Abstract
Staphylococcus aureus is one of the most important causes of nosocomial infections. An effective vaccine to prevent S. aureus infections is urgently required due to the dramatic increase in the number of antibiotic-resistant strains. In this report, we evaluated a newly recombinant protein composed of selected antigenic regions of clumping factor A (ClfA), iron surface determinant B (IsdB) and gamma hemolysin B (HlgB) of S. aureus and sequence coding for hydrophobic linkers between three domains. The recombinant gene was constructed in pET-28a (+) and expressed in Escherichia coli BL21. In addition, sequence coding for a His6-tag was added followed by a hybrid procedure of nickel chelate protein purification. Immunization of BALB/c mice with the recombinant protein ClfA–IsdB–Hlg evoked antigen-specific antibodies that could opsonize S. aureus cells, enhancing in vitro phagocytosis by macrophages. Vaccination with the recombinant protein also reduced the bacterial load recovered from mice spleen samples and increased survival following the intraperitoneal challenge with pathogenic S. aureus compared to the control mice. Our results showed that the recombinant protein ClfA–IsdB–Hlg is a promising vaccine candidate for the prevention of S. aureus bacteremia infections.
Similar content being viewed by others
Introduction
Staphylococcus aureus bacteria are a potential pathogen that can cause numerous infections in humans ranging from moderate skin infections to systemic infections, including bacteremia, osteomyelitis and septic shock. This opportunistic pathogen is one of the most important causes of both nosocomial and community-acquired infections [1, 2]. In the last two decades, there has been a significant increase in the incidence of nosocomial infections associated with S. aureus [3]. It is becoming increasingly difficult to treat these severe infections because of the emergence of strains resistant to antibiotics, particularly methicillin and vancomycin [4, 5]. Due to the dramatic increase in the number of nosocomial staphylococcal infections, including antibiotic-resistant S. aureus, there is an urgent need for the development of alternative treatment approaches particularly in the field of vaccines and therapeutic antibodies. The main challenge for designing an effective vaccine against S. aureus is that this organism can produce several potential virulence factors. This challenge can potentially be overcome using multi-component vaccines [6]. Several S. aureus virulence factors have been investigated over the past decade. Proteins selected as vaccine candidates must be expressed by the majority of clinical S. aureus strains, perform important functions during infection and produce immune response that promotes opsonophagocytic activity [7]. Clumping factor A (ClfA), iron surface determinant B (IsdB) and gamma hemolysin (Hlg) all have such features. ClfA is a fibrinogen-binding surface protein of S. aureus, which can cause clumping of bacteria in suspension [8]. This interaction between ClfA and fibrinogen is very important for bacterial virulence, and almost all S. aureus strains can express the clfA gene [9]. ClfA is also an excellent target for immunological attack by antibodies [10]. The fibrinogen-binding activity of ClfA is related to the N-terminal A region of this protein [11]. Iron surface determinant B (IsdB) is another component under clinical development for multi-subunit vaccine, which has shown protective efficacy in animal models [12, 13]. IsdB protein of S. aureus is known as iron-sequestering protein in iron-limited condition [14]. The gene isdB is conserved in diverse S. aureus clinical isolates [7], and loss of this protein leads to a reduction in virulence, which makes it a suitable candidate in vaccine projects [13]. Evaluation of binding regions confirmed that amino acid residues 130–454 of the IsdB protein are required for bindings in monoclonal antibodies that bind to this portion effectively [15]. Another candidate component for developing multi-subunit vaccine against S. aureus is gamma hemolysin (Hlg). Hlg protein is a two-component toxin, which plays an important role in the disruption and lysis of erythrocytes and leukocytes [16]. More than 99 % of S. aureus strains are capable of producing this protein [17]. IgG antibody production against gamma hemolysin B (HlgB) was higher in S. aureus-infected patients than in control groups [18]. In this report, we have prepared a recombinant vaccine using antigenic regions of ClfA, IsdB and HlgB proteins to evaluate their immunogenicity in a mouse model. The clinical application of the developed know-how is subject to further studies; however, the identified vaccine targets may have the potential to generate a significant level of functional antibodies in patients with a high risk of developing S. aureus infections.
Materials and methods
Bacterial strains
Escherichia coli BL21 (DE3) (Novagen, USA) was used as an expression host. A clinical isolate of S. aureus was applied for immunization assay, opsonophagocytic activity and bacteremia challenge. This strain was isolated from blood cultures, and the presence of three genes clfA, isdB and hlg was confirmed by PCR.
