Abstract
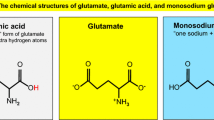
Glutamate is the major excitatory neurotransmitter of the Central Nervous System (CNS), and it is crucially needed for numerous key neuronal functions. Yet, excess glutamate causes massive neuronal death and brain damage by excitotoxicity—detrimental over activation of glutamate receptors. Glutamate-mediated excitotoxicity is the main pathological process taking place in many types of acute and chronic CNS diseases and injuries. In recent years, it became clear that not only excess glutamate can cause massive brain damage, but that several types of anti-glutamate receptor antibodies, that are present in the serum and CSF of subpopulations of patients with a kaleidoscope of human neurological diseases, can undoubtedly do so too, by inducing several very potent pathological effects in the CNS. Collectively, the family of anti-glutamate receptor autoimmune antibodies seem to be the most widespread, potent, dangerous and interesting anti-brain autoimmune antibodies discovered up to now. This impression stems from taking together the presence of various types of anti-glutamate receptor antibodies in a kaleidoscope of human neurological and autoimmune diseases, their high levels in the CNS due to intrathecal production, their multiple pathological effects in the brain, and the unique and diverse mechanisms of action by which they can affect glutamate receptors, signaling and effects, and subsequently impair neuronal signaling and induce brain damage. The two main families of autoimmune anti-glutamate receptor antibodies that were already found in patients with neurological and/or autoimmune diseases, and that were already shown to be detrimental to the CNS, include the antibodies directed against ionotorpic glutamate receptors: the anti-AMPA-GluR3 antibodies, anti-NMDA-NR1 antibodies and anti-NMDA-NR2 antibodies, and the antibodies directed against Metabotropic glutamate receptors: the anti-mGluR1 antibodies and the anti-mGluR5 antibodies. Each type of these anti-glutamate receptor antibodies is discussed separately in this very comprehensive review, with regards to: the human diseases in which these anti-glutamate receptor antibodies were found thus far, their presence and production in the nervous system, their association with various psychiatric/behavioral/cognitive/motor impairments, their possible association with certain infectious organisms, their detrimental effects in vitro as well as in vivo in animal models in mice, rats or rabbits, and their diverse and unique mechanisms of action. The review also covers the very encouraging positive responses to immunotherapy of some patients that have either of the above-mentioned anti-glutamate receptor antibodies, and that suffer from various neurological diseases/problems. All the above are also summarized in the review’s five schematic and useful figures, for each type of anti-glutamate receptor antibodies separately. The review ends with a summary of all the main findings, and with recommended guidelines for diagnosis, therapy, drug design and future investigations. In the nut shell, the human studies, the in vitro studies, as well as the in vivo studies in animal models in mice, rats and rabbit revealed the following findings regarding the five different types of anti-glutamate receptor antibodies: (1) Anti-AMPA-GluR3B antibodies are present in ~25–30 % of patients with different types of Epilepsy. When these anti-glutamate receptor antibodies (or other types of autoimmune antibodies) are found in Epilepsy patients, and when these autoimmune antibodies are suspected to induce or aggravate the seizures and/or the cognitive/psychiatric/behavioral impairments that sometimes accompany the seizures, the Epilepsy is called ‘Autoimmune Epilepsy’. In some patients with ‘Autoimmune Epilepsy’ the anti-AMPA-GluR3B antibodies associate significantly with psychiatric/cognitive/behavior abnormalities. In vitro and/or in animal models, the anti-AMPA-GluR3B antibodies by themselves induce many pathological effects: they activate glutamate/AMPA receptors, kill neurons by ‘Excitotoxicity’, and/or by complement activation modulated by complement regulatory proteins, cause multiple brain damage, aggravate chemoconvulsant-induced seizures, and also induce behavioral/motor impairments. Some patients with ‘Autoimmune Epilepsy’ that have anti-AMPA-GluR3B antibodies respond well (although sometimes transiently) to immunotherapy, and thanks to that have reduced seizures and overall improved neurological functions. (2) Anti-NMDA-NR1 antibodies are present in patients with autoimmune ‘Anti-NMDA-receptor Encephalitis’. In humans, in animal models and in vitro the anti-NMDA-NR1 antibodies can be very pathogenic since they can cause a pronounced decrease of surface NMDA receptors expressed in hippocampal neurons, and also decrease the cluster density and synaptic localization of the NMDA receptors. The anti-NMDA-NR1 antibodies induce these effects by crosslinking and internalization of the NMDA receptors. Such changes can impair glutamate signaling via the NMDA receptors and lead to various neuronal/behavior/cognitive/psychiatric abnormalities. Anti-NMDA-NR1 antibodies are frequently present in high levels in the CSF of the patients with ‘Anti-NMDA-receptor encephalitis’ due to their intrathecal production. Many patients with ‘Anti-NMDA receptor Encephalitis’ respond well to several modes of immunotherapy. (3) Anti-NMDA-NR2A/B antibodies are present in a substantial number of patients with Systemic Lupus Erythematosus (SLE) with or without neuropsychiatric problems. The exact percentage of SLE patients having anti-NMDA-NR2A/B antibodies varies in different studies from 14 to 35 %, and in one study such antibodies were found in 81 % of patients with diffuse ‘Neuropshychiatric SLE’, and in 44 % of patients with focal ‘Neuropshychiatric SLE’. Anti-NMDA-NR2A/B antibodies are also present in subpopulations of patients with Epilepsy of several types, Encephalitis of several types (e.g., chronic progressive limbic Encephalitis, Paraneoplastic Encephalitis or Herpes Simplex Virus Encephalitis), Schizophrenia, Mania, Stroke, or Sjorgen syndrome. In some patients, the anti-NMDA-NR2A/B antibodies are present in both the serum and the CSF. Some of the anti-NMDA-NR2A/B antibodies cross-react with dsDNA, while others do not. Some of the anti-NMDA-NR2A/B antibodies associate with neuropsychiatric/cognitive/behavior/mood impairments in SLE patients, while others do not. The anti-NMDA-NR2A/B antibodies can undoubtedly be very pathogenic, since they can kill neurons by activating NMDA receptors and inducing ‘Excitotoxicity’, damage the brain, cause dramatic decrease of membranal NMDA receptors expressed in hippocampal neurons, and also induce behavioral cognitive impairments in animal models. Yet, the concentration of the anti-NMDA-NR2A/B antibodies seems to determine if they have positive or negative effects on the activity of glutamate receptors and on the survival of neurons. Thus, at low concentration, the anti-NMDA-NR2A/B antibodies were found to be positive modulators of receptor function and increase the size of NMDA receptor-mediated excitatory postsynaptic potentials, whereas at high concentration they are pathogenic as they promote ‘Excitotoxcity’ through enhanced mitochondrial permeability transition. (4) Anti-mGluR1 antibodies were found thus far in very few patients with Paraneoplastic Cerebellar Ataxia, and in these patients they are produced intrathecally and therefore present in much higher levels in the CSF than in the serum. The anti-mGluR1 antibodies can be very pathogenic in the brain since they can reduce the basal neuronal activity, block the induction of long-term depression of Purkinje cells, and altogether cause cerebellar motor coordination deficits by a combination of rapid effects on both the acute and the plastic responses of Purkinje cells, and by chronic degenerative effects. Strikingly, within 30 min after injection of anti-mGluR1 antibodies into the brain of mice, the mice became ataxic. Anti-mGluR1 antibodies derived from patients with Ataxia also caused disturbance of eye movements in animal models. Immunotherapy can be very effective for some Cerebellar Ataxia patients that have anti-mGluR1 antibodies. (5) Anti-mGluR5 antibodies were found thus far in the serum and CSF of very few patients with Hodgkin lymphoma and Limbic Encephalopathy (Ophelia syndrome). The sera of these patients that contained anti-GluR5 antibodies reacted with the neuropil of the hippocampus and cell surface of live rat hippocampal neurons, and immunoprecipitation from cultured neurons and mass spectrometry demonstrated that the antigen was indeed mGluR5. Taken together, all these evidences show that anti-glutamate receptor antibodies are much more frequent among various neurological diseases than ever realized before, and that they are very detrimental to the nervous system. As such, they call for diagnosis, therapeutic removal or silencing and future studies. What we have learned by now about the broad family of anti-glutamate receptor antibodies is so exciting, novel, unique and important, that it makes all future efforts worthy and essential.





