Abstract
Purpose
To develop a modeling framework that simulates clinical endpoints (objective response rate and progression-free survival) to support development of motesanib. The framework was evaluated using results from a phase 2 study of motesanib in thyroid cancer.
Methods
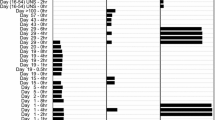
Models of probability and duration of dose modifications and overall survival were developed using data from 93 patients with differentiated thyroid cancer and 91 patients with medullary thyroid cancer, who received motesanib 125 mg once daily. The models, combined with previously developed population pharmacokinetic and tumor growth inhibition models, were assessed in predicting dose intensity, tumor size over time, objective response rate, and progression-free survival. Dose–response simulations were performed in patients with differentiated thyroid cancer.
Results
The predicted objective response rate and median progression-free survival in patients with differentiated thyroid cancer was 15.0% (95% prediction interval, 7.5%–23.7%) and 40 weeks (95% prediction interval, 32–49 weeks), respectively, compared with the observed objective response rate of 14.0% and median progression-free survival of 40 weeks. The simulated median objective response rate increased with motesanib starting dose from 13.5% at 100 mg once daily to 38.0% at 250 mg once daily. However, simulated median progression-free survival was independent of starting dose, ranging from 40.5 weeks (95% prediction interval, 38.6–46.9 weeks) at 100 mg once daily to 40.0 weeks (95% prediction interval, 38.6–46.8 weeks) at 250 mg once daily.
Conclusions
Dose–response simulations confirmed the appropriateness of 125-mg once-daily dosing; no clinically relevant improvement in progression-free survival would be obtained by dose intensification. This modeling framework represents an important tool to simulate clinical response and support clinical development decisions.




Similar content being viewed by others
References
Ratain MJ, Humphrey RW, Gordon GB, Fyfe G, Adamson PC, Fleming TR, Stadler WM, Berry DA, Peck CC (2008) Recommended changes to oncology clinical trial design: revolution or evolution? Eur J Cancer 44:8–11
Leff R, Andrews M (2008) Predicting success in phase III studies from phase II results: a new paradigm is needed. J Clin Oncol 26:3653–3654 author reply 3654–3655
Bruno R, Claret L (2009) On the use of change in tumor size to predict survival in clinical oncology studies: toward a new paradigm to design and evaluate phase II studies. Clin Pharmacol Ther 86:136–138
Guidance for industry end-of-phase 2A meetings (2009) United States food and drug administration. Available at: http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/ucm079690.pdf. Accessed Aug 24 2009
Claret L, Girard P, O’Shaughnessy J, Hoff P, Van Cutsem E, Blum J, Zuideveld K, Jorga K, Fagerberg J, Bruno R (2006) Model-based predictions of expected anti-tumor response and survival in phase III studies based on phase II data of an investigational agent [abstract]. J Clin Oncol 24:6025
Claret L, Girard P, Hoff PM, Van Cutsem E, Zuideveld KP, Jorga K, Fagerberg J, Bruno R (2009) Model-based prediction of phase III overall survival in colorectal cancer on the basis of phase II tumor dynamics. J Clin Oncol 27:4103–4108
Wang Y, Sung C, Dartois C, Ramchandani R, Booth BP, Rock E, Gobburu J (2009) Elucidation of relationship between tumor size and survival in non-small-cell lung cancer patients can aid early decision making in clinical drug development. Clin Pharmacol Ther 86:167–174
Polverino A, Coxon A, Starnes C, Diaz Z, DeMelfi T, Wang L, Bready J, Estrada J, Cattley R, Kaufman S, Chen D, Gan Y, Kumar G, Meyer J, Neervannan S, Alva G, Talvenheimo J, Montestruque S, Tasker A, Patel V, Radinsky R, Kendall R (2006) AMG 706, an oral, multikinase inhibitor that selectively targets vascular endothelial growth factor, platelet-derived growth factor, and kit receptors, potently inhibits angiogenesis and induces regression in tumor xenografts. Cancer Res 66:8715–8721