Bioinformatic analysis of recombinant protein
To design a recombinant protein, antigenic epitope regions of ClfA, IsdB and HlgB proteins were selected and fused together by hydrophobic linkers to separate these three domains from each other. The secondary and tertiary structures of the recombinant protein prediction were performed by GOR secondary structure prediction server and I-TASSER ab initio online software, and its stability was analyzed by mfold software (www.bioinfo.rpi.edu/applications/mfold) [19–21]. A VaxiJen server was used to predict the immunogenicity of the recombinant protein (www.jenner.ac.uk/VaxiJen) [22]. The amino acid sequence of the recombinant protein was analyzed using the software based on B cell epitope prediction algorithms to predict continuous (http://www.imtech.res.in/raghava/bcepred/) and discontinuous B cell epitopes (http://www.cbs.dtu.dk/services/DiscoTope) [23, 24]. The recombinant gene was designed to be inserted between the BamHI and HindIII sites of pET-28a (+) vector, and a 6His-encoding sequence was added at the 3′ end of the recombinant gene sequence. The recombinant gene was synthesized by Shine Gene Molecular Biotech, Inc (Shanghai, China). The nucleotide sequence of the clfA–isdB–hlg recombinant gene was submitted and published in DDBJ (Accession number: KF515219.1).
Expression of recombinant protein
The recombinant pET-28a–clfA–isdB–hlg was initially transferred into E. coli BL21 (DE3). An overnight culture of recombinant E. coli BL21 (DE3) in 5 ml LB broth (containing 30 µg/mL of kanamycin; Sigma, Germany) was used to inoculate a fresh LB broth. New culture media were incubated at 37 °C while shaking; when the OD600 reached 1.0, expression was induced by 1 mM of isopropylthio-β-d-galactoside (IPTG). After overnight induction, cells were harvested by centrifugation and pellets were suspended in PBS. Cells were destroyed using ultrasonication for 5 min, three times with a 0.5-s cycle frequency of 70 % on ice. The bacterial lysates was centrifuged, and the soluble and solid phases were separated; solid materials were dissolved in 8 M urea. Both soluble supernatant and insoluble protein were analyzed by SDS-PAGE for the presence of recombinant proteins.
Purification of recombinant protein
The His6-tagged recombinant protein was purified by nickel chelate chromatography according to the previously described hybrid procedure [25]. Briefly, the cell pellet was dissolved in a lysis buffer, debris was removed, and urea-dissolved cell components were subjected to Ni–NTA resin (Qiagen, USA). Urea was removed by using washing buffers with decreasing urea concentrations (8, 6, 4, 2, 1, 0 M urea). Finally, the recombinant protein was eluted from the column using 250 mM imidazole solution. Imidazole was removed by dialysis against 100 volume of PBS (pH 7.2) for 24 h with three exchanges [25]. Purified protein was analyzed by SDS-PAGE and quantified with NanoDrop®, and it stored at −80 °C.
Western blot
Western blot analysis was performed as described previously [25]. Briefly, proteins were separated on a 10 % polyacrylamide gel and then were transferred into a polyvinylidene difluoride (PVDF) membrane (Roche, Germany) by a semi-dry blotting unit (Bio-Rad, USA). The PVDF membrane was blocked with 3 % BSA, in PBST (PBS containing 0.05 % Tween 20) for 2 h, at room temperature and washed three times with PBST. Proteins were traced by incubating with 1:1000 dilutions of mouse HRP-conjugated anti-His-tag antibody (Roche, Germany) in PBST for 2 h, at room temperature. Finally, the membrane was washed as described above and was developed using a DAB substrate solution (3,3′-diaminobenzidine tetrahydrochloride, Sigma).
Preparation of formalin-inactivated S. aureus
S. aureus clinical isolate was grown in brain-heart infusion (BHI) broth at 37 °C for 24 h. Bacterial cells were diluted 1:200 in fresh BHI broth and then cultured at 37 °C for 24 h. To prepare inactivated suspensions, bacterial cells were harvested by centrifugation (10,000×g for 10 min), washed three times with PBS and suspended in PBS. For formalin inactivation, bacterial cells were suspended in 1 % formaldehyde in PBS and incubated at 4 °C for 24 h with shaking. Bacterial cells were then centrifuged, washed three times and suspended in PBS. The concentration of bacterial cells was set at 108 CFU/mL using spectrophotometric method. The suspension was checked for complete inactivation through streaking onto blood agar plates.