Similar content being viewed by others
References
Andrews PI, McNamara JO (1996) Rasmussen’s encephalitis: an autoimmune disorder? Curr Opin Neurobiol 6:673–678
Andrews PI, Dichter MA, Berkovic SF, Newton MR, McNamara JO (1996) Plasmapheresis in Rasmussen’s encephalitis. Neurology 46:242–246
Andrews PI, McNamara JO, Lewis DV (1997) Clinical and electroencephalographic correlates in Rasmussen’s encephalitis. Epilepsia 38:189–194
Ankarcrona M, Dypbukt JM, Bonfoco E, Zhivotovsky B, Orrenius S, Lipton SA, Nicotera P (1995) Glutamate-induced neuronal death: a succession of necrosis or apoptosis depending on mitochondrial function. Neuron 15:961–973
Antozzi C, Granata T, Aurisano N, Zardini G, Confalonieri P, Airaghi G, Mantegazza R, Spreafico R (1998) Long-term selective IgG immuno-adsorption improves Rasmussen’s encephalitis. Neurology 51:302–305
Appenzeller S (2011) NR2 antibodies in neuropsychiatric systemic lupus erythematosus. Rheumatology (Oxford) 50(9):1540–1541
Arinuma Y, Yanagida T, Hirohata S (2008) Association of cerebrospinal fluid anti-NR2 glutamate receptor antibodies with diffuse neuropsychiatric systemic lupus erythematosus. Arthritis Rheum 58(4):1130–1135
Asano NM, Coriolano MD, Asano BJ, Lins OG (2013) Psychiatric comorbidities in patients with systemic lupus erythematosus: a systematic review of the last 10 years. Rev Bras Rheumatol 53:431–437
Balosso S, Ravizza T, Pierucci M, Calcagno E, Invernizzi R, Di Giovanni G, Esposito E, Vezzani A (2009) Molecular and functional interactions between tumor necrosis factor-alpha receptors and the glutamatergic system in the mouse hippocampus: implications for seizure susceptibility. Neuroscience 161:293–300
Baltagi SA, Shoykhet M, Felmet K, Kochanek PM, Bell MJ (2010) Neurological sequelae of 2009 influenza A (H1N1) in children: a case series observed during a pandemic. Pediatr Crit Care Med 11:179–184
Baranzini SE, et al (2002) Analysis of antibody gene rearrangement, usage, and specificity in chronic focal encephalitis. Neurology 58(5):709–716
Basile AS, Koustova E, Ioan P, Rizzoli S, Rogawski MA, Usherwood PN (2001) IgG isolated from LP-BM5 infected mouse brain activates ionotropic glutamate receptors. Neurobiol Dis 8:1069–1081
Beneyto M, Kristiansen LV, Oni-Orisan A, McCullumsmith RE, Meador-Woodruff JH (2007) Abnormal glutamate receptor expression in the medial temporal lobe in schizophrenia and mood disorders. Neuropsychopharmacology 32:1888–1902
Berg AT, Langfitt JT, Testa FM, Levy SR, DiMario F, Westerveld M, Kulas J (2008) Global cognitive function in children with epilepsy: a community-based study. Epilepsia 49:608–614
Bernasconi P, Cipelletti B, Passerini L, Granata T, Antozzi C, Mantegazza R, Spreafico R (2002) Similar binding to glutamate receptors by Rasmussen and partial epilepsy patient’s sera. Neurology 59:1998–2001
Bien CG, Vincent A, Barnett MH, Becker AJ, Blumcke I, Graus F, Jellinger KA, Reuss DE, Ribalta T, Schlegel J, Sutton I, Lassmann H, Bauer J (2012) Immunopathology of autoantibody-associated encephalitides: clues for pathogenesis. Brain 135:1622–1638
Binnie CD (1993) Significance and management of transitory cognitive impairment due to subclinical EEG discharges in children. Brain Dev 15:23–30
Bonsi P, Cuomo D, De Persis C, Centonze D, Bernardi G, Calabresi P, Pisani A (2005) Modulatory action of metabotropic glutamate receptor (mGluR) 5 on mGluR1 function in striatal cholinergic interneurons. Neuropharmacology 49(Suppl 1):104–113
Borchers AT, Aoki CA, Naguwa SM, Keen CL, Shoenfeld Y, Gershwin ME (2005) Neuropsychiatric features of systemic lupus erythematosus. Autoimmun Rev 4:329–344
Cahn-Weiner DA, Wittenberg D, McDonald C (2009) Everyday cognition in temporal lobe and frontal lobe epilepsy. Epileptic Disord 11:222–227
Carlson NG, Gahring LC, Twyman RE, Rogers SW (1997) Identification of amino acids in the glutamate receptor, GluR3, important for antibody-binding and receptor-specific activation. J Biol Chem 272:11295–11301
Cheung MC, Chan AS, Chan YL, Lam JM, Lam W (2006) Effects of illness duration on memory processing of patients with temporal lobe epilepsy. Epilepsia 47:1320–1328
Chu Z, Hablitz JJ (2000) Quisqualate induces an inward current via mGluR activation in neocortical pyramidal neurons. Brain Res 879:88–92
Coesmans M, Smitt PA, Linden DJ, Shigemoto R, Hirano T, Yamakawa Y, van Alphen AM, Luo C, van der Geest JN, Kros JM, Gaillard CA, Frens MA, de Zeeuw CI (2003) Mechanisms underlying cerebellar motor deficits due to mGluR1-autoantibodies. Ann Neurol 53:325–336
Cohen-Kashi Malina K, Ganor Y, Levite M, Teichberg VI (2006) Autoantibodies against an extracellular peptide of the GluR3 subtype of AMPA receptors activate both homomeric and heteromeric AMPA receptor channels. Neurochem Res 31:1181–1190
Collingridge GL, Olsen RW, Peters J, Spedding M (2009) A nomenclature for ligand-gated ion channels. Neuropharmacology 56:2–5
Cusick MF, Libbey JE, Fujinami RS (2012) Molecular mimicry as a mechanism of autoimmune disease. Clin Rev Allergy Immunol 42:102–111
Dalmau J, Tuzun E, Wu HY, Masjuan J, Rossi JE, Voloschin A, Baehring JM, Shimazaki H, Koide R, King D, Mason W, Sansing LH, Dichter MA, Rosenfeld MR, Lynch DR (2007) Paraneoplastic anti-N-methyl-D-aspartate receptor encephalitis associated with ovarian teratoma. Ann Neurol 61:25–36
