery for transport and a polymethylpentene membrane oxygenator (PLSQuadroxD; Maquet Cardiopulmonary-AG, Rastatt, Germany). On VV ECMO support, she was able to sit upright for long periods of time (Fig. 1) and was mobile and ambulated for short distances. The day after placing a bicaval dual-lumen catheter, a tracheostomy was placed for airway control and chest physiotherapy.
While on VV ECMO, anticoagulation was performed with heparin in accordance to Extracorporeal Life Support Organization (ELSO) recommendations with ACT ranging from 180 to 220 s. Eight days after the implementation of the VV ECMO, donor lungs were available, and she underwent bilateral sequential lung transplantation. Prior to beginning surgery, she developed a pulmonary hemorrhage. During cardiopulmonary bypass (CPB), the bicaval dual-lumen catheter was heplocked with ACT of >480 s. The ischemia time was 6 h because of the dissection of significant adhesions of her native lungs and right chest as a result of prior right upper lobectomy 6 years earlier. During the transplant, she had short periods of mild hemodynamic instability and required transfusion of 275 ml of packed red blood cells (PRBCs) and 307 ml of fresh frozen plasma. After completion of the transplant, she was continued on VV ECMO as an intervention to optimize her oxygenation and provide a margin of safety given her difficult operative course, transfusion requirements, and 6 h allograft ischemia time. After resuming VV ECMO, the initial arterial blood gas was pH 7.34, PCO2 43, and PO2 184. Over the next 24 h, her clinical course was consistent with PGD on the chest radiograph (Fig. 2), and the patient had an increased oxygen requirement on mechanical ventilation (PRVC mode, tidal volume 5 ml/kg, respiratory rate 20, PEEP 5 cmH2O, FIO2 60–80 %) with peak inspiratory pressures of 20–25 cmH2O. Furthermore, after the transplant, her mean PAP improved to 18 mmHg, and transthoracic echocardiography revealed normal cardiac function.
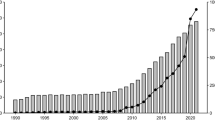
A total of 550 ml of PRBCs was transfused during her postoperative course in the intensive care unit. Her PGD reached a severity score of grade 3 with a nadir of her P/F ratio of 72 on POD 3. Despite the level of oxgenation based on her supplemental oxygen requirement, the P/F remained severely low for only 4 days (POD 1-4) as illustrated in Fig. 3 with rapid improvement occurring thereafter. In fact, the patient was tolerating being off mechanical ventilation on POD 5, so the bicaval dual-lumen catheter was replaced with a smaller catheter for venous access. She was ambulating on room air the following day on POD 6.
There was progressive escalation in her creatinine, starting on POD 8 with subsequent need for continuous venovenous hemofiltration (CVVH) on POD 11. The acute renal failure was due to medication-related acute tubular necrosis (combination of tacrolimus, furosemide, and tobramycin) with the development of oliguria and a peak in the creatinine level of 4.66 mg/dl (normal range 0.40–1.10 mg/dl) on POD 14. Her renal function eventually normalized at the time of discharge 6 weeks after transplant. Three months after transplantation, her spirometric measurements demonstrated forced vital capacity (FVC) 2.27 l (88 % predicted) and forced expiratory volume in 1 s (FEV1) 2.06 l (89 % predicted).
Discussion
The incidence and outcomes of PGD are inconsistent because of variable definitions of the disorder [6]. As a framework for research, the International Society for Heart and Lung Transplantation (ISHLT) Working Group on PGD proposed a standardized definition of PGD based on the P/F ratio and chest infiltrates assessed at time points up to 72 h as outlined in Table 1 [7]. Research investigating PGD grade 3 identifies an incidence ranging from 10 to 25 % with 30-day mortality being close to 50 % [8–12].
In the setting of complete cardiopulmonary support, conventional venoarterial (VA) ECMO is primarily used while primary respiratory failure, including severe oxygenation failure, is treated with VV ECMO. Over the last decade, ECMO has become an accepted rescue therapy for severe PGD after lung transplant [13–15]. Early implementation of ECMO decreased mortality in patients with PGD after transplant, despite the high incidence of multiple organ failure [14]. A review of the ELSO registry demonstrated a survival rate of 42 % (63/151) in lung transplant recipients (age 35 ± 18 years) with PGD who required ECMO [15]. A total of 151 ECMO cases were identified in the ESLO registry where lung transplant recipients with PGD were treated [15]. The mode of ECMO used was VV ECMO in 25 patients, VA ECMO in 89 patients, and other modes in 15 patients (unknown in 22 patients) [15]. Recently, the use of VV ECMO for the treatment of PGD in a large single-center study over an 8-year period found substantial improvement in the survival of patients with severe PGD with survival rates of 82 % at 30 days, 64 % at 1 year, and 49 % at 5 years [16].
Due to the recent outcomes of VV ECMO in treatment of PGD after lung transplant, the decision was made at the conclusion of the complicated transplant of the current patient to continue VV ECMO as a preventative measure. Because of the organ ischemia time, transfusion requirements, and prolonged CPB time, we anticipated the development of PGD; therefore, VV ECMO could potentially “protect” the allograft. The patient eventually manifested grade 3 PGD based on the P/F ratio with quick improvement (Fig. 3) with normal pulmonary function 3 months after transplant.