Immunization of mice
Female BALB/c mice, 6–8 weeks of age, were bought from the laboratory animal production center of Pasture Institute of Iran (Tehran, Iran) and kept under pathogen-free conditions. Mice (n = 14) were assigned into three groups (1, 2 and 3), and each group was vaccinated three times. Vaccination was performed with 200 µL of the emulsion containing purified recombinant protein (10 µg) emulsified 1:1 with complete Freund’s adjuvant and 200 µL of the emulsion containing formalin-inactivated S. aureus (108 CFU/mL) emulsified 1:1 with complete Freund’s adjuvant administered subcutaneously on days 0 for group 1 and 2, respectively. Booster immunizations were performed on days 14 and 28 for both groups (emulsified 1:1 with incomplete Freund’s adjuvant). The control group 3 inoculated with PBS followed the same protocol.
IgG assessment
One week after the each immunization dose, blood samples were drawn by retro-orbital bleeding and serum samples were stored at −80 °C separately. ELISA method was used for the measurement of total IgG and its subtypes [25]. Ninety-six-well microtiter plates were coated with 5 µg/mL recombinant protein overnight at 4 °C, and then blocked for 2 h, at 37 °C, with 1 % BSA. Plates were washed three times and incubated with diluted sera in PBS −1 % BSA, for 2 h, at 37 °C. The wells were washed again and incubated stepwise with a HRP-conjugated goat anti-mouse IgG antibody diluted 1:4000, TMB solution as a substrate and 2NH2SO4. Finally, OD450 was measured using a microplate reader. ELISA plates coated with 107 CFU/mL, of S. aureus clinical strain, also were used to evaluate the humoral response induced in formalin-inactivated S. aureus immunized mice.
Opsonophagocytic activity
Opsonophagocytic activity assay (OPK) was performed based on previously published protocols [26, 27]. Macrophages from peritoneal cavity of naive mice were collected by injection of cold RPMI medium supplemented with 10 % FBS. Peritoneal macrophages were counted, diluted to 2 × 106 macrophages per mL, and seeded (200 µL) into each well of a 24-well plate. Five hundred microliters of cell culture medium was added to each well, and then plates were incubated at 37 °C, for 24 h. Afterward, each well was replaced by 500 µL of a new antibiotic-free medium and then was incubated at 37 °C, for 24 h. For the OPK assay, 200 µL of a clinical S. aureus isolate with an approximate concentration of 2 × 107 CFU per mL, was opsonized for 30 min, at 37 °C, with equal volume of complement source (the baby rabbit complement; Razi Institute of Vaccine Research and Production, Karaj, Iran) and equal volume of heat-treated sera (at 56 °C for 30 min) of three groups separately. Five hundred microliters of serum containing the complement and opsonized staphylococcus was added to macrophages. After 50-min incubation at 25 °C, all macrophages were washed three times by distilled water. The macrophage was lysed by saline for 20 min, and bacterial cells from each well were counted on 5 % blood agar plates via plating serial dilutions.
Lethal challenge
Ten days after final immunization, mice were challenged intraperitoneally by 2 × 109 CFU of a clinical S. aureus isolate (containing clfA, isdB and hlg genes) to induce bacteremia. After 5 days, three mice of each group were killed; their kidneys and spleens were removed and homogenized in PBS, and the bacterial load of each sample was counted on BHI and blood agar. The remaining mice were followed until day seven post-challenge for survival analysis.
Statistical analysis
Data were analyzed by IBM SPSS 22.0 via one-way analysis of variance (ANOVA) and post hoc test (LSD). Fisher’s exact test was used to analyze the statistical significance of the survival data. All the data of this study are expressed as mean ± SD, and differences between groups with p values ≤0.05 were considered significant.
Result
Bioinformatics
The recombinant gene length was 1431 bp and was composed of residues 500–559 of the region A of clumping factor A, amino acid residues 130–454 of the IsdB protein and the first 50 amino acid residues after the Hlg protein of signal peptide. In order to separate the different domains, linkers consisting of EAAAKEAAAKEAAAK repeats and DPRVPSS repeats were designed. A schematic diagram of protein domain structures with the design of linker sites is shown in Fig. 1a. The complete sequence of the recombinant protein is shown in Fig. 1b. The data from mRNA prediction showed that the mRNA was stable enough for efficient translation in the host. VaxiJen analysis of the protein showed high antigenicity. Continuous and discontinuous B cell epitopes were identified (data not shown). In general, the results confirmed that proteins encoded by these genes are valid candidates for designing vaccines against S. aureus infections.