Dalmau J, Gleichman AJ, Hughes EG, Rossi JE, Peng X, Lai M, Dessain SK, Rosenfeld MR, Balice-Gordon R, Lynch DR (2008) Anti-NMDA-receptor encephalitis: case series and analysis of the effects of antibodies. Lancet Neurol 7:1091–1098
Dalmau J, Lancaster E, Martinez-Hernandez E, Rosenfeld MR, Balice-Gordon R (2011) Clinical experience and laboratory investigations in patients with anti-NMDAR encephalitis. Lancet Neurol 10:63–74
Dambinova SA, Khounteev GA, Izykenova GA, Zavolokov IG, Ilyukhina AY, Skoromets AA (2003) Blood test detecting autoantibodies to N-methyl-d-aspartate neuroreceptors for evaluation of patients with transient ischemic attack and stroke. Clin Chem 49:1752–1762
Dambinova SA, Bettermann K, Glynn T, Tews M, Olson D, Weissman JD, Sowell RL (2012) Diagnostic potential of the NMDA receptor peptide assay for acute ischemic stroke. PLoS ONE 7:e42362
Das S, Sasaki YF, Rothe T, Premkumar LS, Takasu M, Crandall JE, Dikkes P, Conner DA, Rayudu PV, Cheung W, Chen HS, Lipton SA, Nakanishi N (1998) Increased NMDA current and spine density in mice lacking the NMDA receptor subunit NR3A. Nature 393:377–381
de Graaff E, Maat P, Hulsenboom E, van den Berg R, van den Bent M, Demmers J, Lugtenburg PJ, Hoogenraad CC, Sillevis Smitt P (2012) Identification of delta/notch-like epidermal growth factor-related receptor as the Tr antigen in paraneoplastic cerebellar degeneration. Ann Neurol 71:815–824
DeGiorgio LA, Konstantinov KN, Lee SC, Hardin JA, Volpe BT, Diamond B (2001) A subset of lupus anti-DNA antibodies cross-reacts with the NR2 glutamate receptor in systemic lupus erythematosus. Nat Med 7(11):1189–1193
Dickerson F, Stallings C, Vaughan C, Origoni A, Khushalani S, Yolken R (2012) Antibodies to the glutamate receptor in mania. Bipolar Disord 14:547–553
Dingledine R, Borges K, Bowie D, Traynelis SF (1999) The glutamate receptor ion channels. Pharmacol Rev 51:7–61
Dracheva S, McGurk SR, Haroutunian V (2005) mRNA expression of AMPA receptors and AMPA receptor binding proteins in the cerebral cortex of elderly schizophrenics. J Neurosci Res 79:868–878
Elger CE, Helmstaedter C, Kurthen M (2004) Chronic epilepsy and cognition. Lancet Neurol 3:663–672
Endoh T (2004) Characterization of modulatory effects of postsynaptic metabotropic glutamate receptors on calcium currents in rat nucleus tractus solitarius. Brain Res 1024:212–224
Falsafi SK, Ghafari M, Pollak A, Hoger H, Lubec G (2012) Hippocampal AMPA-type receptor complexes containing GluR3 and GluR4 are paralleling training in the multiple T-Maze. Neurochem Int 60:425–430
Fanouriakis A, Boumpas DT, Bertsias GK (2013) Pathogenesis and treatment of CNS lupus. Curr Opin Rheumatol 25:577–583
Fastenau PS, Johnson CS, Perkins SM, Byars AW, deGrauw TJ, Austin JK, Dunn DW (2009) Neuropsychological status at seizure onset in children: risk factors for early cognitive deficits. Neurology 73:526–534
Faust TW, Chang EH, Kowal C, Berlin R, Gazaryan IG, Bertini E, Zhang J, Sanchez-Guerrero J, Fragoso-Loyo HE, Volpe BT, Diamond B, Huerta PT (2010) Neurotoxic lupus autoantibodies alter brain function through two distinct mechanisms. Proc Natl Acad Sci USA 107(43):18569–18574
Feichtinger M, Wiendl H, Korner E, Holl A, Gruber L, Fazekas F, Schrottner O, Eder H, Ott E (2006) No effect of immunomodulatory therapy in focal epilepsy with positive glutamate receptor type 3-antibodies. Seizure 15(5):350–354
Finke C, Kopp UA, Pruss H, Dalmau J, Wandinger KP, Ploner CJ (2012) Cognitive deficits following anti-NMDA receptor encephalitis. J Neurol Neurosurg Psychiatry 83:195–198
Florance NR, Davis RL, Lam C, Szperka C, Zhou L, Ahmad S, Campen CJ, Moss H, Peter N, Gleichman AJ, Glaser CA, Lynch DR, Rosenfeld MR, Dalmau J (2009) Anti-N-methyl-d-aspartate receptor (NMDAR) encephalitis in children and adolescents. Ann Neurol 66:11–18
Frassoni C, Spreafico R, Franceschetti S, Aurisano N, Bernasconi P, Garbelli R, Antozzi C, Taverna S, Granata T, Mantegazza R (2001) Labeling of rat neurons by anti-GluR3 IgG from patients with Rasmussen encephalitis. Neurology 57(2):324–327
Frechette ES, Zhou L, Galetta SL, Chen L, Dalmau J (2011) Prolonged follow-up and CSF antibody titers in a patient with anti-NMDA receptor encephalitis. Neurology 76:S64–S66
Gable MS, Gavali S, Radner A, Tilley DH, Lee B, Dyner L, Collins A, Dengel A, Dalmau J, Glaser CA (2009) Anti-NMDA receptor encephalitis: report of ten cases and comparison with viral encephalitis. Eur J Clin Microbiol Infect Dis 28:1421–1429
Gahring LC, Rogers SW (2002) Autoimmunity to glutamate receptors in the central nervous system. Crit Rev Immunol 22:295–316
Gahring LC, Carlson NG, Rogers SW (1998) Antibodies prepared to neuronal glutamate receptor subunit3 bind IFNalpha-receptors: implications for an autoimmune process. Autoimmunity 28:243–248
Ganor Y, Levite M (2012) Glutamate in the immune system: glutamate receptors in immune cells, potent effects, endogenous production and involvement in disease. In: Levite M (ed) Nerve-Driven immunity: Neurotransmitters and Neuropeptides in the Immune System. Springer, Vienna, pp 121–161