Factors that are commonly considered in determining whether ECMO should be used for PGD after lung transplantation include the patient's oxygenation status, hemodynamic stability, and surgeon preference. In this particular case, VV ECMO was used as a protective measure prospectively to take advantage of protective ventilation maneuvers during this initial period of PGD development after transplant. ECMO allowed avoidance of exposure of the new allograft to high ventilator settings in the first few days and during the most critical phases of progressing PGD. Based on the experiences with this patient, VV ECMO should be considered in the operating room after a complicated lung transplant as a protective strategy for PGD before transferring the patient to intensive care unit.
References
Garcia JP, Iacono A, Kon ZN, Griffith BP. Ambulatory extracorporeal membrane oxygenation: a new approach for bridge-to-lung transplantation. J Thorac Cardiovasc Surg. 2010;139:e137–9.
Mangi AA, Mason DP, Yun JJ, Murthy SC, Pettersson GB. Bridge to lung transplantation using short-term ambulatory extracorporeal membrane oxygenation. J Thorac Cardiovasc Surg. 2010;140:713–5.
Turner DA, Cheifetz IM, Rehder KJ, Williford WL, Bonadonna D, Banuelos SJ, Peterson-Carmichael S, Lin SS, Davis RD, Zaas D. Active rehabilitation and physical therapy during extracorporeal membrane oxygenation while awaiting lung transplantation: a practical approach. Crit Care Med. 2011;39:2593–8.
Hayes D Jr, Kukreja J, Tobias JD, Ballard HO, Hoopes CW. Ambulatory venovenous extracorporeal respiratory support as a bridge for cystic fibrosis patients to emergent lung transplantation. J Cyst Fibros. 2012;11:40–5.
Fischer S, Simon AR, Welte T, Hoeper MM, Meyer A, Tessmann R, Gohrbandt B, Gottlieb J, Haverich A, Strueber M. Bridge to lung transplantation with the novel pumpless interventional lung assist device NovaLung. J Thorac Cardiovasc Surg. 2006;131:719–23.
Arcasoy SM, Fisher A, Hachem RR, Scavuzzo M, Ware LB, ISHLT Working Group on Primary Lung Graft Dysfunction. Report of the ISHLT Working Group on Primary Lung Graft Dysfunction part V: predictors and outcomes. J Heart Lung Transplant. 2005;24:1483–8.
Christie JD, Carby M, Bag R, Corris P, Hertz M, Weill D, ISHLT Working Group on Primary Lung Graft Dysfunction. Report of the ISHLT working group on primary lung graft dysfunction part ii: definition. A consensus statement of the international society for heart and lung transplantation. J Heart Lung Transplant. 2005;24:1454–9.
Christie JD, Bavaria JE, Palevsky HI, Litzky L, Blumenthal NP, Kaiser LR, Kotloff RM. Primary graft failure following lung transplantation. Chest. 1998;114:51–60.
King RC, Binns OA, Rodriguez F, Kanithanon RC, Daniel TM, Spotnitz WD, Tribble CG, Kron IL. Reperfusion injury significantly impacts clinical outcome after pulmonary transplantation. Ann Thorac Surg. 2000;69:1681–5.
Christie JD, Kotloff RM, Pochettino A, Arcasoy SM, Rosengard BR, Landis JR, Kimmel SE. Clinical risk factors for primary graft failure following lung transplantation. Chest. 2003;124:1232–41.
Christie JD, Sager JS, Kimmel SE, Ahya VN, Gaughan C, Blumenthal NP, Kotloff RM. Impact of primary graft failure on outcomes following lung transplantation. Chest. 2005;127:161–5.
Fiser SM, Kron IL, McLendon Long S, Kaza AK, Kern JA, Tribble CG. Early intervention after severe oxygenation index elevation improves survival following lung transplantation. J Heart Lung Transplant. 2001;20:631–6.
Smits JM, Mertens BJ, Van Houwelingen HC, Haverich A, Persijn GG, Laufer G. Predictors of lung transplant survival in eurotransplant. Am J Transplant. 2003;3:1400–6.
Wigfield CH, Lindsey JD, Steffens TG, Edwards NM, Love RB. Early institution of extracorporeal membrane oxygenation for primary graft dysfunction after lung transplantation improves outcome. J Heart Lung Transplant. 2007;26:331–8.
Fischer S, Bohn D, Rycus P, Pierre AF, de Perrot M, Waddell TK, Keshavjee S. Extracorporeal membrane oxygenation for primary graft dysfunction after lung transplantation: analysis of the Extracorporeal Life Support Organization (ELSO) registry. J Heart Lung Transplant. 2007;26:472–7.
Hartwig MG, Walczak R, Lin SS, Davis RD. Improved survival but marginal allograft function in patients treated with extracorporeal membrane oxygenation after lung transplantation. Ann Thorac Surg. 2012;93:366–71.
Conflict of interest
There is no conflict of interest or disclosure for any of the authors with any companies/organizations whose products/services discussed in this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hayes, D., Galantowicz, M., Yates, A.R. et al. Venovenous ECMO as a bridge to lung transplant and a protective strategy for subsequent primary graft dysfunction. J Artif Organs 16, 382–385 (2013). https://doi.org/10.1007/s10047-013-0699-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10047-013-0699-z