Expression and purification of recombinant protein
The majority of expressed proteins were detected in inclusion bodies after the recombinant pET-28a (+) was induced with 1 mM IPTG and an overnight induction period at 37 °C. SDS-PAGE analysis showed a 58-KDa protein present in inclusion body fraction (data not shown). The recombinant protein was successfully purified (Fig. 2) with a yield of approximately 2 mg of purified recombinant protein from one liter of culture. Western blot analysis also confirmed the purified protein with His6-tag residue (Fig. 3).
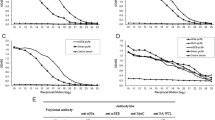
Humoral immune response to recombinant protein in mice
Specific IgG titer directed to the recombinant protein was measured after three doses of immunization. IgG titer against the recombinant protein reached a maximum level at the third immunization (Fig. 4a). Comparison of IgG titer between the three groups revealed that after the third immunization, the antibody titers in the recombinant protein group were higher than those in either the formalin-inactivated S. aureus group or the control group (Fig. 4b). These results were statistically significant (p ≤ 0.05). The serum levels of IgG1, IgG2a, IgG2b and IgG3 directed against the recombinant protein were measured (Fig. 4c). IgG1, IgG2a, IgG2b and IgG3 titers in the recombinant protein group showed a significant increase as compared to control group (p ≤ 0.05), and IgG1 subtype was predominant.
a IgG antibody titers against the recombinant protein determined by ELISA. The mice (n = 14) were immunized three times (0, 14, 28 days), and sera were obtained from the mice 1 week after the second and the third vaccination. b Comparison of IgG titers between three groups: recombinant protein group, inactivated S. aureus and control group after the third immunization. c Measurement of serum levels of IgG1, IgG2a, IgG2b and IgG3 against the recombinant protein and control groups. Values represent the means ± the SEM
Bioactivity of all sera from each in vitro group was examined by the impact of specific antibodies on phagocytosis activity of peritoneal macrophages. A clinical S. aureus isolate (containing clfA, isdB and hlg genes) was used for this purpose. Bacterial cells were opsonized with serum from mice under experiment. After exposing the opsonized bacteria to the peritoneal macrophages, the phagocytic capacity of macrophages exposed with serum from mice immunized with recombinant protein showed a significant increase as compared to macrophages exposed to groups 2 and 3 (p = 0.043 and p = 0.002, respectively). Furthermore, the phagocytic capacity of macrophages exposed to serum from mice immunized with formalin-inactivated S. aureus showed a significant increase as compared to macrophages exposed with group 3 (p = 0.041) (Fig. 5).
Number of in vitro ingested staphylococci after phagocytosis assay with serum from mice immunized with recombinant protein, serum from mice immunized with formalin-inactivated S. aureus and serum from mice immunized with PBS. Error bars represent the SEM. All of the p values provided represent comparison between sera from control group and from formalin-inactivated S. aureus or recombinant protein vaccinated groups
Bacterial challenge
To determine whether the recombinant protein could elicit protective immunity and reduce the bacteremia rate in mice, 10 days after the second booster, mice were challenged intraperitoneally with 2 × 109 CFU of the same clinical S. aureus strain, which was used for immunization, and there was a significant (p = 0.004) reduction in CFU recovered from spleen samples in mice immunized with the recombinant protein as compared to non-immunized mice (Fig. 6). However, this result was not significant for kidney samples (p = 0/1). All animals were monitored for 7 days post-challenge to study mortality. While 64.2 % of mice, which were vaccinated with the recombinant protein, survived after 7 days, the survival rate of mice in groups 2 and 3 was only 42.8 and 35.7 %, respectively (Fig. 7). Survival analysis showed a significant (p = 0.04) increase in survival rate of mice receiving the recombinant protein as compared to mice receiving PBS.