Ganor Y, Levite M (2014) The Neurotransmitter Glutamate and human T cells: Glutamate receptors and glutamate-induced direct and potent effects on normal human T cells, cancerous human leukemia and lymphoma T cells, and autoimmune human T cells. J Neural Transm (in press, Abstract available online)
Ganor Y, Besser M, Ben-Zakay N, Unger T, Levite M (2003) Human T cells express a functional ionotropic glutamate receptor GluR3, and glutamate by itself triggers integrin-mediated adhesion to laminin and fibronectin and chemotactic migration. J Immunol 170:4362–4372
Ganor Y, Goldberg-Stern H, Amrom D, Lerman-Sagie T, Teichberg VI, Pelled D, Futerman AH, Zeev BB, Freilinger M, Verheulpen D, Van Bogaert P, Levite M (2004) Autoimmune Epilepsy: some epilepsy patients harbor autoantibodies to glutamate receptors and dsDNA on both sides of the blood-brain barrier, which may kill neurons and decrease in brain fluids after hemispherotomy. Clin Dev Immunol 11:241–252
Ganor Y, Freilinger M, Dulac O, Levite M (2005a) Monozygotic twins discordant for epilepsy differ in the levels of potentially pathogenic autoantibodies and cytokines. Autoimmunity 38:139–150
Ganor Y, Golgberg-stern H, Lerman-Sagie T, Teichberg V, Levite M (2005b) Autoimmune Epilepsy: Distinct subpopulation of epilepsy patients harbor serum autoantibodies to either glutamate/AMPA receptor GluR3, glutamate/NMDA receptor subunit NR2A or double-stranded DNA. Epilepsy Res 65(1–2):11–22
Ganor Y, Gottlieb M, Eilam R, Otmy H, Teichberg V, Levite M (2005c) Immunization with the glutamate receptor derived peptide GluR3B induced neuronal death and reactive gliosis, but confer partial protection from pentylenetetrazole-induced seizures. Exp Neurol 195(1):92–102
Ganor Y, Goldberg-Stern H, Blank M, Shoenfeld Y, Dobrynina LA, Kalashnikova L, Levite M (2005d) Antibodies to glutamate receptor subtype 3 (GluR3) are found in some patients suffering from epilepsy as the main disease, but not in patients whose epilepsy accompanies antiphospholipid syndrome or Sneddon’s syndrome. Autoimmunity 38:417–424
Ganor Y, Teichberg VI, Levite M (2007) TCR activation eliminates glutamate receptor GluR3 from the cell surface of normal human T cells, via an autocrine/paracrine granzyme B-mediated proteolytic cleavage. J Immunol 178:683–692
Ganor Y, Grinberg I, Reis A, Cooper I, Goldstein RS, Levite M (2009) Human T-leukemia and T-lymphoma express glutamate receptor AMPA GluR3, and the neurotransmitter glutamate elevates the cancer-related matrix-metalloproteinases inducer CD147/EMMPRIN, MMP-9 secretion and engraftment of T-leukemia in vivo. Leuk Lymphoma 50:985–997
Ganor Y, Goldberg-Stern H, Cohen R, Teichberg V, Levite M (2014) Glutamate receptor antibodies directed against AMPA receptors subunit 3 peptide B (GluR3B) can be produced in DBA/2J mice, lower seizure threshold and induce abnormal behavior. Psychoneuroendocrinology 42:106–117
Gao HX, Sanders E, Tieng AT, Putterman C (2010) Sex and autoantibody titers determine the development of neuropsychiatric manifestations in lupus-prone mice. J Neuroimmunol 229(1–2):112–122
Goldberg-Stern H, Ganor Y, Cohen R, Pollak L, Teichberg VI, Levite M (2014) Glutamate receptor antibodies directed against AMPA receptors subunit 3 peptide B (GluR3B) associate with some cognitive/psychiatric/behavioral abnormalities in epilepsy patients. Psychoneuroendocrinology 40:221–231
Gono T, Kawaguchi Y, Kaneko H, Nishimura K, Hanaoka M, Kataoka S, Okamoto Y, Katsumata Y, Yamanaka H (2011) Anti-NR2A antibody as a predictor for neuropsychiatric systemic lupus erythematosus. Rheumatology (Oxford) 50(9):1578–1585
Granata T, Fusco L, Gobbi G, Freri E, Ragona F, Broggi G, Mantegazza R, Giordano L, Villani F, Capovilla G, Vigevano F, Bernardina BD, Spreafico R, Antozzi C (2003) Experience with immunomodulatory treatments in Rasmussen’s encephalitis. Neurology 61:1807–1810
Graus F, Dalmau J, Valldeoriola F, Ferrer I, Rene R, Marin C, Vecht CJ, Arbizu T, Targa C, Moll JW (1997) Immunological characterization of a neuronal antibody (anti-Tr) associated with paraneoplastic cerebellar degeneration and Hodgkin’s disease. J Neuroimmunol 74:55–61
Hahn BH (1993) An overview of the pathogenesis of systemic lupus erythematosus. In: Wallace DJ, Hahn BH (eds) Dubois’ lupus erythematosus. Williams and Wilkins, Philadelphia, pp 69–76
Hahn BH (1998) Antibodies to DNA. N Engl J Med 338:1359–1368
Hammack J, Kotanides H, Rosenblum MK, Posner JB (1992) Paraneoplastic cerebellar degeneration. II. Clinical and immunologic findings in 21 patients with Hodgkin’s disease. Neurology 42:1938–1943
Hanly JG, Robichaud J, Fisk JD (2006) Anti-NR2 glutamate receptor antibodies and cognitive function in systemic lupus erythematosus. J Rheumatol 33(8):1553–1558
Harrison MJ, Ravdin LD, Lockshin MD (2006) Relationship between serum NR2a antibodies and cognitive dysfunction in systemic lupus erythematosus. Arthritis Rheum 54(8):2515–2522
He XP, Patel M, Whitney KD, Janumpalli S, Tenner A, McNamara JO (1998) Glutamate receptor GluR3 antibodies and death of cortical cells. Neuron 20:153–163
Helmstaedter C (2002) Effects of chronic epilepsy on declarative memory systems. Prog Brain Res 135:439–453
