Abstract
Purpose
Early postoperative mobilization is crucial for early ambulation to reduce postoperative pulmonary complications after lung resection. However, orthostatic intolerance (OI) may delay patient recovery, leading to complications. It is therefore important to understand the prevalence of and predisposing factors for OI following video-assisted thoracic surgery (VATS), which have not been established. This study evaluated the incidence of OI, impact of OI on delayed ambulation, and predisposing factors associated with OI in patients after VATS.
Methods
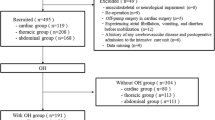
This retrospective cohort study consecutively analyzed data from 236 patients who underwent VATS. The primary outcome was defined as OI with symptoms associated with ambulatory challenge on postoperative day 1 (POD1), including dizziness, nausea and vomiting, feeling hot, blurred vision, or transient syncope. Multivariate logistic regression was performed to identify independent factors associated with OI.
Results
Of the 236 patients, 35.2 % (83) experienced OI; 45.8 % of these could not ambulate at POD1, compared with 15.7 % of patients without OI (P < 0.001). Factors independently associated with OI included advanced age [odds ratio 2.83 (1.46–5.58); P = 0.002], female gender [odds ratio 2.40 (1.31–4.46); P = 0.004], and postoperative opioid use [odds ratio 2.61 (1.23–5.77); P = 0.012]. Use of thoracic epidural anesthesia was not independently associated with OI [odds ratio 0.72 (0.38–1.37); P = 0.318].
Conclusion
Postoperative OI was common in patients after VATS and significantly associated with delayed ambulation. Advanced age, female gender, and postoperative opioid use were identified as independent predisposing factors for OI.
Similar content being viewed by others
References
Kehlet H. Multimodal approach to control postoperative pathophysiology and rehabilitation. Br J Anaesth. 1997;78:606–17.
Khoo CK, Vickery CJ, Forsyth N, Vinall NS, Eyre-Brook IA. A prospective randomized controlled trial of multimodal perioperative management protocol in patients undergoing elective colorectal resection for cancer. Ann Surg. 2007;245:867–72.
Wind J, Polle SW, Fung Kon Jin PH, Dejong CH, von Meyenfeldt MF, Ubbink DT, Gouma DJ, Bemelman WA, Laparoscopy and/or Fast Track Multimodal Management Versus Standard Care (LAFA) Study Group, Enhanced Recovery after Surgery (ERAS) Group. Systematic review of enhanced recovery programmes in colonic surgery. Br J Surg. 2006;93:800–9.
Grubb BP. Neurocardiogenic syncope and related disorders of orthostatic intolerance. Circulation. 2005;111:2997–3006.
Chung F, Mezei G. Factors contributing to a prolonged stay after ambulatory surgery. Anesth Analg. 1999;89:1352–9.
Bundgaard-Nielsen M, Jørgensen CC, Jørgensen TB, Ruhnau B, Secher NH, Kehlet H. Orthostatic intolerance and the cardiovascular response to early postoperative mobilization. Br J Anaesth. 2009;102:756–62.
Jans O, Bundgaard-Nielsen M, Solgaard S, Johansson PI, Kehlet H. Orthostatic intolerance during early mobilization after fast-track hip arthroplasty. Br J Anaesth. 2012;108:436–43.
Iwata Y, Mizota Y, Mizota T, Koyama T, Shichino T. Postoperative continuous intravenous infusion of fentanyl is associated with the development of orthostatic intolerance and delayed ambulation in patients after gynecologic laparoscopic surgery. J Anesth. 2012;26:503–8.
Auriant I, Jallot A, Hervé P, Cerrina J, Le Roy Ladurie F, Fournier JL, Lescot B, Parquin F. Noninvasive ventilation reduces mortality in acute respiratory failure following lung resection. Am J Respir Crit Care Med. 2001;164:1231–5.
Muehling BM, Halter GL, Schelzig H, Meierhenrich R, Steffen P, Sunder-Plassmann L, Orend KH. Reduction of postoperative pulmonary complications after lung surgery using a fast track clinical pathway. Eur J Cardiothorac Surg. 2008;34:174–80.
Joshi GP, Bonnet F, Shah R, Wilkinson RC, Camu F, Fischer B, Neugebauer EA, Rawal N, Schug SA, Simanski C, Kehlet H. A systematic review of randomized trials evaluating regional techniques for postthoracotomy analgesia. Anesth Analg. 2008;107:1026–40.
Gan TJ. Risk factors for postoperative nausea and vomiting. Anesth Analg. 2006;102:1884–98.
de Leon-Casasola OA, Lema MJ. Postoperative epidural opioid analgesia: what are the choices? Anesth Analg. 1996;83:867–75.
Tschernko EM, Hofer S, Bieglmayer C, Wisser W, Haider W. Early postoperative stress: video-assisted wedge resection/lobectomy vs. conventional axillary thoracotomy. Chest. 1996;109:1636–42.
Perttunen K, Nilsson E, Kalso E. i.v. diclofenac and ketorolac for pain after thoracoscopic surgery. Br J Anaesth. 1999;82:221–7.
Hill SE, Keller RA, Stafford-Smith M, Grichnik K, White WD, D’Amico TA, Newman MF. Efficacy of single-dose, multilevel paravertebral nerve blockade for analgesia after thoracoscopic procedures. Anesthesiology. 2006;104:1047–53.
Fiorelli A, Vicidomini G, Laperuta P, Busiello L, Perrone A, Napolitano F, Messina G, Santini M. Pre-emptive local analgesia in video-assisted thoracic surgery sympathectomy. Eur J Cardiothorac Surg. 2010;37:588–93.
Acknowledgments
The authors thank Enago (http://www.enago.jp) for the English language review.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Mizota, T., Iwata, Y., Daijo, H. et al. Orthostatic intolerance during early mobilization following video-assisted thoracic surgery. J Anesth 27, 895–900 (2013). https://doi.org/10.1007/s00540-013-1634-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-013-1634-4