Protection against bacterial dissemination in bacteremia model. Bacterial burden in kidneys and spleen in three mice of each group was determined after intraperitoneal injection with 2 × 109 CFU of S. aureus per mouse. There was a significant reduction in CFU recovered from spleen in mice immunized with the recombinant protein as compared to non-immunized mice. p values were recorded
Protection against lethal challenge infections. After determination of lethal dose, the mice (n = 14) were challenged by intraperitoneal injection with clinical S. aureus isolates (2 × 109 CFU) and monitored for 7 days for survival. Survival analysis showed a significant (p = 0.04) increase in survival rate of mice receiving the recombinant protein as compared to mice receiving PBS
Discussion
Over the past decade, increasing levels of resistance to antimicrobial components of S. aureus have become a major challenge for health care. There are currently no vaccines available for S. aureus infections [4, 28, 29]; therefore, an effective vaccine to prevent S. aureus infections is urgently required [30]. The main problem for designing an effective vaccine against S. aureus is that these bacteria can express several potential virulence factors. Using multi-component vaccines is a way to address this issue [6, 31]. In this study, we designed a new multi-component vaccine against S. aureus bacteremia infection by combining the antigenic regions of three important virulence factors of S. aureus (ClfA, IsdB and Hlg) that are expressed by most clinical isolates of S. aurous. We choose ClfA, IsdB and Hlg proteins, because it was shown in previous attempts that these three virulence factors can produce an immune response that promotes opsonophagocytic activity [1, 10, 13, 18, 32, 33]. Ebert et al. [34] showed that a humanized monoclonal antibody targeting IsdB can protect mice in a murine sepsis model, reduce bacteremia and prevent central venous catheter colonization in a rat model. Josefsson et al. [35], in their preclinical studies, had showed that antibodies against ClfA have the potential to protect from infection. Other investigations have also confirmed that ClfA is an important virulence factor and elicited antibodies against this protein can completely prevent S. aureus binding to fibrinogen, which is required to inhibit ClfA-mediated pathology [36]. IgG levels against gamma hemolysin B (HlgB) were higher in S. aureus-infected patients than in control subjects [18]. To find successful S. aureus candidate vaccines, we considered major virulence mechanisms associated with staphylococcal disease including binding to host cells (ClfA), nutrient acquisition or scavenging nutrients (IsdB) and promoting tissue damage (Hlg). We selected the antigenic region for each protein and generated antibodies against these regions. By combining several bioinformatics approaches, it was shown that synthetic multi-component vaccine structure had desirable protein stability and could successfully induce B cell-mediated immune response. According to bioinformatics predictions, the recombinant protein can be a suitable immunogen. Furthermore, our results indicated reasonable immunogenicity for the recombinant protein in a mice model. We confirmed that clfA–isdB–hlg gene synthesis takes place directly in the expression vector pET-28a. This is a rapid, easy and cost-effective method for the preparation of the recombinant protein. The yield of recombinant protein ClfA–IsdB–Hlg was more than 70–80 % of the total bacterial proteins, which suggests the process may have the potential to be scaled up for industrial production. Our efforts for removal of urea by dialysis were not fruitful. Therefore, for better refold and elimination of urea, we used a series of washing solutions with decreasing urea concentrations when the recombinant protein was bound to Ni–NTA resins. This method was superior compared to other methods used for purification of recombinant proteins.
S. aureus infections are believed to stimulate a strong humoral immune responses characterized by higher IgG titers, dominance by the IgG1 subtype and the enhanced ability of induced antibodies to bind and opsonize the bacteria, as well as to inhibit bacterial growth [37]. In the present study, immunization of mice with the recombinant protein ClfA–IsdB–Hlg revealed that the protein induced a significant level of IgG antibodies in a mice model and we had the highest antibody titers approximately after the third vaccination. Furthermore, analysis of the IgG responses revealed that immunization with recombinant vaccine produced higher levels of IgG than immunization with inactivated S. aureus or the control group. We did not evaluate ClfA, IsdB and Hlg alone, because each of these proteins showed immunogenicity roles in previous studies. Further experiments to determine isotypes of IgG showed that IgG subtype induced by recombinant protein was predominantly IgG1. This represents a Th2-dominant response. The induction of a higher proportion of IgG1 is a typical feature of protein immunization [38]. In addition, antibodies against the recombinant protein group were more potent in increasing the ingestion of bacteria by peritoneal macrophage compared to the formalin-inactivated S. aureus or control groups. These results confirm that antibodies against the recombinant protein ClfA–IsdB–Hlg promote the phagocytosis of S. aureus and enhance the clearance of the in vivo pathogen. Opsonic activity plays an important role in successful vaccine development against S. aureus infection.