Hermann BP, Seidenberg M, Schoenfeld J, Davies K (1997) Neuropsychological characteristics of the syndrome of mesial temporal lobe epilepsy. Arch Neurol 54:369–376
Hessen E, Lossius MI, Reinvang I, Gjerstad L (2006) Influence of major antiepileptic drugs on attention, reaction time, and speed of information processing: results from a randomized, double-blind, placebo-controlled withdrawal study of seizure-free epilepsy patients receiving monotherapy. Epilepsia 47:2038–2045
Hinoi E, Ogita K, Takeuchi Y, Ohashi H, Maruyama T, Yoneda Y (2001) Characterization with [3H]quisqualate of group I metabotropic glutamate receptor subtype in rat central and peripheral excitable tissues. Neurochem Int 38:277–285
Hofmann C, Baur MO, Schroten H (2010) Anti-NMDA receptor encephalitis after TdaP-IPV booster vaccination: cause or coincidence? J Neurol 258:500–501
Hollmann M, Heinemann S (1994) Cloned glutamate receptors. Annu Rev Neurosci 17:31–108
Holmes GL, Lenck-Santini PP (2006) Role of interictal epileptiform abnormalities in cognitive impairment. Epilepsy Behav 8:504–515
Hommet C, Sauerwein HC, De Toffol B, Lassonde M (2006) Idiopathic epileptic syndromes and cognition. Neurosci Biobehav Rev 30:85–96
Huerta PT, Kowal C, DeGiorgio LA, Volpe BT, Diamond B (2006) Immunity and behavior: antibodies alter emotion. Proc Natl Acad Sci USA 103(3):678–683
Huettner JE (2003) Kainate receptors and synaptic transmission. Prog Neurobiol 70:387–407
Hughes EG, Peng X, Gleichman AJ, Lai M, Zhou L, Tsou R, Parsons TD, Lynch DR, Dalmau J, Balice-Gordon RJ (2010) Cellular and synaptic mechanisms of anti-NMDA receptor encephalitis. J Neurosci 30:5866–5875
Husebye ES, Sthoeger ZM, Dayan M, Zinger H, Elbirt D, Levite M, Mozes E (2005) Autoantibodies to a NR2A peptide of the glutamate/NMDA receptor in sera of patients with systemic lupus erythematosus. Ann Rheum Dis 64(8):1210–1213
Iizuka T, Sakai F, Ide T, Monzen T, Yoshii S, Iigaya M, Suzuki K, Lynch DR, Suzuki N, Hata T, Dalmau J (2008) Anti-NMDA receptor encephalitis in Japan. Long-term outcome without tumor removal. Neurology 70(7):504–511
Irani SR, Vincent A (2011) NMDA receptor antibody encephalitis. Curr Neurol Neurosci Rep 11:298–304
Irani SR, Bera K, Waters P, Zuliani L, Maxwell S, Zandi MS, Friese MA, Galea I, Kullmann DM, Beeson D, Lang B, Bien CG, Vincent A (2010) N-methyl-D-aspartate antibody encephalitis: temporal progression of clinical and paraclinical observations in a predominantly non-paraneoplastic disorder of both sexes. Brain 133:1655–1667
Jokeit H, Ebner A (2002) Effects of chronic epilepsy on intellectual functions. Prog Brain Res 135:455–463
Kanner AM, Ostrovskaya A (2008a) Long-term significance of postictal psychotic episodes I. Are they predictive of bilateral ictal foci? Epilepsy Behav 12:150–153
Kanner AM, Ostrovskaya A (2008b) Long-term significance of postictal psychotic episodes II. Are they predictive of interictal psychotic episodes? Epilepsy Behav 12:154–156
Keinanen K, Wisden W, Sommer B, Werner P, Herb A, Verdoorn TA, Sakmann B, Seeburg PH (1990) A family of AMPA-selective glutamate receptors. Science 249:556–560
Kew JN, Kemp JA (2005) Ionotropic and metabotropic glutamate receptor structure and pharmacology. Psychopharmacology 179:4–29
Kleen JK, Scott RC, Holmes GL, Lenck-Santini PP (2010) Hippocampal interictal spikes disrupt cognition in rats. Ann Neurol 67:250–257
Koustova E, Sei Y, Fossom L, Wei ML, Usherwood PN, Keele NB, Rogawski MA, Basile AS (2001) LP-BM5 virus-infected mice produce activating autoantibodies to the AMPA receptor. J Clin Investig 107:737–744
Kowal C, Diamond B (2012) Aspects of CNS lupus: mouse models of anti-NMDA receptor antibody mediated reactivity. Methods Mol Biol 900:181–206
Kowal C, DeGiorgio LA, Nakaoka T, Hetherington H, Huerta PT, Diamond B, Volpe BT (2004) Cognition and immunity; antibody impairs memory. Immunity 21(2):179–188
Kowal C, Degiorgio LA, Lee JY, Edgar MA, Huerta PT, Volpe BT, Diamond B (2006) Human lupus autoantibodies against NMDA receptors mediate cognitive impairment. Proc Natl Acad Sci USA 103(52):19854–19859
Kozora E, West SG, Maier SF, Filley CM, Arciniegas DB, Brown M, Miller D, Grimm A, Zhang L (2010) Antibodies against N-methyl-D-aspartate receptors in patients with systemic lupus erythematosus without major neuropsychiatric syndromes. J Neurol Sci 295(1–2):87–91
Lancaster E, Martinez-Hernandez E, Titulaer MJ, Boulos M, Weaver S, Antoine JC, Liebers E, Kornblum C, Bien CG, Honnorat J, Wong S, Xu J, Contractor A, Balice-Gordon R, Dalmau J (2011) Antibodies to metabotropic glutamate receptor 5 in the Ophelia syndrome. Neurology 77:1698–1701
Lapteva L, Nowak M, Yarboro CH, Takada K, Roebuck-Spencer T, Weickert T, Bleiberg J, Rosenstein D, Pao M, Patronas N, Steele S, Manzano M, van der Veen JW, Lipsky PE, Marenco S, Wesley R, Volpe B, Diamond B, Illei GG (2006) Anti-N-methyl-D-aspartate receptor antibodies, cognitive dysfunction, and depression in systemic lupus erythematosus. Arthritis Rheum 54(8):2505–2514
Lauvsnes MB, Omdal R (2012) Systemic lupus erythematosus, the brain, and anti-NR2 antibodies. J Neurol 259(4):622–629
Lauvsnes MB, Maroni SS, Appenzeller S, Beyer MK, Greve OJ, Kvaloy JT, Harboe E, Goransson LG, Tjensvoll AB, Omdal R (2013) Memory dysfunction in primary Sjogren’s syndrome is associated with anti-NR2 antibodies. Arthritis Rheum 65(12):3209–3217
