Abstract
Objectives
The goal of this study was to investigate the effects of spaced versus massed practice on skill acquisition and retention in the context of laparoscopic motor skill training.
Background
Reaching proficiency in performing laparoscopic surgery involves extensive training to acquire the required motor skills. Conventionally, training of such skills occurs during a full day training event utilizing surgical simulators that train specific motor skills pertinent to laparoscopic surgery. An important variable to consider is the optimal schedule for laparoscopic motor training.
Methods
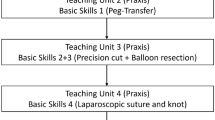
In this study, two groups of trainees without prior experience were trained on a variety of physical box-trainer tasks on different time-schedules. One group received three 75-min training sessions on a single day (massed condition) and the other received one 75-min training session per week for three consecutive weeks (spaced condition). Short- and long-term retention were assessed 2 weeks and 1 year after the completion of training.
Results
Outcome measures indicated better performance at the end of training, at a 2-week delayed retention session and at a 1-year retention session for the group that received training on a spaced schedule. This spacing effect was most pronounced for the more difficult laparoscopic training tasks such as intra-corporeal suturing. On average, 21 % of participants in the massed group and 65 % in the spaced group reached proficiency by the end of training.
Conclusions
Spacing practice of laparoscopic motor skill training will facilitate skill acquisition, short-term and long-term retention, and thus, a more efficient learning process for trainees. Though more challenging in terms of logistics, training courses in medical centers should distribute practice sessions over longer time intervals.



Similar content being viewed by others
References
Gallagher Anthony G et al (2005) Virtual reality simulation for the operating room: proficiency-based training as a paradigm shift in surgical skills training. Ann Surg 241(2):364
Gauger Paul G et al (2010) Laparoscopic simulation training with proficiency targets improves practice and performance of novice surgeons. Am J Surg 199(1):72–80
Stefanidis D et al (2007) Closing the gap in operative performance between novices and experts: does harder mean better for laparoscopic simulator training? J Am Coll Surg 205:307–313
Stefanidis Dimitrios, Todd Heniford B (2009) The formula for a successful laparoscopic skills curriculum. Arch Surg 144(1):77
Adams JA (1987) Historical review and appraisal of research on the learning, retention, and transfer of human motor skills. Psychol Bull 101:41
Spruit EN et al. (2013) Optimal training design for procedural motor skills: a review and application to laparoscopic surgery. Psychol Res 1–14
Benjamin Aaron S, Tullis Jonathan (2010) What makes distributed practice effective? Cogn Psychol 61(3):228–247
Rosenbaum David A, Carlson Richard A, Gilmore Rick O (2001) Acquisition of intellectual and perceptual-motor skills. Annu Rev Psychol 52(1):453–470
Cepeda Nicholas J et al (2006) Distributed practice in verbal recall tasks: a review and quantitative synthesis. Psychol Bull 132(3):354
McDaniel M (2012) Put the SPRINT in knowledge training: training with SPacing, Retrieval, and INTerleaving. In: Healy AF, LE Bourne (eds) Training cognition. Psychology Press, New York
Shea Charles H et al (2000) Spacing practice sessions across days benefits the learning of motor skills. Hum Mov Sci 19(5):737–760
Lee Timothy D, Genovese Elizabeth D (1988) Distribution of practice in motor skill acquisition: learning and performance effects reconsidered. Res Q Exerc Sport 59(4):277–287
Donovan John J, Radosevich David J (1999) A meta-analytic review of the distribution of practice effect: now you see it, now you don’t. J Appl Psychol 84(5):795
Moulton C-AE et al (2006) Teaching surgical skills: what kind of practice makes perfect?: a randomized, controlled trial. Ann Surg 244:400
Gallagher Anthony G, Jordan-Black Julie Anne, O’Sullivan Gerald C (2012) Prospective, randomized assessment of the acquisition, maintenance, and loss of laparoscopic skills. Ann Surg 256(2):387–393
Kolkman Wendela et al (2008) Laparoscopic skills simulator: construct validity and establishment of performance standards for residency training. Gynecol Surg 5(2):109–114
Seijts GH, Latham GP (2006) Learning goals or performance goals: is it the journey or the destination? Ivey Bus J 70:1–6
Dweck Carol (2006) Mindset: the new psychology of success. Random House Digital, Inc., New York
Strandbygaard Jeanett et al (2013) Instructor feedback versus no instructor feedback on performance in a laparoscopic virtual reality simulator: a randomized trial. Ann Surg 257(5):839–844
Gallagher Anthony G, O’Sullivan Gerald C (2012) Fundamentals of surgical simulation. Springer, London GC
van der Linden D (2011) The urge to stop: the cognitive and biological nature of acute mental fatigue. In: Ackerman PL (ed) Cognitive fatigue: multidisciplinary perspectives on current research and future applications. American Psychological Association, Washington, DC
Kahol Kanav et al (2008) Effect of fatigue on psychomotor and cognitive skills. Am J Surg 195(2):195–204
Bjork RA (1999) Assessing our own competence: heuristics and illusions. In: Gopher D, Koriat A (eds) Attention and performance XVII: cognitive regulation of performance: interaction of theory and application. Attention and performance
Stickgold Robert (2005) Sleep-dependent memory consolidation. Nature 437(7063):1272–1278
Brashers-Krug Thomas, Shadmehr Reza, Bizzi Emilio (1996) Consolidation in human motor memory. Nature 382(6588):252–255
Korman Maria et al (2007) Daytime sleep condenses the time course of motor memory consolidation. Nat Neurosci 10(9):1206–1213
Batson Glenna (2007) Revisiting overuse injuries in dance in view of motor learning and somatic models of distributed practice. J Dance Med Sci 11(3):70–75
Loehr Jim, Schwartz Tony (2003) The power of full engagement: managing energy, not time, is the key to high performance and personal renewal. Simon & Schuster, Inc., New York
Acknowledgments
We would like to acknowledge Gertjan Hultzer, Rene Rodenburg, and Tom Hulscher for their assistance in the LUMC skillslab. This work was funded by Leiden University Medical Centre (LUMC).
Disclosure
Edward N. Spruit MSc., Dr. Guido P. H. Band, & Prof. Jaap F. Hamming have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Spruit, E.N., Band, G.P.H. & Hamming, J.F. Increasing efficiency of surgical training: effects of spacing practice on skill acquisition and retention in laparoscopy training. Surg Endosc 29, 2235–2243 (2015). https://doi.org/10.1007/s00464-014-3931-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-014-3931-x