Rosen LS, Kurzrock R, Mulay M, Van Vugt A, Purdom M, Ng C, Silverman J, Koutsoukos A, Sun YN, Bass MB, Xu RY, Polverino A, Wiezorek JS, Chang DD, Benjamin R, Herbst RS (2007) Safety, pharmacokinetics, and efficacy of AMG 706, an oral multikinase inhibitor, in patients with advanced solid tumors. J Clin Oncol 25:2369–2376
Price TJ, Lipton L, McGreivy J, McCoy S, Sun YN, Rosenthal MA (2008) Safety and pharmacokinetics of motesanib in combination with gemcitabine for the treatment of patients with solid tumours. Br J Cancer 99:1387–1394
Tebbutt N, Burris H, Hurwitz H, Stephenson J, Kotasek D, Goldstein D, Sikorski R, Sun Y, McCoy S, Schwartzberg L (2008) Safety and pharmacokinetics (PK) of motesanib diphosphate with or without panitumumab (pmab) plus FOLFIRI or FOLFOX for the treatment of metastatic colorectal cancer (mCRC) [abstract 468PD]. Ann Oncol 19 (suppl): viii155–156
Sherman SI, Wirth LJ, Droz JP, Hofmann M, Bastholt L, Martins RG, Licitra L, Eschenberg MJ, Sun YN, Juan T, Stepan DE, Schlumberger MJ (2008) Motesanib diphosphate in progressive differentiated thyroid cancer. N Engl J Med 359:31–42
Schlumberger MJ, Elisei R, Bastholt L, Wirth LJ, Martins RG, Locati LD, Jarzab B, Pacini F, Daumerie C, Droz JP, Eschenberg MJ, Sun YN, Juan T, Stepan DE, Sherman SI (2009) Phase II study of safety and efficacy of motesanib in patients with progressive or symptomatic, advanced or metastatic medullary thyroid cancer. J Clin Oncol 27:3794–3801
Lu J-F, Claret L, Sutjandra L, Kuchimanchi M, Melara R, Bruno R, Sun Y-N (2010) Population pharmacokinetic/pharmacodynamic modeling for the time course of tumor shrinkage by motesanib in thyroid cancer patients. Cancer Chemother Pharmacol. doi:10.1007/s00280-010-1456-0 (this issue)
Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L, Verweij J, Van Glabbeke M, van Oosterom AT, Christian MC, Gwyther SG (2000) New guidelines to evaluate the response to treatment in solid tumors. European organization for research and treatment of cancer, national cancer institute of the United States, national cancer institute of Canada. J Natl Cancer Inst 92:205–216
Gabrielsson J, Weiner D (2007) Pharmacokinetic and pharmacodynamic data analysis: concepts and applications. Swedish Pharmaceutical Press, Stockholm
Beal SL, Sheiner LB (1998) NONMEM user’s guide–part VII. Conditional estimation methods. NONMEM project group, University of California, San Francisco
Meeker WQ, Duke SD (1981) CENSOR–a user oriented computer program for life data analysis. Am Stat 35:112
Claret L, Stark FS, Sirzen F, Gieschke R, Bruno R (2008) A modeling framework to simulate Xeloda dose intensity and survival in colorectal cancer [abstract 1312]. Presented at: annual meeting of the population approach group in Europe. June 18–20. Marseille, France
Acknowledgments
The authors wish to thank Benjamin Scott, PhD (Complete Healthcare Communications, Inc., Chadds Ford, PA), whose work was funded by Amgen Inc., for editorial assistance in the preparation of this manuscript.
Conflict of interest
LC and RB are employees of Pharsight and contractors to Amgen Inc. J-FL, and Y-NS are employees of and stockholders in Amgen Inc.
Author information
Authors and Affiliations
Corresponding author
Additional information
L. Claret and J.-F. Lu contributed equally to this manuscript.
Appendix
Appendix

Rights and permissions
About this article
Cite this article
Claret, L., Lu, JF., Sun, YN. et al. Development of a modeling framework to simulate efficacy endpoints for motesanib in patients with thyroid cancer. Cancer Chemother Pharmacol 66, 1141–1149 (2010). https://doi.org/10.1007/s00280-010-1449-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-010-1449-z