Leach JP, Chadwick DW, Miles JB, Hart IK (1999) Improvement in adult-onset Rasmussen’s encephalitis with long-term immunomodulatory therapy. Neurology 52:738–742
Lerma J (2006) Kainate receptor physiology. Curr Opin Pharmacol 6:89–97
Levite M (2002) Autoimmune Epilepsy. Nat Immunol 3:500
Levite M (2008) Neurotransmitters activate T-cells and elicit crucial functions via neurotransmitter receptors. Curr Opin Pharmacol 8:460–471
Levite M, Ganor Y (2008) Autoantibodies to glutamate receptors can damage the brain in Epilepsy, Systemic Lupus Erythematosus and Encephalitis. Expert Rev Neurother 8:1141–1160
Levite M, Hart IK (2002) Immunotherapy for Epilepsy. Expert Rev Neurother 2:804–819
Levite M, Hermelin A (1999) Autoimmunity to the glutamate receptor in mice - a model for Rasmussen’s encephalitis? J Autoimmun 13:73–82
Levite M, Fleidervish IA, Schwarz A, Pelled D, Futerman AH (1999) Autoantibodies to the glutamate receptor kill neurons via activation of the receptor ion channel. J Autoimmun 13:61–72
Li F, Tsien JZ (2009) Memory and the NMDA receptors. N Engl J Med 361:302–303
Li Y, Uccelli A, Laxer KD, Jeong MC, Vinters HV, Tourtellotte WW, Hauser SL, Oksenberg JR (1997) Local-clonal expansion of infiltrating T lymphocytes in chronic encephalitis of Rasmussen. J Immunol 158:1428–1437
Loscher W (2002) Animal models of epilepsy for the development of antiepileptogenic and disease-modifying drugs. A comparison of the pharmacology of kindling and post-status epilepticus models of temporal lobe epilepsy. Epilepsy Res 50:105–123
Maneta E, Garcia G (2013) Psychiatric manifestations of anti-NMDA receptor encephalitis: neurobiological underpinnings and differential diagnostic implications. Psychosomatics 55(1):37–44
Manev H, Favaron M, Guidotti A, Costa E (1989) Delayed increase of Ca2+ influx elicited by glutamate: role in neuronal death. Mol Pharmacol 36:106–112
Mantegazza R, Bernasconi P, Baggi F, Spreafico R, Ragona F, Antozzi C, Bernardi G, Granata T (2002) Antibodies against GluR3 peptides are not specific for Rasmussen’s encephalitis but are also present in epilepsy patients with severe, early onset disease and intractable seizures. J Neuroimmunol 131(1–2):179–185
Manto M, Dalmau J, Didelot A, Rogemond V, Honnorat J (2010) In vivo effects of antibodies from patients with anti-NMDA receptor encephalitis: further evidence of synaptic glutamatergic dysfunction. Orphanet J Rare Dis 5:31
Manto M, Dalmau J, Didelot A, Rogemond V, Honnorat J (2011) Afferent facilitation of corticomotor responses is increased by IgGs of patients with NMDA-receptor antibodies. J Neurol 258:27–33
Marignier R, Chenevier F, Rogemond V, Sillevis Smitt P, Renoux C, Cavillon G, Androdias G, Vukusic S, Graus F, Honnorat J, Confavreux C (2010) Metabotropic glutamate receptor type 1 autoantibody-associated cerebellitis: a primary autoimmune disease? Arch Neurol 67:627–630
Masu M, Tanabe Y, Tsuchida K, Shigemoto R, Nakanishi S (1991) Sequence and expression of a metabotropic glutamate receptor. Nature 349:760–765
Mat A, Adler H, Merwick A, Chadwick G, Gullo G, Dalmau JO, Tubridy N (2013) Ophelia syndrome with metabotropic glutamate receptor 5 antibodies in CSF. Neurology 80:1349–1350
Mathern GW, Pretorius JK, Leite JP, Kornblum HI, Mendoza D, Lozada A, Bertram EH 3rd (1998) Hippocampal AMPA and NMDA mRNA levels and subunit immunoreactivity in human temporal lobe epilepsy patients and a rodent model of chronic mesial limbic epilepsy. Epilepsy Res 32:154–171
Mayer ML (2005) Glutamate receptor ion channels. Curr Opin Neurobiol 15:282–288
Mayer ML (2011a) Emerging models of glutamate receptor ion channel structure and function. Structure 19:1370–1380
Mayer ML (2011b) Structure and mechanism of glutamate receptor ion channel assembly, activation and modulation. Curr Opin Neurobiol 21:283–290
Meldrum BS (1994) The role of glutamate in epilepsy and other CNS disorders. Neurology 44:S14–S23
Meldrum BS (2000) Glutamate as a neurotransmitter in the brain: review of physiology and pathology. J Nutr 130:1007S–1015S
Miyamoto M, Tsuboi Y, Honda K, Kobayashi M, Takamiya K, Huganir RL, Kondo M, Shinoda M, Sessle BJ, Katagiri A, Kita D, Suzuki I, Oi Y, Iwata K (2012) Involvement of AMPA receptor GluR2 and GluR3 trafficking in trigeminal spinal subnucleus caudalis and C1/C2 neurons in acute-facial inflammatory pain. PLoS ONE 7:e44055
Nabbout R (2012) Autoimmune and inflammatory epilepsies. Epilepsia 53(Suppl 4):58–62
Nakajima H, Hosoya M, Takahashi Y, Matsuyama K, Tagami M, Ishida S, Furutama D, Sugino M, Kimura F, Shinoda K, Hanafusa T (2007) A chronic progressive case of enteroviral limbic encephalitis associated with autoantibody to glutamate receptor epsilon2. Eur Neurol 57:238–240
Nicolai J, Aldenkamp AP, Arends J, Weber JW, Vles JS (2006) Cognitive and behavioral effects of nocturnal epileptiform discharges in children with benign childhood epilepsy with centrotemporal spikes. Epilepsy Behav 8:56–70
Ohashi H, Maruyama T, Higashi-Matsumoto H, Nomoto T, Nishimura S, Takeuchi Y (2002) A novel binding assay for metabotropic glutamate receptors using [3H] l-quisqualic acid and recombinant receptors. Z Naturforsch C 57:348–355