The aim of the present study was to examine the protective efficacy of recombinant protein ClfA-IsdB-Hlg in mouse bacteremia model, because bacteremia caused by S. aureus is an important infection and the morbidity and mortality of both community-acquired and healthcare-associated bacteremia is high [39, 40]. In our bacterial challenge results, a significant reduction in the bacteria recovered from spleen samples was demonstrated in mice immunized with the recombinant protein ClfA–IsdB–Hlg compared with the control group (p < 0/05). Immunization with the recombinant protein ClfA–IsdB–Hlg also decreased the mortality rate in immunized mice compared to mice in the control groups.
Conclusion
Overall, our findings indicate that the recombinant protein ClfA–IsdB–Hlg induces a significantly stronger and more effective immune response than the formalin-inactivated S. aureus in mouse bacteremia model. To confirm the protection efficiency of the recombinant protein ClfA–IsdB–Hlg, we suggest examining the other challenge strain, infection site, and immunization routes and doses. The recombinant protein ClfA–IsdB–Hlg is currently being further investigated in our laboratory as a novel promising multi-component candidate vaccine that can protect humans at high risk of S. aureus infection, such as dialysis patients, those who undergoing surgery, those who suffering from chronic illnesses and those who experiencing prolonged hospitalization.
References
Archer GL (1998) Staphylococcus aureus: a well-armed pathogen. Clin Infect Dis 26(5):1179–1181
Lowy FD (1998) Staphylococcus aureus infections. N Engl J Med 339(8):520–532. doi:10.1056/NEJM199808203390806
Wertheim HF, Vos MC, Ott A, Voss A, Kluytmans JA, Vandenbroucke-Grauls CM, Meester MH, van Keulen PH, Verbrugh HA (2004) Mupirocin prophylaxis against nosocomial Staphylococcus aureus infections in nonsurgical patients: a randomized study. Ann Intern Med 140(6):419–425
David MZ, Daum RS (2010) Community-associated methicillin-resistant Staphylococcus aureus: epidemiology and clinical consequences of an emerging epidemic. Clin Microbiol Rev 23(3):616–687. doi:10.1128/CMR.00081-09
Klein E, Smith DL, Laxminarayan R (2007) Hospitalizations and deaths caused by methicillin-resistant Staphylococcus aureus, United States, 1999–2005. Emerg Infect Dis 13(12):1840–1846. doi:10.3201/eid1312.070629
Spellberg B, Daum R (2012) Development of a vaccine against Staphylococcus aureus. Semin Immunopathol 34(2):335–348. doi:10.1007/s00281-011-0293-5
Schaffer AC, Lee JC (2008) Vaccination and passive immunisation against Staphylococcus aureus. Int J Antimicrob Agents 32(Suppl 1):S71–S78. doi:10.1016/j.ijantimicag.2008.06.009
Peacock SJ, Moore CE, Justice A, Kantzanou M, Story L, Mackie K, O’Neill G, Day NP (2002) Virulent combinations of adhesin and toxin genes in natural populations of Staphylococcus aureus. Infect Immun 70(9):4987–4996
Josefsson E, Higgins J, Foster TJ, Tarkowski A (2008) Fibrinogen binding sites P336 and Y338 of clumping factor A are crucial for Staphylococcus aureus virulence. PLoS One 3(5):e2206. doi:10.1371/journal.pone.0002206
Hall AE, Domanski PJ, Patel PR, Vernachio JH, Syribeys PJ, Gorovits EL, Johnson MA, Ross JM, Hutchins JT, Patti JM (2003) Characterization of a protective monoclonal antibody recognizing Staphylococcus aureus MSCRAMM protein clumping factor A. Infect Immun 71(12):6864–6870
Hartford OM, Wann ER, Hook M, Foster TJ (2001) Identification of residues in the Staphylococcus aureus fibrinogen-binding MSCRAMM clumping factor A (ClfA) that are important for ligand binding. J Biol Chem 276(4):2466–2473. doi:10.1074/jbc.M007979200
Pozzi C, Wilk K, Lee JC, Gening M, Nifantiev N, Pier GB (2012) Opsonic and protective properties of antibodies raised to conjugate vaccines targeting six Staphylococcus aureus antigens. PLoS One 7(10):e46648. doi:10.1371/journal.pone.0046648
