Abstract
Objectives
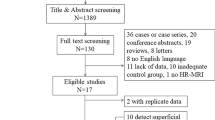
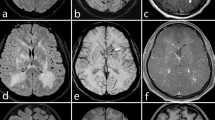
To assess the detectability of vasculitic changes of the superficial cranial arteries with contrast-enhanced 7 T MRI in three patients with GCA and intraindividual comparison with 3 T MRI.
Methods
Three patients (two female, one male) with suspected GCA underwent contrast-enhanced T1-weighted high-resolution MRI at 3 T and 7 T magnetic field strength. The clinical diagnosis, based on criteria of the American College of Rheumatology, was confirmed by biopsy of the superficial temporal artery after MRI. MR images were visually assessed for detection of vasculitic mural contrast enhancement and vessel wall thickening of the superficial cranial arteries.
Results
Both 3 T and 7 T MRI allows for visualisation of mural inflammatory changes and assessment of the vasculitic involvement pattern. Image quality of 7 T MRI was rated superior to image quality of 3 T MRI scans.
Conclusions
7 T MR imaging of vasculitic changes in patients with GCA is possible, and suggests superior image quality. Larger patient studies are necessary to quantify the diagnostic advantages of 7 T MRI.



Similar content being viewed by others
References
Salvarani C, Cantini F, Hunder GG (2008) Polymyalgia rheumatica and giant-cell arteritis. Lancet 372:234–245
Hunder GG, Bloch DA, Michel BA et al (1990) The American College of Rheumatology 1990 criteria for the classification of giant cell arteritis. Arthritis Rheum 33:1122–1128
Hayreh SS, Podhajsky PA, Raman R, Zimmerman B (1997) Giant cell arteritis: validity and reliability of various diagnostic criteria. Am J Ophthalmol 123:285–296
Bley TA, Uhl M, Carew J et al (2007) Diagnostic value of high-resolution MR imaging in giant cell arteritis. AJNR Am J Neuroradiol 28:1722–1727
Klein RG, Campbell RJ, Hunder GG, Carney JA (1976) Skip lesions in temporal arteritis. Mayo Clin Proc 51:504–510
Taylor-Gjevre R, Vo M, Shukla D, Resch L (2005) Temporal artery biopsy for giant cell arteritis. J Rheumatol 32:1279–1282
Ness T, Bley TA, Schmidt WA, Lamprecht P (2013) The diagnosis and treatment of giant cell arteritis. Dtsch Arztebl Int 110:376–385, quiz 386
Zenone T, Puget M (2013) Characteristics of cerebrovascular accidents at time of diagnosis in a series of 98 patients with giant cell arteritis. Rheumatol Int 33:3017–3023
Bley TA, Wieben O, Uhl M, Thiel J, Schmidt D, Langer M (2005) High-resolution MRI in giant cell arteritis: imaging of the wall of the superficial temporal artery. AJR Am J Roentgenol 184:283–287
Bley TA, Weiben O, Uhl M et al (2005) Assessment of the cranial involvement pattern of giant cell arteritis with 3T magnetic resonance imaging. Arthritis Rheum 52:2470–2477
Bley TA, Wieben O, Uhl M et al (2005) Integrated head-thoracic vascular MRI at 3 T: assessment of cranial, cervical and thoracic involvement of giant cell arteritis. MAGMA 18:193–200
Klink T, Geiger J, Both M et al (2014) Giant cell arteritis: diagnostic accuracy of MR imaging of superficial cranial arteries in initial diagnosis-results from a multicenter trial. Radiology 273:844–852
Achkar AA, Lie JT, Hunder GG, O’Fallon WM, Gabriel SE (1994) How does previous corticosteroid treatment affect the biopsy findings in giant cell (temporal) arteritis? Ann Intern Med 120:987–992
Bley TA, Ness T, Warnatz K et al (2007) Influence of corticosteroid treatment on MRI findings in giant cell arteritis. Clin Rheumatol 26:1541–1543
Bley TA, Markl M, Schelp M et al (2008) Mural inflammatory hyperenhancement in MRI of giant cell (temporal) arteritis resolves under corticosteroid treatment. Rheumatology (Oxford) 47:65–67
Hauenstein C, Reinhard M, Geiger J et al (2012) Effects of early corticosteroid treatment on magnetic resonance imaging and ultrasonography findings in giant cell arteritis. Rheumatology 51:1999–2003
Choi YJ, Jung SC, Lee DH (2012) Vessel wall imaging of the intracranial and cervical carotid arteries. J Stroke 17:238–255
Küker W (2007) Cerebral vasculitis: imaging signs revisited. Neuroradiology 49:471–479
Fischer A, Maderwald S, Johst S et al (2014) Initial evaluation of non-contrast-enhanced magnetic resonance angiography in patients with peripheral arterial occlusive disease at 7 T. Investig Radiol 49:331–338
Wrede KH, Dammann P, Monninghoff C et al (2014) Non-Enhanced MR imaging of cerebral aneurysms: 7 Tesla versus 1.5 Tesla. PLoS One 9(1):e84562
Geiger J, Bley T, Uhl M, Frydrychowicz A, Langer M, Markl M (2010) Diagnostic value of T2-weighted imaging for the detection of superficial cranial artery inflammation in giant cell arteritis. J Magn Reson Imaging 31:470–474
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Dr. Bley receives ongoing research support from the “Deutsche Forschungsgemeinschaft, DFG” for MRI research.
Conflict of interest
Dr. Bley had past consulting activities for HeartFlow, GSK, and MSD, and received past payments for lectures from Bayer, Bracco, HeartFlow, Guerbet, and Siemens. Beyond this, all authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge, or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Goll, C., Thormann, M., Hofmüller, W. et al. Feasibility study: 7 T MRI in giant cell arteritis. Graefes Arch Clin Exp Ophthalmol 254, 1111–1116 (2016). https://doi.org/10.1007/s00417-016-3337-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-016-3337-7