Okamoto S, Hirano T, Takahashi Y, Yamashita T, Uyama E, Uchino M (2007) Paraneoplastic limbic encephalitis caused by ovarian teratoma with autoantibodies to glutamate receptor. Intern Med 46:1019–1022
Okubo Y, Sekiya H, Namiki S, Sakamoto H, Iinuma S, Yamasaki M, Watanabe M, Hirose K, Iino M (2010) Imaging extrasynaptic glutamate dynamics in the brain. Proc Natl Acad Sci USA 107:6526–6531
Olney JW (1990) Excitotoxicity: an overview. Can Dis Wkly Rep 16(Suppl 1E):47–57 discussion 57–58
Omdal R, Brokstad K, Waterloo K, Koldingsnes W, Jonsson R, Mellgren SI (2005) Neuropsychiatric disturbances in SLE are associated with antibodies against NMDA receptors. Eur J Neurol 12(5):392–398
Pin JP, Bockaert J (1995) Get receptive to metabotropic glutamate receptors. Curr Opin Neurobiol 5:342–349
Platt SR (2007) The role of glutamate in central nervous system health and disease—a review. Vet J 173:278–286
Pollak TA, McCormack R, Peakman M, Nicholson TR, David AS (2013) Prevalence of anti-N-methyl-D-aspartate (NMDA) antibodies in patients with schizophrenia and related psychoses: a systematic review and meta-analysis. Psychol Med, pp 1–13
Porter BE, Cui XN, Brooks-Kayal AR (2006) Status epilepticus differentially alters AMPA and kainate receptor subunit expression in mature and immature dentate granule neurons. Eur J Neurosci 23:2857–2863
Pruss H, Dalmau J, Arolt V, Wandinger KP (2010) Anti-NMDA-receptor encephalitis. An interdisciplinary clinical picture. Nervenarzt 81:396, 398, 400, passim
Pruss H, Finke C, Holtje M, Hofmann J, Klingbeil C, Probst C, Borowski K, Ahnert-Hilger G, Harms L, Schwab JM, Ploner CJ, Komorowski L, Stoecker W, Dalmau J, Wandinger KP (2012a) N-methyl-D-aspartate receptor antibodies in herpes simplex encephalitis. Ann Neurol 72:902–911
Pruss H, Holtje M, Maier N, Gomez A, Buchert R, Harms L, Ahnert-Hilger G, Schmitz D, Terborg C, Kopp U, Klingbeil C, Probst C, Kohler S, Schwab JM, Stoecker W, Dalmau J, Wandinger KP (2012b) IgA NMDA receptor antibodies are markers of synaptic immunity in slow cognitive impairment. Neurology 78:1743–1753
Rasmussen T, Olszewski J, Lloydsmith D (1958) Focal seizures due to chronic localized encephalitis. Neurology 8:435–445
Rheumatology TA (1999) The American College of Rheumatology nomenclature and case definitions for neuropsychiatric lupus syndromes. Arthritis Rheum 42:599–608
Rice JS, Kowal C, Volpe BT, DeGiorgio LA, Diamond B (2005) Molecular mimicry: anti-DNA antibodies bind microbial and nonnucleic acid self-antigens. Curr Top Microbiol Immunol 296:137–151
Roebling R, Scheerer N, Uttner I, Gruber O, Kraft E, Lerche H (2009) Evaluation of cognition, structural, and functional MRI in juvenile myoclonic epilepsy. Epilepsia 50:2456–2465
Rogers SW, Andrews PI, Gahring LC, Whisenand T, Cauley K, Crain B, Hughes TE, Heinemann SF, McNamara JO (1994) Autoantibodies to glutamate receptor GluR3 in Rasmussen’s encephalitis. Science 265:648–651
Rosenmund C, Stern-Bach Y, Stevens CF (1998) The tetrameric structure of a glutamate receptor channel. Science 280:1596–1599
Roubertie A, Boukhaddaoui H, Sieso V, de Saint-Martin A, Lellouch-Tubiana A, Hirsch E, Echenne B, Valmier J (2005) Antiglial cell autoantibodies and childhood epilepsy: a case report. Epilepsia 46(8):1308–1312
Sansing LH, Tuzun E, Ko MW, Baccon J, Lynch DR, Dalmau J (2007) A patient with encephalitis associated with NMDA receptor antibodies. Nat Clin Pract Neurol 3:291–296
Sato S, Kawashima H, Hoshika A, Yoshio T (2011) Clinical analysis of anti-NR2 glutamate receptor antibodies and interleukin-6 with neuropsychiatric systemic lupus erythematosus. Rheumatology (Oxford) 50(11):2142–2144
Shehata GA, Bateh Ael A (2009) Cognitive function, mood, behavioral aspects, and personality traits of adult males with idiopathic epilepsy. Epilepsy Behav 14:121–124
Shewmon DA, Erwin RJ (1988) The effect of focal interictal spikes on perception and reaction time I. General considerations. Electroencephalogr Clin Neurophysiol 69:319–337
Sillevis Smitt P, Kinoshita A, De Leeuw B, Moll W, Coesmans M, Jaarsma D, Henzen-Logmans S, Vecht C, De Zeeuw C, Sekiyama N, Nakanishi S, Shigemoto R (2000) Paraneoplastic cerebellar ataxia due to autoantibodies against a glutamate receptor. N Engl J Med 342:21–27
Sladeczek F, Momiyama A, Takahashi T (1993) Presynaptic inhibitory action of a metabotropic glutamate receptor agonist on excitatory transmission in visual cortical neurons. Proc Biol Sci 253:297–303
Solaro C, Mantegazza R, Bacigalupo A, Uccelli A (2006) Intractable myoclonus associated with anti-GluR3 antibodies after allogeneic bone marrow transplantation. Haematologica 91(12 Suppl):ECR62
Steiner J, Walter M, Glanz W, Sarnyai Z, Bernstein HG, Vielhaber S, Kastner A, Skalej M, Jordan W, Schiltz K, Klingbeil C, Wandinger KP, Bogerts B, Stoecker W (2013) Increased prevalence of diverse N-methyl-D-aspartate glutamate receptor antibodies in patients with an initial diagnosis of schizophrenia: specific relevance of IgG NR1a antibodies for distinction from N-methyl-d-aspartate glutamate receptor encephalitis. JAMA Psychiatry 70:271–278