Kuklin NA, Clark DJ, Secore S, Cook J, Cope LD, McNeely T, Noble L, Brown MJ, Zorman JK, Wang XM, Pancari G, Fan H, Isett K, Burgess B, Bryan J, Brownlow M, George H, Meinz M, Liddell ME, Kelly R, Schultz L, Montgomery D, Onishi J, Losada M, Martin M, Ebert T, Tan CY, Schofield TL, Nagy E, Meineke A, Joyce JG, Kurtz MB, Caulfield MJ, Jansen KU, McClements W, Anderson AS (2006) A novel Staphylococcus aureus vaccine: iron surface determinant B induces rapid antibody responses in rhesus macaques and specific increased survival in a murine S. aureus sepsis model. Infect Immun 74(4):2215–2223. doi:10.1128/IAI.74.4.2215-2223.2006
Mazmanian SK, Skaar EP, Gaspar AH, Humayun M, Gornicki P, Jelenska J, Joachmiak A, Missiakas DM, Schneewind O (2003) Passage of heme-iron across the envelope of Staphylococcus aureus. Science 299(5608):906–909. doi:10.1126/science.1081147
Brown M, Kowalski R, Zorman J, Wang XM, Towne V, Zhao Q, Secore S, Finnefrock AC, Ebert T, Pancari G, Isett K, Zhang Y, Anderson AS, Montgomery D, Cope L, McNeely T (2009) Selection and characterization of murine monoclonal antibodies to Staphylococcus aureus iron-regulated surface determinant B with functional activity in vitro and in vivo. Clin Vaccine Immunol 16(8):1095–1104. doi:10.1128/CVI.00085-09
Gouaux E, Hobaugh M, Song L (1997) alpha-Hemolysin, gamma-hemolysin, and leukocidin from Staphylococcus aureus: distant in sequence but similar in structure. Protein Sci 6(12):2631–2635. doi:10.1002/pro.5560061216
Prevost G, Cribier B, Couppie P, Petiau P, Supersac G, Finck-Barbancon V, Monteil H, Piemont Y (1995) Panton-Valentine leucocidin and gamma-hemolysin from Staphylococcus aureus ATCC 49775 are encoded by distinct genetic loci and have different biological activities. Infect Immun 63(10):4121–4129
Verkaik NJ, Dauwalder O, Antri K, Boubekri I, de Vogel CP, Badiou C, Bes M, Vandenesch F, Tazir M, Hooijkaas H, Verbrugh HA, van Belkum A, Etienne J, Lina G, Ramdani-Bouguessa N, van Wamel WJ (2010) Immunogenicity of toxins during Staphylococcus aureus infection. Clin Infect Dis 50(1):61–68. doi:10.1086/648673
Sen TZ, Jernigan RL, Garnier J, Kloczkowski A (2005) GOR V server for protein secondary structure prediction. Bioinformatics 21(11):2787–2788. doi:10.1093/bioinformatics/bti408
Zhang Y (2008) I-TASSER server for protein 3D structure prediction. BMC Bioinform 9:40. doi:10.1186/1471-2105-9-40
Zuker M (2003) Mfold web server for nucleic acid folding and hybridization prediction. Nucleic Acids Res 31(13):3406–3415
Doytchinova IA, Flower DR (2007) VaxiJen: a server for prediction of protective antigens, tumour antigens and subunit vaccines. BMC Bioinform 8:4. doi:10.1186/1471-2105-8-4
El-Manzalawy Y, Dobbs D, Honavar V (2008) Predicting flexible length linear B-cell epitopes. Comput Syst Bioinform Life Sci Soc Comput Syst Bioinform Conf 7:121–132
Kringelum JV, Lundegaard C, Lund O, Nielsen M (2012) Reliable B cell epitope predictions: impacts of method development and improved benchmarking. PLoS Comput Biol 8(12):e1002829. doi:10.1371/journal.pcbi.1002829
Aghababa H, Mohabati Mobarez A, Khoramabadi N, Behmanesh M, Mahdavi M, Tebianian M, Nejati M (2014) A comparative approach to strategies for cloning, expression, and purification of Mycobacterium tuberculosis mycolyl transferase 85B and evaluation of immune responses in BALB/c mice. Mol Biotechnol 56(6):487–497. doi:10.1007/s12033-013-9696-y
Nilsson IM, Patti JM, Bremell T, Hook M, Tarkowski A (1998) Vaccination with a recombinant fragment of collagen adhesin provides protection against Staphylococcus aureus-mediated septic death. J Clin Investig 101(12):2640–2649. doi:10.1172/JCI1823
Swanson RN, O’Brien AD (1983) Genetic control of the innate resistance of mice to Salmonella typhimurium: Ity gene is expressed in vivo by 24 hours after infection. J Immunol 131(6):3014–3020