Steup-Beekman G, Steens S, van Buchem M, Huizinga T (2007) Anti-NMDA receptor autoantibodies in patients with systemic lupus erythematosus and their first-degree relatives. Lupus 16(5):329–334
Takahashi Y, Matsuda K, Kubota Y, Shimomura J, Yamasaki E, Kudo T, Fukushima K, Osaka H, Akasaka N, Imamura A, Yamada S, Kondo N, Fujiwara T (2006) Vaccination and infection as causative factors in Japanese patients with Rasmussen syndrome: molecular mimicry and HLA class I. Clin Dev Immunol 13:381–387
Tanabe Y, Masu M, Ishii T, Shigemoto R, Nakanishi S (1992) A family of metabotropic glutamate receptors. Neuron 8:169–179
Thanou A, Merrill JT (2014) Treatment of systemic lupus erythematosus: new therapeutic avenues and blind alleys. Nat Rev Rheumatol 10:23–34
Theodore WH, Bhatia S, Hatta J, Fazilat S, DeCarli C, Bookheimer SY, Gaillard WD (1999) Hippocampal atrophy, epilepsy duration, and febrile seizures in patients with partial seizures. Neurology 52:132–136
Tomita M, Khan RL, Blehm BH, Santoro TJ (2004) The potential pathogenetic link between peripheral immune activation and the central innate immune response in neuropsychiatric systemic lupus erythematosus. Med Hypotheses 62:325–335
Tomiyama M, Furusawa K, Kamijo M, Kimura T, Matsunaga M, Baba M (2005) Upregulation of mRNAs coding for AMPA and NMDA receptor subunits and metabotropic glutamate receptors in the dorsal horn of the spinal cord in a rat model of diabetes mellitus. Brain Res Mol Brain Res 136:275–281
Twyman RE, Gahring LC, Spiess J, Rogers SW (1995) Glutamate receptor antibodies activate a subset of receptors and reveal an agonist binding site. Neuron 14:755–762
Tziperman B, Garty BZ, Schoenfeld N, Hoffer V, Watemberg N, Lev D, Ganor Y, Levite M, Lerman-Sagie T (2007) Acute intermittent porphyria, Rasmussen encephalitis, or both? J Child Neurol 22(1):99–105
Verhelst H, Verloo P, Dhondt K, De Paepe B, Menten B, Dalmau J, Van Coster R (2010) Anti-NMDA-receptor encephalitis in a 3 year old patient with chromosome 6p21.32 microdeletion including the HLA cluster. Eur J Paediatr Neurol 15:163–166
Villani F, Avanzini G (2002) The use of immunoglobulins in the treatment of human epilepsy. Neurol Sci 23(Suppl 1):S33–S37
Villani F, Spreafico R, Farina L, Giovagnoli AR, Bernasconi P, Granata T, Avanzini G (2001) Positive response to immunomodulatory therapy in an adult patient with Rasmussen’s encephalitis. Neurology 56:248–250
Watson R, Jiang Y, Bermudez I, Houlihan L, Clover L, McKnight K, Cross JH, Hart IK, Roubertie A, Valmier J, Hart Y, Palace J, Beeson D, Vincent A, Lang B (2004) Absence of antibodies to glutamate receptor type 3 (GluR3) in Rasmussen encephalitis. Neurology 63:43–50
Weissman JD, Khunteev GA, Heath R, Dambinova SA (2011) NR2 antibodies: risk assessment of transient ischemic attack (TIA)/stroke in patients with history of isolated and multiple cerebrovascular events. J Neurol Sci 300:97–102
Whitney KD, McNamara JO (2000) GluR3 autoantibodies destroy neural cells in a complement-dependent manner modulated by complement regulatory proteins. J Neurosci 20:7307–7316
Wiendl H, Bien CG, Bernasconi P, Fleckenstein B, Elger CE, Dichgans J, Mantegazza R, Melms A (2001) GluR3 antibodies: prevalence in focal epilepsy but no specificity for Rasmussen’s encephalitis. Neurology 57(8):1511–1514
Winchester RJ (1996) Systemic lupus erythematosus pathogenesis. In: Koopman W (ed) Arthritis and allied conditions. Williams andWilkins, Birmingham, pp 1361–1391
Yoshio T, Okamoto H, Hirohata S, Minota S (2013) IgG anti-NR2 glutamate receptor autoantibodies from patients with systemic lupus erythematosus activate endothelial cells. Arthritis Rheum 65(2):457–463
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Levite, M. GLUTAMATE RECEPTOR ANTIBODIES IN NEUROLOGICAL DISEASES: Anti-AMPA-GluR3 antibodies, Anti-NMDA-NR1 antibodies, Anti-NMDA-NR2A/B antibodies, Anti-mGluR1 antibodies or Anti-mGluR5 antibodies are present in subpopulations of patients with either: Epilepsy, Encephalitis, Cerebellar Ataxia, Systemic Lupus Erythematosus (SLE) and Neuropsychiatric SLE, Sjogren’s syndrome, Schizophrenia, Mania or Stroke. These autoimmune anti-glutamate receptor antibodies can bind neurons in few brain regions, activate glutamate receptors, decrease glutamate receptor’s expression, impair glutamate-induced signaling and function, activate Blood Brain Barrier endothelial cells, kill neurons, damage the brain, induce behavioral/psychiatric/cognitive abnormalities and Ataxia in animal models, and can be removed or silenced in some patients by immunotherapy. J Neural Transm 121, 1029–1075 (2014). https://doi.org/10.1007/s00702-014-1193-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00702-014-1193-3
Keywords
- Anti-glutamate receptor antibodies
- Anti-GluR3 antibodies
- Anti-NR2 antibodies
- Anti-NR1 antibodies
- Glutamate
- Glutamate receptors
- AMPA
- NMDA
- GluR3
- GluR3B
- NMDA-NR1
- NMDA-NR2
- NMDA-NR2A/B
- mGluR1
- mGluR5
- Epilepsy
- Autoimmune Epilepsy
- NMDA encephalitis
- Anti-NMDA receptor Encephalitis
- Encephalitis
- Systemic Lupus Erythematosus (SLE)
- Neuropsychiatric lupus
- Neuropsychiatric Sjogren's Syndrome
- Schizophrenia
- Seizures
- Mania
- Stroke
- Paraneoplastic cerebellar ataxia
- Ophelia syndrome
- Immunotherapy for Epilepsy
- Neuropsychiatric impairments