Sydnor ER, Perl TM (2011) Hospital epidemiology and infection control in acute-care settings. Clin Microbiol Rev 24(1):141–173. doi:10.1128/CMR.00027-10
Anderson AS, Scully IL, Timofeyeva Y, Murphy E, McNeil LK, Mininni T, Nunez L, Carriere M, Singer C, Dilts DA, Jansen KU (2012) Staphylococcus aureus manganese transport protein C is a highly conserved cell surface protein that elicits protective immunity against S. aureus and Staphylococcus epidermidis. J Infect Dis 205(11):1688–1696. doi:10.1093/infdis/jis272
Schaffer AC, Lee JC (2009) Staphylococcal vaccines and immunotherapies. Infect Dis Clin North Am 23(1):153–171. doi:10.1016/j.idc.2008.10.005
Arrecubieta C, Matsunaga I, Asai T, Naka Y, Deng MC, Lowy FD (2008) Vaccination with clumping factor A and fibronectin binding protein A to prevent Staphylococcus aureus infection of an aortic patch in mice. J Infect Dis 198(4):571–575. doi:10.1086/590210
Kim HK, DeDent A, Cheng AG, McAdow M, Bagnoli F, Missiakas DM, Schneewind O (2010) IsdA and IsdB antibodies protect mice against Staphylococcus aureus abscess formation and lethal challenge. Vaccine 28(38):6382–6392. doi:10.1016/j.vaccine.2010.02.097
Etz H, Minh DB, Henics T, Dryla A, Winkler B, Triska C, Boyd AP, Sollner J, Schmidt W, von Ahsen U, Buschle M, Gill SR, Kolonay J, Khalak H, Fraser CM, von Gabain A, Nagy E, Meinke A (2002) Identification of in vivo expressed vaccine candidate antigens from Staphylococcus aureus. Proc Natl Acad Sci USA 99(10):6573–6578. doi:10.1073/pnas.092569199
Ebert T, Smith S, Pancari G, Clark D, Hampton R, Secore S, Towne V, Fan H, Wang XM, Wu X, Ernst R, Harvey BR, Finnefrock AC, Wang F, Tan C, Durr E, Cope L, Anderson A, An Z, McNeely T (2010) A fully human monoclonal antibody to Staphylococcus aureus iron regulated surface determinant B (IsdB) with functional activity in vitro and in vivo. Human Antib 19(4):113–128. doi:10.3233/HAB-2010-0235
Josefsson E, Hartford O, O’Brien L, Patti JM, Foster T (2001) Protection against experimental Staphylococcus aureus arthritis by vaccination with clumping factor A, a novel virulence determinant. J Infect Dis 184(12):1572–1580. doi:10.1086/324430
Anderson AS, Miller AA, Donald RG, Scully IL, Nanra JS, Cooper D, Jansen KU (2012) Development of a multicomponent Staphylococcus aureus vaccine designed to counter multiple bacterial virulence factors. Hum Vaccine Immunother 8(11):1585–1594. doi:10.4161/hv.21872
Gong R, Hu C, Xu H, Guo A, Chen H, Zhang G, Shi L (2010) Evaluation of clumping factor A binding region A in a subunit vaccine against Staphylococcus aureus-induced mastitis in mice. Clin Vaccine Immunol 17(11):1746–1752. doi:10.1128/CVI.00162-10
Kawano Y, Fukuda J, Nasu K, Nishida M, Narahara H, Miyakawa I (2004) Production of macrophage inflammatory protein-3α in human follicular fluid and cultured granulosa cells. Fertil Steril 82(Suppl 3):1206–1211. doi:10.1016/j.fertnstert.2004.05.070
Naber CK (2009) Staphylococcus aureus bacteremia: epidemiology, pathophysiology, and management strategies. Clin Infect Dis 48(Suppl 4):S231–S237. doi:10.1086/598189
van Hal SJ, Jensen SO, Vaska VL, Espedido BA, Paterson DL, Gosbell IB (2012) Predictors of mortality in Staphylococcus aureus bacteremia. Clin Microbiol Rev 25(2):362–386. doi:10.1128/CMR.05022-11
Acknowledgments
This research has been supported by Tehran University of Medical Sciences and Health Services Grant 13942/90-02-30.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Delfani, S., Mohabati Mobarez, A., Imani Fooladi, A. et al. Protection of mice against Staphylococcus aureus infection by a recombinant protein ClfA–IsdB–Hlg as a vaccine candidate. Med Microbiol Immunol 205, 47–55 (2016). https://doi.org/10.1007/s00430-015-0425-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00430-015-0425-y